Clostridium tetani, formerly known as bacillus Nicolaier, is a gram-positive bacillus spore forming, anaerobic strict, which releases a neurotropic exotoxin entramant a formidable poisoning: tetanus. Despite the existence of an effective vaccine, tetanus is not a rare disease.

HISTORY:
Already described by Hippocrates, tetanus has been well studied by Larrey during the Napoleonic campaigns.
Nicolaier reproduced tetanus in 1884 by inoculating the earth at various animals and evokes a poison strychnine effect.
Kitasato in 1889 isolated the bacteria by using the heat-resistant property imparted by the spore and culturing anaerobically. The following year Knud Faber-demonstrates the existence of the toxin.
In 1923, Gaston Ramon discovered tetanus. Subsequently, many work continues on the pathophysiology, clinical and therapeutic, but still many unknowns and mortality of the disease remains high.
I – CLASSIFICATION:
In the 4 groups of Clostridium tetani C. contained in group IV, that is to say from non-proteolytic Clostridiumnot glucidolytiques.
The GC% of the strains is between 25 and 26.
II – HABITAT – TRANSMISSION:
C. tetani is in the soil where it persists indefinitely due to its spore. It is rare in non-residential areas and forests, the spore is most abundant in contaminated areas and we can talk about tétanigènes zones (North and East of France). In some areas, it was found that 40% of the soil samples contained C. tetani.
The germ is also present in the gut and in the faeces of humans and various animals (horses, cattle).
It can also be found in dust, water, or even in the hospital environment (plaster, talc, cotton …).
The germ may enter the body:
A – Taking advantage of various injuries:
– Important: wounds contaminated with soil, with foreign bodies, deformities, possibly containing other anaerobic or anaérobiesaérobies associatioans,
– Minimal: bites, abrasions, splinters, bites …
– Chronic: ulcers, pressure sores, burns …
B – Taking advantage of an act that is not accompanied by a sufficient aseptic:
– Surgical: intervention in the intestine, open fracture,
– Medical: intramuscular injections performed with non-sterile equipment, possibly with predisposing products (quinine, anti-inflammatory, lactic acid …) bites among addicts
– Obstetrics: the umbilical neonatal tetanus remains common in developing countries.
Tetanus reached more fréquemmment the elderly, especially women, including booster shots are often forgotten (Figure 1).
depending on the age and sex (male * female •) and in comparison frequency of protected subjects (tetanus antibody levels above 0,025 IU HA) in Clermont Ferrand in 1975 in the local adult population foncûon of age and sex.
III – PATHOPHYSIOLOGY:
The infection begins with the introduction of C. spores tetani in the body through a skin cut. Then, under the influence of factors lowering the redox potential (associated bacteria, certain medications), spores that are found in anaerobic conditions will germinate and give the bacterial form producing tetanus toxin in situ. C. tetani produces two exoproteins a hemolysin (tétanolysine) and a neurotoxin (tetanospasmin). The latter being solely responsible for the disease.
A – Propagation of the tetanus neurotoxin:
Produced at the wound “gateway” toxin wins the central nervous system where it accumulates using two ways:
– Hematogenous route, so the generalized tetanus descendant,
– Nerve retrograde is tetanus ascendant.
The toxin rises along the axons of alpha motor neurons (for neuroprobasie) in the following sense:
muscle nerve endings -> nerve trunk -> ventral roots -> gray matter of the anterior horns of the spinal cord.
This explains that in this form, the incubation period is inversely proportional to the distance which separates the entrance of the central nervous system.
B – Targets of the toxin:
Toxin having a molecular weight of 150 kDa, binds at certain lipids nerve (van Heyningen, 1959). Receptors are gangliosides GT1b (trisialo ganglioside) and GD1b (disialo ganglioside) containing in their formula
– Two galactose units,
– N-acetylgalactosamine,
– Two to three units of N-acetylneuraminic acid (sialic acid =). The latter structure is essential to the binding of the toxin.
When attached to its receptor, the toxin acts on its molecular target still unknown and causes spastic paralysis.
C – Mode of action:
Tetanus neurotoxin:
– Blocking the influx inhibitors acting on the alpha motor neurons and acting on presynaptic level,
– Inhibits the release of various mediators of the central nervous system, GABA, glycine …
– Causes an increased release of acetylcholine and decreased cholinesterase activity.
