Both types belong to the family Vibrionaceae whose general characteristics have been described in the previous chapter.
THE GENDER AEROMONAS
The pathogenicity of these bacteria in the family Vibrionaceae has long been underestimated. Infections are mostly waterborne.
Aeromonas are Gram-negative bacilli, aero-anaerobic with a oxidase ferment glucose with or without gas, reducing nitrate to nitrite, mobile or immobile by polar cilia, 0/129 resistant compound.
HISTORY:
Of Aeromonas strains have been described as early as 1890, but the name à’Aeromonas proposed by Kluyver and Van Niel in 1936, was admitted to the Bergey’s manual in 1959.
I – CLASSIFICATION:

Aeromonas species have long been confused withProteus, Pseudomonas or Vibrio.
Aeromonas (GC% between 57 and 63) are currently classified in the family Vibrionaceae, next genera Vibrioand Plesiomonas Some authors propose to fit them into a new family. Aeromonadaceae them.
The genus Aeromonas consists of several mobile and immobile species, the main are:
– Mobile species:
A. hydrophila (type species)
A. caviae
A. veronii (biogroups veronii and sobria)
A. jandaei
A. schubertii
A. eucrenophila
– Immobile species:
A. salmonicida (ssp., Salmonicida achromogenes, masoucida, smithid)
A. Media
II – PATHOPHYSIOLOGY:
Aeromonas infections are often associated with waterborne contamination. Germs usually enter the body after a break, thanks to trauma or through the digestive tract through thy mucosal lesion.
Infections often affect immunocompromised. The table may be that of endotoxin shock, or the events are related to toxins produced by the bacteria.
III – HABITAT:
Aeromonas are isolated frequently in gifted waters (freshwater bacteria) in standing water, running water, drinking water, water from sea or lagoons receiving the gifted water and sewage (concentration> • 10 ml). These are characteristics of surface bacteria.
They can multiply in water talented depending on temperature, pH and nutrient content, they would be good indicators of the trophic status of these waters.
Their presence is signaled in various foods (oysters, mussels, shellfish in particular) and in soils.
Through research using selective media, it has been shown the existence of intestinal carriage in animals or humans. In the latter respect porting 1-3% of patients in Europe or the United States, and up to 8-16% of children and 27% of adults in exotic countries like Thailand.
IV – PATHOGENICITY:
1. For cold-blooded animals (fish, reptiles and amphibians):
Aeromonas cause hemorrhagic syndromes; they are sometimes responsible for epidemics harmful to fish (trout). A.salmonicida is responsible for furunculosis of salmonids.
2. In men:
Infections are most often waterborne, deep wound after swimming in a river, immersion, drowning … or consecutive to the ingestion of contaminated food.
It is recognized:
a / Skin infections:
They are kind of cellulitis or secondary infections of wounds, burns and consecutive to a contact with water or soil.The (rare) cases of gas gangrene have been described and are a therapeutic trap.
b / More or less acute diarrhea:
They can evoke choleriform syndromes, with watery stools, not slimy and not bloody. These diarrhea are found in all parts of the world especially in the tropics (travelers and young children are often affected), but also in the temperate zone (1% of stools in Strasbourg during systematic studies), especially in hot weather.
The enteropathogenic power has long been controversial because only 5% of volunteers ingesting 5.1010Aeromonas showed gastrointestinal symptoms in some studies. Consider now that Aeromonas hydrophila, A. sobria and A. caviae can behave like true intestinal pathogens.
c / The septicemia:
They are often associated with liver disease (cirrhosis), biliary, pancreatic or hematological malignancies including.But these septicemia may also occur in patients with normal immune systems. The origin is usually digestive, especially during cancer chemotherapy.
In some cases, sepsis is associated with skin lesions such ecthyma gangrenosum. The mortality in sepsis is about 50%.
d / Other infections can be observed:
These lung infections after drowning, rarely urinary tract infections, peritonitis, meningitis infections, ear infections, endocarditis, eye infections.
Infections are either Monomicrobial or mixed, especially in diarrhea.
