Known as the agent of gas gangrene or postpartum sepsis, Clostridium perfringens is currently isolated in food poisoning of tissue or systemic infections.

HISTORY:
Isolated for the first time in 1881, this germ has seen its role in gas gangrene recognized by Welch and Nuttall Frankel and in acute appendicitis by Veillon.
The study of toxic factors and differentiation of types ofClostridium back to the 1950s; Hobbs in 1953 demonstrates the existence of an enterotoxin.
I – CLASSIFICATION:
In the 4 groups of Clostridium perfringens C. is in Group III saccharolytic, no or low proteolytic.
It differs from other Clostridium immobility and the presence of a capsule. The species C. perfringens is divided into five subtypes toxin designated by letters A to E.
Type A is mainly encountered in human pathology; other types of leaders are enterotoxaemia endogenously in animals (sheeps, cattle), rarely of human infections.
II – HABITAT – TRANSMISSION – PATHOPHYSIOLOGY:
C. perfringens is present in the intestinal flora of humans and many animal species. Among Clostridium species in the intestine, C. perfringens happens in order of frequency second only C. ramosum.
The soil contains spores of C. perfringens. The presence of this species or its spores in water or food is in favor of faecal contamination.
Humans are contaminated:
-either from an endogenous source (intestine, vagina …) on the occasion of a break or surgery,
– Either from an exogenous source in favor:
– A wound, the seed penetrates then multiplies in tissues where it releases toxins and enzymes,
– Ingestion of 108-109 germs in contaminated food, which can cause food poisoning (roughly between 30 and 80% of the carcasses are contaminated with C. perfringens, the meat is considered to be contaminated if it contains more than 106 live bacteria / gram). A first cooking preserves the spores; the food is cooled to room temperature and served cold or slightly heated, which causes reactivation of the spore. The symptoms are related to the release of enterotoxin from lysed bacteria in the gut.
III – PATHOGENICITY:
A – Experimental:
Intramuscular injection of a culture of C. perfringens guinea pigs causes diffuse inflammation, gaseous, with hemolysis, myolysis and died in 24 hours.
B – Natural:
Different clinical presentations can be observed:
1. Tissue Infections:
a / localized infection of skin and soft tissue (subcutaneous tissue) infections progressing slowly and often indolent such as foot ulcers, decubitus …
b / Cellulite diffuse etfasciites:
All the superficial layers of the skin are affected include abscesses and gas formation. In the absence of treatment there is a rapid expansion of fasciitis and shock.
c / myonecrosis and gas gangrene
– Post-traumatic or post-surgical occurring between 8 am and 20 days after the initial event. The beginning is manifested by a sudden pain, a purplish wound, hemorrhagic bullae, crepitus, runny sérohématique nauseous …
– After nontraumatic intestinal perforation (eg neoplasia)
– After normal delivery or sometimes septic abortion occurs post-abortion sepsis (or postpartum) with gas gangrene uterus with intense jaundice, hemolysis, acute renal failure.
One can also find C. perfringens in various pus, abdominal abscess, lung abscess, pleural, peritoneal liquid, with or without local or general signs.
Note that in some samples C. perfringens is not alone, but willingly associated with other anaerobic and / or facultative aerobic-anaerobic bacteria.
2. Digestive disorders:
a / food poisoning:
Symptoms begin 8-12 hours after eating infecting (including meat) with abdominal cramps and diarrhea, nausea, fever, vomiting rarely. Disorders diminish within 24 hours.
Type A is involved in these collective food poisoning.
The etiology is the cause of 15% of food poisoning although the incidence of true food poisoning C. perfringens is probably underestimated in France.
b / necrotizing enteritis:
This rare poisoning has been reported in Germany under the name “Darmbrand” and New Guinea as that of “pig-bel.”
This is a condition involving bloody diarrhea and spontaneous gangrene of the small intestine with a poor prognosis.
A beta toxin produced by C. perfrmgens type C is normally rapidly degraded by proteolytic enzymes in the intestine or degradation would be inhibited in cases of malnutrition or by certain foods inhibiting trypsin (endowed potatoes).