IV – PATHOGENICITY:
A – In animals:
The toxin is active in mammals, particularly in horses, mice, guinea pigs. The injection of the toxin intravenously causes widespread tetanus or descending, by IM ascending tetanus.
B – In men:
1. usual form: Acute generalized tetanus
The incubation has a variable duration of 3 to 30 days, but it is usually between 3 and 15 days. This incubation is usually silent and is not alerted by the front door that has, in many cases, no signs of local inflammation.
The wounds are traumatic in 2 cases of 3 and 1 in 5 cases are chronic type (eg, varicose ulcer). Most often the wounds are small and do not attract attention. One in ten, no door is found.
The inaugural symptom is trismus, contraction of the masseter blocking the opening of the mouth. Then the contractions become widespread, extending to the muscles of the face where the sardonic facies and the vertebral muscles, neck, trunk … The belly is “wooden” and members are affected (greater flexion, lower extension), the thoracolumbar spine widened, hence the opisthotonos.
Permanent contractures reinforce during paroxysms caused by various stimuli (noise, light, touch). The crises are very painful causing various postures (opisthotonos, orthotonos …), lung function may be affected.
It is a non febrile illness. The prognosis varies with the severity scores.
2. There are different clinical forms:
– Cephalic tetanus linked to a door entry face,
– Localized tetanus members,
– Specific forms:
– Post-abortion,
– Umbilical formidable in newborns in developing countries
– Post-injection prognosis.
It is important to emphasize that the disease is not immunizing.
in the normal subject during the excitement of the biceps (1), the sensorimotor reflex arc (2.3) tends to oppose the distension of the triceps. Releasing the triceps is provided by the inhibition of the reflex arc (4), botulism, neuromuscular junction is blocked (5) resulting in flaccid paralysis in tetanus, tetanus toxin prevents the inhibition of the reflex . The two antagonistic muscles by contracting cause contracture.
V – BACTERIOLOGICAL CHARACTERS:
A – morphological characters:
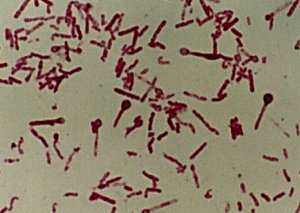
C. tetani is a gram positive bacillus but easily loses this character Dyer relatively long and thin (0.4 um x 4-8 pm). It has a terminal spore giving it a classically aspect pinhead. In culture, the long forms are not exceptional. The germ is a highly mobile peritrichous ciliature.
B – Cropping characters:
It is a strict anaerobic germs, having an optimum growth temperature of 37 ° C and an optimum pH of 7.4.
The appearance of the colonies, which appear in 48 hours, rhizoid is translucent; surface, colonies tend to swarm. It is therefore advantageous to use very dry boxes.
It is an undemanding germ that grows on all common media for anaerobic: agar, blood agar, bouillon broth … VF TGY an odor of burnt horn emerges linked to acrolein.
Hyperbaric oxygen kills 99.9% of cells.
The spores are destroyed by 20 minutes at 121 ° C in an autoclave.
C – biochemical characters:
Conventionally, C. sucking is little proteolytic. In Bergey’s Manual, 1986, this species is considered Gelatinolytic. It has peptidases and deaminase; there are irregular production of H2S and indole.
Carbohydrates are fermented (glucose (-), sucrose (-), lactose (-), esculin (-), starch (-)).
The fermentation end products are acetic acid, propionic acid, butyric acid, ethanol, propanol, butanol.
C. tetani has a DNase, but not lipase or lecithinase.
On blood agar there is a hemolysis around the colonies. It is due to a toxin, tétanolysine, oxygénolabile soluble hemolysin, which seem to play a pathogenic role but is antigenic. There may be another high molecular weight hemolysin.
From the viewpoint of biochemistry, C. tetani approximates C. Cochlearium and C. tetanomorphum but is distinguished by its pathogenicity and differences of DNA / DNA hybridization.
D – Tetanus toxin: tetanospasmin
C. tetani produces two exotoxins, responsible tetanospasmin symptoms of the disease and tétanolysine.
1. Production:
Excretion in the medium during the growth phase is partial. Most of the toxin remains inside the bacterium, which is liberated during the autolysis; toxin can represent up to 10% of the dry weight of the bacteria. The synthesis is favored by some amino acids (serine, glutamine peptides containing histidine).
