Pseudomonas aeruginosa
Pseudomonas aeruginosa, Greek Puon = pus and Greek kuanos = dark blue, is referred to Pseudomonas aeruginosa Latin species name = aeruginosus covered in rust. Isolated in 1882 by Gessard.
This is the species most known and most widespread of the genus Pseudomonas. The more pathogenic, it is the type species of the genus.
I – HABITAT:
It is a bacterium that normally lives in the state of saprophyte in water and moist soil or on plants. It resists evil desiccation. This bacteria can live in commensal in the gut of humans and various animals. The B.
Pseudomonas aeruginosa can survive and multiply in an endless variety of liquids and circles on media and materials especially if they are wet.
Considered an opportunistic pathogen that is the germ standard hospital or hospital-acquired infections.
II – MORPHOLOGY AND CHARACTERS CROPPING:
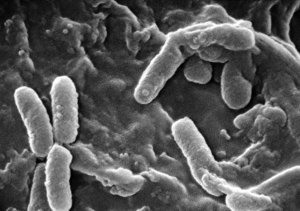
 Bacillus Gram négatif- 1-3 pm long; 0.5 to 1 micron wide.
Bacillus Gram négatif- 1-3 pm long; 0.5 to 1 micron wide.
Sometimes surrounded by a pseudo-capsule called slime that can play an important role in the pathogenicity of this bacterium.
It can be grown easily on all media under aerobic conditions (37 ° C or 30 ° C). It gives off an aromatic odor characteristic of mock due to the production of ortho-amino-acetophenone via tryptophan metabolism and not related to pigment production. A selective medium as Drigalski medium suitable for culture. Selective media based Cetrimide that the antibiotic can add (ac. Nalidixic) are proposed for research in highly contaminated products or water (hydrology).
A – colonies aspects:
They are unique to this species. Spontaneous dissociation into 3 main types can be observed:
– Settlements (“off”): isolated, large with a domed central part and an irregular contour – Fried Eggs (fried eggs). They are characterized by autolysis which gives a metallic appearance, iridescent when cultured sheet of the bacterium.This phenomenon is related to the action of bacterial proteolytic enzymes.
– Sm colonies (“small”): small, slightly curved mates with a regular circular edge.
-. M colonies (mucosa), curved, opaque, viscous sometimes flowing like Klebsiella These colonies almost specifically found in chronic infections, urinary tract or lung. The bacterium then produces an extra-cellular polysaccharide (alginic acid) that is different from “slime”.
B – Production of pigments:
This is a characteristic of this species; they are used for identification.
This property is not correlated with either the virulence or with protection. These pigments are fluorescent or non-fluorescent.
1. pyoverdine:
Fluorescent yellow-green pigment, soluble in water, insoluble in chloroform of molecular weight 1500, quinolinic chromophore associated with two small peptides.
This is a siderophore that by complexing with Fe ions can capture the extracellular iron.
Oxidized pyorubine in old cultures. Highlighted in the middle of King B (phosphate, sulphate, glycerol, peptone), its production is inhibited by sodium ions and promoted in iron deficiency environments.
2. Pyocyanin:
Pigment blue soluble in water and chloroform, characteristic of P. aeruginosa is the only species to produce it (highly polar compound, phenazine of Nature). The synthesis of this pigment is decreased in the presence of an excess of phosphate ion and sodium. This is a pH indicator, in solution at pH = 3 red in neutral or alkaline medium = blue. It can act as terminal electron acceptor if the respiratory chain is inhibited for example by Na azide.
Pyocyanin further has a bacteriostatic action on certain bacteria in particular Gram positive. It is highlighted in medium A King (low mineral content, glycerol, peptone pepsin).
There are apigmentées strains; less than 5% of wild-type strains do not produce either of these pigments. They are frequently isolated from antibiotic-treated patients.
There are strains melanogenic = black brown pigment diffusing (not producing Pyocyanin or pyoverdine) isolated from purulent lesions.
There are still varieties erythrogenic = red-brown pigment aéruginosine A, sometimes called pyorubrine.
Note that other Pseudomonas produce pigments including plant pathogenic species and it is appropriate to make a differential diagnosis:
P. fluorescens, P. putida, P. aureofaciens, P. chlororaphis P.lemonieri, P. cepacia, P. stutzeri, P. mendocina, P. vesicularis, X. (P.) Maltophilia, P. paucimobilis.