Patients with hepatobiliary disorders are more prone than others to Aeromonas infections. The laying of leeches has been the source of some infections Aeromonas.
V – BACTERIOLOGICAL CHARACTERS:
A – Body type:
Aeromonas are Gram-negative bacilli 1-4 pm / 0.6 prn, movable polar cilia usually monotriches or immobile (A.salmonicida). They can take a look coccobacillary or short chains.
B – Cropping characters:
These are aero-anaerobes.
The optimum pH is 7 (cultivation between 5.2 and 9.8) and the optimal temperature is generally 30 ° C. It is actually varies by species, A. salmonicida did not grow at 37 ° C.
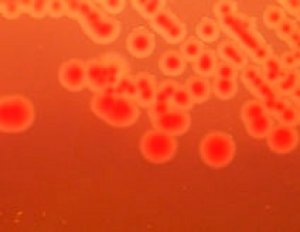
In 24 hours on solid medium, obtained colonies 1 to 3 mm translucent resembling enterobacteria. Culture is possible circles type or trypticase soy blood agar, but also circles “selective” MacConkey, EMB or Drigalski (colonies unevenly ferment lactose).
The SS medium is very inhibitor for Aeromonas, colonies are thin and appear only 48 hours.
C – biochemical characters:
These bacteria are oxidase (+) and reduced nitrates to nitrites.
Some characters are common to different species:
– Fermentation of glucose, sucrose (except A. jandaei and schubertii), maltose, trehalose, mannitol (except A.schubertii) Character ONPG (+)..
– Possession of DNase, gelatinase, indole production. ODC character (-) (except A. veronii veronii)
– Resistance vibriostatic composed 0/129
The diagnosis of the most common species based on the differential characteristics shown in Table I.
Search for decarboxylase in these species may pose some difficulties because of the difference in sensitivity of the reaction media. The middle of Fay and Barry (Appl. Microbiol. 1972, 23, 710-713) would be more suitable for this research (30 ° C, 24 h) than the middle of Moeller.
D – Substances produced, virulence factors and pathophysiological hypotheses:
Pigment: A. salmonicida and A. hydrophila give brownish or dark green colonies after 2 to 5 days of incubation.These species synthesize a pigment melanin from tyrosine and phenylalanine.
Virulence factors identified in Aeromonas are many outside enzymes promoting infection: proteases, elastase, DNase, phospholipase, lipase, they exhibit adhesion capacity and produce a variety of toxins.
– The ability of adhesion, which is the first step before the colonization of the intestinal mucosa has been shown using HEp-2 cells (study model for the pathogenesis of infections with E. coli, Salmonella, Campylobacter) .
There are two types of pili: pili-L (long pili, thin, flexible, polypeptide 4 kDa) and pili-S (short, thick, polypeptide of 17 kDa). The adhesive strength is related to the presence of L-pili involved in pathogenicity, environmental strains are poorly adherent and exhibit S-pili.
– The enterotoxigenic strains produce specific lectins sialic acid to the colonization of the intestinal surfaces. There are enteroinvasive strains of A. Sobria and A. hydrophila (except environmental strains).
– Toxins of several types. Firstly we distinguish the hemolysin or cytotoxins and enterotoxins or cytotonines.
There are two hemolysins:
– An alpha-hemolysin (65 kDa) produced not beyond 30 ° C
– A beta-hemolysin (50 kDa) produced in greater amount at 37 ° C also known as aerolysin or ASAO-hemolysin.Heat-labile, it is cytotoxic to many cell lines and a product water accumulation in isolated ileal loop; it would be the main virulence factor involved in diarrhea.
The nature of Aeromonas enterotoxins was the subject of much controversy. Have been described:
– A cholera-like enterotoxin (63 kDa) neutralized by an anti-cholera toxin serum produced by 5 to 10% of the strains of A. hydrophila This cytotonic toxin (Yl cells) immunological communities with cholera toxin and stimulates production cAMP.