3. sepsis and bacteremia:
The classic table was represented by the post-abortion sepsis, characterized by hemolytic jaundice and severe renal impairment. The prognosis of this infection, uterine starting point was particularly bleak. This disease has virtually disappeared in our region since the law on abortion. It does not have to neglect this possibility and discuss in developing countries.
Simple bacteremia C. perfringens meet today in hospitalized patients and having the most diverse pathologies. One positive blood culture is discussed based on clinical data.
IV – BACTERIOLOGICAL CHARACTERS:
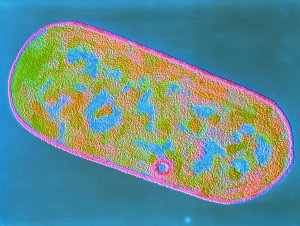
A – Morphology of the vegetative form:
– Gram-positive bacilli, stubby parallel edges and square pieces of about 1 um 3-4 u, m, motionless. Singly or in short chains; depending on the stage of growth, one can observe filamentous forms at the beginning or spheroplasts in aged cultures. The preparation, the bacterial bodies irregularly keep the dyes.
– A capsule is observed in pathological products.
B – Spore and sporulation:
– Typical clostridial spores are deforming subterminal.
– The sporulation is obtained only in complex environments (Ellner environments, SEC, DS: Duncan and Strong)
– Can be distinguished based on two types of thermotolerance spore:
– Thermosensitive destroyed at 100 ° C in 5 seconds: myonecrosis strains
– Heat resistant destroyed at 100 ° C in 60 minutes, strains of food poisoning. Enterotoxin production occurs during sporulation (presence of inclusion paracrystalline).
C – Culture:
– Strict anaerobic bacteria, but relatively tolerant to oxygen. If she can grow up to 44 ° C, the optimum temperature is 37 ° C and the optimum pH is 6.6 to 7 (tolerance of 5 to 9).
Rapid growth is obtained on media containing amino acids, vitamins, carbohydrates.
– In deep agar lenticular colonies is observed, with significant gas formation.
– On the surface, convex colonies, round (3-4 mm) in 24 hours, whitish, sometimes rhizoid board.
– On blood agar, a large area of hemolysis is observed for the toxigenic strains, but the diameter varies between strains. The type A provides complete haemolysis (hemolysin theta) around the colony, hemolysis can be inhibited by anti-A serum perfringens and incomplete hemolysis zone related to alpha-toxin (phospholipase C) especially visible after stay 4 ° C and has a synergistic effect with the CAMP factor of S. agalactiae (97% of strains).
D – biochemical characters:
– The proteolysis is low gelatin liquefaction in 24-48 hours, rapid clotting cysteinated milk (acidification, clot retraction), H2S (+), indole (-), urease (-).
– Carbohydrates are fermented with gas: glucose, lactose, sucrose, maltose. The products of the fermentation the glucose terminals (gas chromatography) are butyric and acetic acids and a small amount of propionic acid.
– Phospholipase C is demonstrated on an agar with egg as opalescence around the colonies, inhibited by an anti-Aserum perfringens (test Nagler). This character is generally positive for all strains.
– Lack of lipase agar with egg or tributyrin.
E – Toxins and other substances produced:
Diffférents components have been identified:
1.-lethal necrotizing toxins (Table I):
a / alpha toxin, hemolytic:
II are:
– A phospholipase C found in all types ABCDE
– An exotoxin produced during the exponential phase
– A 43 kDa protein, whose synthesis is promoted by iron, fructose, certain amino acids …
It acts:
– By destroying the membranes of the red blood cells (haemolysis), platelet hence coagulation disorders.
– Causing inactivation of muscle ATPase.
It causes myonecrosis (type A).
b / Toxin beta (40 kDa) non-hemolytic which mainly has a pathogenicity in animals (types B and C); more rarely in humans.
c / epsilon toxin (34 kDa) non-hemolytic, synthesized as protoxin. It is activated by trypsin; it causes necrosis sub-endocarditiques and renal parenchyma (Types B and D)
d / iota toxin (120 kDa) non-hemolytic, activated by proteases; increases vascular permeability, especially in animals (type E).
2. enterotoxin:
The enterotoxin is produced by type A strains, responsible for food poisoning. This heat-labile toxin (35 kDa) occurred during sporulation, the gene was cloned and its sequence is known.