Toxin production would not be linked to a state of lysogenic strains.
2. Properties:
The gene encoding the toxin is carried by a plasmid and fully sequenced. The stage endocellular, the toxin is a polypeptide of 150 kDa, when the excretion is cleaved by a protease into two fragments linked by a disulfide bridge
– A light chain of 50 kDa (L)
– A heavy chain of 100 kDa (H)
Each fragment in isolation is not toxic.
There is only one antigenic type.
3. Toxicity:
II is a potent toxin because 1 mg of toxin corresponds to 107 mouse LD50. The DMM mouse is 2 x 10-5 ug toxicity to the animal depends on the route of administration.
Toxin as it is by the Ramon flocculation test (flocculent Units) or by determining the minimum lethal dose in mice DMM 20 g or 350 g guinea pig, flocculent unit (UF) = 3000 DMM guinea pig = 10000 DMM mouse.
4. The anti-toxin antibodies:
They neutralize all the biological effects of the toxin. Can be obtained:
– Either from sensitized individuals,
– Either from hyperimmunized horses.
These antibodies do not cross the barrier hémoméningée.
5. Tetanus:
It is highly immunogenic in humans, horses and laboratory animals (rabbits, guinea pigs). It causes the formation of anti-toxin antibodies, neutralizing and precipitating. The immune response is enhanced through additives (Ca + phosphate, aluminum hydroxide).
The toxin may be detoxified and toxoided by formaldehyde (0.5%) at 40 ° C for one week. Tetanus keeps intact the immunogenicity of the toxin. This transformation is related to the blocking of lysyl residues of the molecule through the formation of stable methylene links.
E – The tétanolysine:
C. tetani produces a hemolysin, the tétanolysine sensitive oxygen; it is operatively and serologically related to streptolysin 0 and the hemolysin produced by other Clostridium. This hemolysin alters erythrocytes, leukocytes, platelets, macrophages and fibroblasts. Its real role in the pathophysiology of the infection is still poorly understood.
VI – LABORATORY DIAGNOSIS OF TETANUS:
The role of the laboratory is secondary, the diagnosis is almost exclusively clinic. The tetanus bacteria remains localized at the point of penetration, it never spreads, no sepsis.
At the time of sampling (early symptoms of tetanus) in 75% of cases, the germ has disappeared from the wound to other bacterial species.
A – Direct diagnosis:
Rarely seeks to isolate C. tetani at the front door, especially as the culture results are random. Can be removed from the serum and:
– Sowing double sampling as is and after heating to keep only the spores on solid medium (VL middle or TGY)
– Include in the boxes of the antitoxin, colonies then appearing after 3 to 4 days at 37 ° C with a halo,
– Inoculate part of the levy to the animal to try to reproduce the experimental disease in mice.
The morphological and biochemical features of the seed for the identification of C. tetani have been previously described.
It should be driving parallel cultures aerobically to detect either an association (aerobic-anaerobic) or substitution by pyogenic particular.
B – Indirect diagnosis:
It is not possible to detect the circulating toxin; Indeed the toxinémie is very transient, the substance being fixed immediately on the nervous tissue.
Tetanus antibody can not be assayed in the context of a diagnosis of tetanus, because the course of the disease, the amount of toxin released is sufficient to cause the disease, but insufficient to cause an antigen stimulation.
Measurement of serum antibodies against is interesting to study the immune status of a population (and check the correlation as a function of age group between cases of tetanus and lowered immunity) (Figure 2) and to check the response to vaccination.
There are several techniques for determination of tetanus antibodies:
– Against immunoelectrophoresis,
– Agglutination of latex particles, hemagglutination,
– Immunosorbent assays (ELISA)
– Radioimmunoassay (RIA) techniques.
VII – TREATMENT:
A – Preventive treatment:
The best prevention is a good vaccination; for almost all subjects with tetanus, previous vaccination is nonexistent, unknown or very old, the last booster dating back more than 10 years. The séroprévention is an expensive practice, which does not provide absolute protection (4-7% of tetanus occur despite séroprévention).