– Cytolytic enterotoxin (52 kDa) which reacts with the antitoxin cholera but is not neutralized; its cytolytic and haemolytic activities are correlated and its N-terminal sequence is identical to that of aerolysin.
– A cytotonic enterotoxin (15 kDa) relatively stable to the heat produced by most strains of A. hydrophila and A. sobria and about 10% of A. caviae, active on the newborn mouse intestine…
– Enterotoxin cytotonic and cytotoxic (50 kDa) thermostable unneutralized by anti-cholera toxin serum and verotoxic produced by half of A. sobria and A. hydrophila strain..
The study of. these toxins has been difficult, it now seems (although this is not yet firmly established) the cytotoniques enterotoxin and cholera-like enterotoxins are genetically very similar, and similarly, the cytolytic enterotoxin and beta hemolysin are also nearby. Only differences in expression in vivo or in vitro modify toxinogenesis resulting in a variation of the enterotoxigenic or cytotoxic activity according to the type of target tissue.
Some mobile Aeromonas strains (A. hydrophila, A. sobria, A. caviae) grown in broth containing 0.5% glucose shows an inhibition of the subsequent growth in the accumulation of fatty acid and acetate causing Suppression of the Krebs cycle. This “phenomenon suicide” is correlated with the growth temperature and it has been shown that only the non-virulent strains were suicide and enteric. This suicide phenomenon was closer to the presence of protein antigens thermostable area making autoagglutinables strains resistant to acetic acid, and considered the most virulent.
The study of the pathophysiology of Aeromonas infections is complex: the entéropathogénicité strains of Aeromonas is due to the simultaneous action of several physiological, metabolic, antigenic and toxic. The presenceof Aeromonas in a stool culture does not necessarily mean that it enteropathogenic, as the strain is suicide or not, it will implant according as it will entéroadhérente or enteroinvasive or that it will produce a cholera-like toxin or cytolytic be observed is a minor intestinal infection, more serious or chronic.
E – antigenic structures:
Aeromonas all possess antigens 0. mobile species further antigens H.
Agglutination techniques or indirect hemagglutination were used to attempt serotyping of Aeromonas.
If the species A. salmonicida seems antigenically homogeneous, considerable heterogeneity was observed in the other species. In addition, a significant number of strains present a spontaneous agglutination. Strains of group A 0:11. Hydrophila are autoagglutinables and are involved in more than 50% of sepsis and wound infections.
There are cross-reactions between different species of Aeromonas between P. shigelloides and A. hydrophila or A.sobria.
F – Phage:
A provisional scheme was proposed by phage Popoff. Note that there is an active phage on all strains of A.salmonicida, which may be of interest for diagnosis.
VI – BACTERIOLOGICAL DIAGNOSIS:
A – pathological products:
Isolates, apart from systematic research are often the result of chance. The main pathological products are: blood culture, pus, urine, CSF, puncture liquid stools …
Searches can be performed on the water or food.
B – Isolation:
Isolation can be easily obtained on non-selective media (trypticase soy blood agar) if the product is pathological monomicrobien. For polymicrobial samples, for against, one should use selective media, especially the stool.Various solid isolation media have been recommended: dextrin agar-fuchsin; xylose deoxycholate sodium-citrate;MacConkey trehalose in place of lactose; inositol agar – bright green – bile salts (BWI); Starch Agar – glutamate – ampicillin – penicillin (SGAP – 10 C) for samples of polluted water. Note that the TCBS is not sufficiently selective.
In fact, for a stool, one can simply use a trypticase agar – soy sheep blood (5%) containing ampicillin (20 mg / 1) or CIN agar: cefsulodine (4 mg / 1) irgasan – novobiocin. Selective enrichment liquid media (alkaline peptone water pH 8.6 and ampicillin, for example) do not relevant since there is no correlation with the clinical.
The main differential diagnoses arise with Vibrions the Plesiomonas and Pseudomonas. The fermentation of sugars, oxidase character (+) and resistance to 0/129 guide the diagnosis. The main differential type are the gas production medium containing glucose, hydrolysis of esculin, the fermentation of arabinose, VP and ONPG.