III – IDENTIFICATION BACTERIOLOGICAL:
The diagnosis is easy oxidase (+), cultured at 37 ° C: 41 ° C culture but not at 4 ° C. It is better to study the biochemical properties at 30 ° C. Circles A and B King (pyocyanin production and pyoverdine) oxidation of certain sugars with acid production, use as a sole source of carbon and energy many hydrocarbon substrates (achieving auxanogramme in a simple mineral medium) .
Hydrolyzed gelatin, lecithin, DNA.
In anaéobiose breathes nitrates resulting in confusion if the deep agar contains nitrates, but its metabolism is only respiratory.
Arginine deiminase positive.

IV – TOXIC SUBSTANCES AND PRODUCTS PROCESSED:
Apart pigments, which we have seen interest in the identification, B. aeruginosa develops proteins and toxic to humans, laboratory animals or plants. There are mainly: a thermostable hemolysin, exo-enzymes (proteases, phospholipase) and protein toxins (exotoxin, enterotoxin).
Hemolysin:
Two hemolysin are produced: a thermostable glycolipid and phospholipase C.
– Hemolytic glycolipid is a non-enzymatic low molecular weight substance and nonantigenic thermostable and relatively low toxicity.
– Phospholipase C. The hydrolysis of the lecithin is due to a lecithinase, thermolabile, comparable to the alpha-toxin of Clostridium perfringens It produces a limited inflammatory reaction, edematous, erythematous or hemorrhagic animal resembling what is observed. in humans in some forms of skin infection with P. aeruginosa.
Proteases:
P. aeruginosa produces proteolytic enzymes (elastase, alkaline protease, collagenase caseinase) which are virulence factors because their actions combine explaining the tissue destruction observed during infection.
Exotoxin A:
This lethal toxin was discovered by Liu in the blood of dying rabbits after injection of a living culture. It has no proteolytic activity or lécithinasique (purified 66.6 kDa, 2 subunits A and B, LD 50 of 0.05 to 0.10 ug for the mouse).
This toxin has the same mechanism of action as the diphtheria toxin (ADP-ribosylating toxin) acting by inhibiting protein synthesis by alteration of the elongation factor EF2. Toxinogenesis is not related to the presence of a lysogenic phage.
The toxin is produced by more than 90% of the strains.
Exo S:
Some strains of P. aeruginosa produce another different toxic exotoxin A having ADP-ribosyltransferase activity, excreted by 40% of the strains.
Cytotoxin:
Cytotoxin (“Leukocidin”) is a protein of 25.1 kDa with a lyrical work in small doses on different cell types in particular leukocytes (PMN, lymphocytes), produced by more than 95% of the strains.
Enterotoxin:
It is not well known. It causes fluid accumulation in ligated rabbit handle and could be the cause of enterocolitis B. aeruginosa.
Vascular permeability factor
V – PATHOGENICITY NATURAL:
Low virulence for normal individual, B. aeruginosa is against a formidable infectious agent when the immune defenses of the subject are affected.
P. aeruginosa is an example of the opportunistic pathogen.
Particularly sensitive patients are infants, the elderly, people with serious conditions, chronic, metabolic (diabetes) but mainly hematological or cancerous. Immunosuppressive drugs, corticosteroids, antimetabolites promote infection with B. aeruginosa endogenous origin. In burn, this infection is a major cause of mortality. The wet crust and the diminution of local defenses favor rapid proliferation of the germ. Finally, the treatment or prevention of high-risk patients with broad-spectrum antibiotics contributes significantly to the increased frequency of infections with multidrug-resistant bacteria, including P. aeruginosa plays an important role.
A – Pulmonary Infections:
They can be primary or secondary to sepsis.
Primitive lung are observed exceptionally in healthy subjects but the current batch of tracheotomy patients, respiratory failure in prolonged antibiotic therapy of patients with blood diseases or cancer receiving chemotherapy.Evolution is severe (30-50% mortality), the germ is isolated sputum while blood cultures are usually negative.
Cystic fibrosis (children with cystic fibrosis pancreas) is complicated by bacterial bronchial infections including S.aureus in the early years, and under the influence of antibiotic therapy in B. aeruginosa in 70-90% of cases. The isolation of stem M mucous producing mucous exopolysaccharide (alginate: Polymer mannuronic acid and guluronic acid) is characteristic.
Finally lung damage can be observed in the B. aeruginosa septicemia.