The enterotoxin is released after lysis of the bacteria spore within the intestine; it binds to epithelial cells at the level of receptors (ileum). Toxin induces an increase in intracellular Ca + and by an alteration of membrane permeability causes a loss of fluid, ions and small molecules by intestinal cells.
3. Enzymatic Factors “non-toxic” (Table II):
F – Antigens:
There are about 50 serotypes for food poisoning strains, strains causing myonecrosis are generally not typable.
Serotyping is mostly interesting in the epidemiological studies (comparison of intestinal stem and stem found in foods during food poisoning).
V – BACTERIOLOGICAL DIAGNOSIS:
A – Isolation of C. perfringens:
1. Samples:
– Blood culture under anaerobic conditions.
– Pus which often have a putrid odor. Is removed using a syringe which is removed and the air that is mouth or using transport medium containing a reducing agent.
– Anatomical Pieces: Appendix myonecrosis … transport as the cultivation should, as with pus, be achieved quickly.
– In the context of food poisoning research and germ count in the stool are useful for diagnosis. It is desirable to have all suspect foods. Bacteriological criteria can confirm the foodborne poisoning are: a bacterial count> 105 / g of food, a spore count> 106 / g of feces, isolation of the same serotype in patients, the detection of enterotoxin in the stool (counterimmunoelectrophoresis, latex test, Elisa).
2. Direct examination:
This examination is always essential on pus or internal fluids.
The observation of bacteria with morphology of Clostridium allows to implement without delay appropriate antibiotic therapy, it is indeed an emergency that can not wait, in many cases, the results of the culture.
3. Crops:
They are carried out
– Either in liquid medium for anaerobic or previously regenerated with gear such as thioglycollate medium or broth VF, TGY, PGY, middle Rosenow,
– Either in solid medium, blood agar, possibly rendered selective by the addition of neomycin (0.1%). Solid media are placed in an anaerobic jar, unless all the manipulations will be carried out in an anaerobic chamber.
The C. perfringens are actually quite strong, even in the presence of oxygen.
Their culture is easy anaerobically producing gas.
On blood agar, there is a characteristic double hemolysis halo.
4. Identification:
The motionless character of Clostridium may already towards C. perfringens.
Definitive diagnosis is based species:
– On the fermentation of lactose and sucrose
– On the search for a Lecithinase, and inhibition of this enzyme activity with an anti-serum perfringens A (test Nagler, Willis).
The elements of the differential diagnosis included in the introductory chapter Clostridium table (Table I).
In a blood culture bottle, the diagnosis of C. perfringens should be considered immediately before the character very gasifier, hemolysis of the blood and the visualization of large Gram-positive bacilli; this finding should lead to immediate information sepsis is suspected C. perfringens.
B – The direct evidence enterotoxin:
It is carried in the feces or food in a context of food poisoning; various techniques are proposed: sensitized latex particles, electro-syneresis, ELISA techniques. Synthesis of an oligonucleotide probe for detection of the enterotoxin gene has been used.
VI – TREATMENT:
A – Prophylaxis:
– All wounds should always be disinfected with powerful antiseptic. We must proceed with the removal of all foreign material and careful debridement of wounds.
– Antibiotic prophylaxis is used in visceral surgery (combining a beta-lactam and metronidazole). If dirty surgery, rupture of viscera, traumatic wounds, antibiotic therapy will be extended; it will be the same for amputations in ischemic or open fractures views late.
B – Curative treatment:
The treatment of tissue and systemic infections is based on the use of penicillin G (10-50000000 units / day), or ampicillin. Some cephalosporins are sometimes less active.
Plasmid resistance was observed for tetracycline, chloramphenicol, macrolides and lincosamides.
Serum therapy is discontinued. Hyperbaric oxygenation chamber in specialized centers is an additional therapeutic option. The surgery takes first place in the treatment of gas gangrene and requires the removal of necrotic tissue.
The prognosis remains formidable, and in a French multicenter study it was noted 34% of deaths directly related to gangrene and 10% of deaths from other causes. Mortality was very similar in the cellulitis and myonecrosis.
The prognosis is darker in postoperative posttraumatic that gangrene.
Digestive infections usually require only symptomatic therapy, rather, they require effective prophylaxis in the food chain.


You must be logged in to post a comment.