VII – ANTIBIOTIC SENSITIVITY:
Aeromonas are sensitive to tetracyclines, chloramphenicol, aminoglycosides and trimethoprim-sulfamethoxazole.Vis-à-vis behavior colistin varies strains (MIC 1 to over 64 mg / 1).
Among the beta-lactam resistance is regularly observed to ampicillin but also to carbenicillin, ticarcillin or piperacillin. TO.
hydrophila and A. caviae are also resistant to cephalothin but A. sobria is relatively sensitive. By against the latamoxef and 3rd generation cephalosporins (cefotaxime, ceftriaxone) are constantly active. But some strains of Aeromonas sp. may have more than 2 inducible beta-lactamase conferring resistance to a wider third-generation cephalosporins, aztreonam and imipenem.
These germs are also sensitive to nalidixic acid and very sensitive to fluoroquinolones. The septicemic forms often require a third-generation cephalosporin or treatment with a fluoroquinolone with an aminoglycoside.
The treatment of diarrhea may require rehydration, but antibiotics are usually unnecessary.
THE GENDER Plesiomonas
It is only one species: P. shigelloides.
I – HABITAT AND PATHOGENICITY:
P. shigelloides is present in water (all year round in tropical or subtropical, summer or autumn in temperate zone) and in various animals. It is isolated from stool of diarrheal subjects especially in the tropics, occasionally in Europe.Pathophysiological hypotheses about these forms of diarrhea have been advanced. Invasiveness or enterotoxigenic not specified. There is no DNA sequence homologies with known genes encoding enterotoxins. However, we began to study some potential virulence factors (cytolysin or cytotoxin).
P. shigelloides is involved in infections in humans, fish, and probably other animals.
In humans there is sometimes predisposing factors: underlying diseases (cancer, cirrhosis), anti-acid treatment; and sources of contamination such as contact with water or sea talented, raw seafood intake or undercooked, or spoiled canned fish.
The fact that the ingestion of P. shigelloides by volunteers does not cause disease suggests that this species would pathogenicity in combination with another agent.
P. shigelloides was isolated from various tables:
– Gastroenteritis (the most common form) in children or adults preferably (opposite Aeromonas) is taking an aspect choleriform, more rarely dysentery appearance; cases can be isolated but can attend small epidemics, subacute and chronic forms can be observed, evolving from 14 days to 2 or 3 months.
– Extra-intestinal forms, rare. Cases of meningitis, septicemia, cellulitis, arthritis or ophthalmia have been reported.
II – BACTERIOLOGICAL DIAGNOSIS:
A – Morphological Character:
Motile by polar cilia usually lophotriche.
B – Cropping characters:
They grow well at 37 ° C, but they do not grow in broth with 6.5% NaCl. Culture on the classic usual media for enteric bacteria can be inhibited. The selective medium inositol – bright green – bile salts (BWI) can be used for stool cultures. In an authentic diarrhea germ will be in pure culture.
C – Identification characters:
Ferment glucose without producing gas.
Oxidase (+), common sensitivity to 0/129.
The ODC Plesiomonas are (+), LDC (+), ADH (+) and the main biochemical characteristics are reported in Table I.
Antigenic classification was proposed by Sakasaki with 107 serovars. Some groups 0 cross-react with the antigens of Shigella or â’Aeromonas.
IV – ANTIBIOTIC SENSITIVITY:
P. shigelloides is frequently resistant to amino-, carboxy- and ureido-penicillins, but is susceptible to other antibiotics (imipenem, aztreonam …). Many strains produce penicillinase encoded by a plasmid, beta-lactamase inhibitors (sulbactam, clavulanic acid, tazobactam) restore the activity of beta-lactam antibiotics. P. shigelloides is usually resistant to aminoglycosides, netilmicin remaining active.
Gastroenteritis in the most commonly used treatments are based tetracyclines, trimethoprim-sulfamethoxazole or fluoroquinolones (ciprofloxacin).

You must be logged in to post a comment.