1. tetanus vaccination:
Well managed, it confers a nearby 100% protection. Progress has been made in recent years for the vaccine, purified toxoid is more concentrated and adsorbed on a mineral adjuvant (calcium phosphate for IPAD T-Pasteur and aluminum hydroxide for Tetavax Mérieux). These two main vaccines distributed in France, confer some immunity in 2 injections, provided they are spaced more than 2 months and a reminder made after one year. Any subsequent injection occurring several years later and even decades later leads to a secondary type response.
The vaccine is administered intramuscularly or subcutaneously (in scapular region or arm), it is well tolerated (reaction only in 1-3% of recipients). Neurological accidents are exceptional: 1 case per 2.5 million doses. There are no cons-indications. Pregnancy is not a cons-indication, vaccination is recommended even for pregnant women in developing countries to prevent neonatal tetanus.
Tetanus toxoid is often associated with diphtheria toxoid (DT), pertussis vaccine (DT-cock) or antipoliomyélite (DT-cock polio or Tetracoq).
It is advisable to France the following vaccination schedule:
– From 3 months DTCP (3 injections at least 4 weeks apart)
– From 15-18 months booster DTCP,
– 5-6 years DTP booster,
– DTP booster at 11-13 years,
– To 16-21 DTP booster or TP,
– More than every 10 years or TP T,
– Beyond 60 years or from the callback retirement or full revaccination.
Finally, the vaccine can be administered simultaneously with a tetanus antitoxin injection or of specific immunoglobulins without altering the immune response.
It is considered that the protective levels of antitoxin antibodies is from 0.01 or even 0.025 U / ml of serum (different authors). The vaccination coverage in children ranging in France between 90 and 95%.

(A) minor wounds including punctures, cuts, abrasions little penetrating, unsoiled without foreign body. Can be placed in this category some non-traumatic wounds (leg ulcers) and all surgical procedures: particularly work on the foot, the digestive tract, uterus, an open fracture.
(B) Traumatic Wounds widespread, penetrating with foreign objects, stained or treated late (after 24 pm) shock with severe bleeding, musculoskeletal disrepair.
Nontraumatic exhibitions extensive burns, septic abortions, septic deliveries, frostbite, necrotic ulcers, gangrene.
(1) heterologous animal serum (at least 1500 IU) or human tetanus immunoglobulin (at least 250 IU is a light bulb).
The dose will be doubled in case of risk (b) where the earlier vaccination is dubious or nonexistent.
(2) The vaccination will be completed later under the simplified scheme currently recommended.
If this is the first vaccine injection received by the patient, provide the second injection after four weeks, and recall six months to a year later. If it is the second vaccine injection received by the patient, only the recall is necessary, six months to a year later.
2. Serotherapy:
The purified serum administered at 1500 U subcutaneous injection by the method of Besredka protects for a maximum of 20 days. The specific gamma globulin (Tétaglobulines) administered intramuscularly (bulb 250 IU) provide protection for 1 month and take shelter in serum disease, but are expensive.
This serum therapy must be associated with vaccination.
What to do for the prevention of tetanus in injured or anyone exposed is clearly defined in the guide to the prevention of tetanus due to the Ministry of Health (Table I). Elderly patients are particularly affected. Prevention is based on vaccination. When vaccination is old, it is advisable to repeat the booster injection:
– In the elderly over 60 years with the last vaccination dates back more than 20 years,
– In people whose prior vaccination was incomplete (less than 3 injections).
We must seize every individual contact opportunities with health services to be vaccinated or revaccinated elderly:
– Any medical consultation,
– Systematic visit to retirement,
– Vaccination in geriatric communities, nursing homes, hospitals, at the institution entrance.
B – Curative treatment:
It is performed in specialized centers, this will not be developed here will remember only the principle of this treatment.
– Therapeutics specifically referred to:
– Processing the front door (trimming …)
– Systematic antibiotic therapy (penicillin G at 4 million units per day for adults)
– Curative serum therapy systemically,
– Vaccination because tetanus is not immunizing and recurrences are not uncommon.
– Therapeutics symptomatic referred:
– Sensory isolation,
– Sedatives (barbiturates) and muscle relaxant drugs (diazepam)
– Resuscitation
– Electrolyte and nutritional resuscitation.
Prognosis
In intensive care centers in France, overall mortality is 11 to 33%, it reaches 50% in 80 years. The percentages of deaths are higher in developing countries.



You must be logged in to post a comment.