B – urogenital infections:
Very frequent, they are never primitive, but always secondary to urinary tract exploration: single cystoscopy and bladder catheterization, indwelling urethral catheters, kidney or prostate procedure …
C – bone and joint infections:
B. aeruginosa is responsible for about 10% of osteitis and 20% of septic arthritis. The secondary osteitis, the most frequent, repeated at a compound fracture or intervention with implantation of a foreign material, or secondary infections of skin ulcers in a diabetic. Primitive hematogenous osteomyelitis is mainly seen among heroin and electively affect the vertebrae.
D – Eye Infections:
B. aeruginosa may be present as a saprophyte in the conjunctival fornix. Under certain conditions, it can cause superficial infections of the eye, such as conjunctivitis blepharoconjunctivitis were observed during cancer chemotherapy in patients with HCV of corneal lenses after the use of contaminated mascara.
In fact, these infections are rare but they are severe. B. aeruginosa is responsible for 15-20% of bacterial infections of corneal ulceration.
They earn very fast the entire eyeball. This panophthalmitis called, rightly, purulent eye, is a dreaded complication of surgery or ophthalmological investigations.
E – ENT infections:
B. aeruginosa is not a saprophyte current external auditory canal; only 1% of healthy individuals are carriers. It is against isolated in 45-65% of subjects with a banal otitis externa.
Otitis malignant B. aeruginosa was observed in elderly diabetics. Malignant term was used because of the possibilities of extension.
Recently a new form of otitis externa in B. aeruginosa was described as the “ear of the divers,” reaching divers oil research stations in the North Sea.
F – meningeal infections:
They are rare: 2% meningitis together, however 10% of meningitis after neuro-surgery due to P. aeruginosa.
G – Skin infections:
In healthy subjects can be observed with a onyxis perionyxis realizing green nail interdigital infections, secondary infections of leg ulcers. Polymorphic cutaneous lesions known Secthyma gangrenosum occur during sepsis particularly in leukemia. In burn injuries colonization by B. aeruginosa is rapid; at the thirtieth time, 20% of lesions are infected, 48% at the forty-eighth hour and over 60% in the fifth day. The major risk is sepsis, brutal, whose mortality rate is high: about 50%.
Skin infections with B. aeruginosa can be observed in warm and humid climate, but also in any subject in contact with contaminated water. Especially in our climate, the current vogue for baths with warm or hot water (hot tubs, spa, heated or thermal mud applications, medicinal baths, thalassotherapy, Roman baths) can cause folliculitis in Pseudomonas aeruginosa. Treatment with chlorine of these recreational water is sometimes absent, often inadequate and inefficient (pH, filtration, ventilation …). A risk also exists for swimming in stagnant water or poorly renewed or untreated (gravel pits, crowded seaside coves without currents or low tide in summer, near sewage) which are associated, of course other water-borne bacteria.
H – Septicaemia:
They are steadily increasing, as are other gram-negative bacilli septicemia.
These septicemia are observed firstly among infants and also in adults treated with corticosteroids or anti-metabolites. They succeed to secondary infections of skin burns, bacterial blooms of tracheotomy patients. Finally catheters and probes are also entrance doors. The prognosis of septicemia B. aeruginosa is severe; mortality is greater than 50% but this of course depends on the underlying disease and how early and choice of treatment.
J – enteritis B. aeruginosa:
Their pathophysiological mechanism is similar to that of other enteritis. They are very rare. Been described diarrheal outbreaks in nurseries.
The three clinical forms are:
– Acute enteritis: secondary to broad spectrum antibiotics or ingestion of contaminated food very,
– Typhlitis: necrotizing colitis localized in the cecum occurs in leukemia and neutropenic patients
– Enteritis water (Shanghai Fever) with an array of typhoid fever, related to the absorption of polluted water.
However, isolation from fecal P. aeruginosa should not lead to systematic antibiotic therapy.
K – Endocarditis:
Approximately 1% of endocarditis may be due to B. aeruginosa. The frequency of tricuspid endocarditis in drug addicts increases.
VI – MODEL PHYSIOPATHOLOGICAL:
P. aeruginosa colonizes the mucous membranes or wounds and adhere through adhesion factors or external polysaccharide compounds. In a non-immunized patient against a strain of the same serogroup 0 rapid multiplication of bacteria occurs under the influence of different virulence factors already mentioned, in particular the LPS-endotoxin, forms a local inflammatory focus. In this focus focus many phagocytes, neutrophils that are in favorable cases ensure the rapid destruction of bacteria. Specific serum antibody species for enzymes or group to LPS are produced in a few days, but too late to play a role in the immediate phenomena.
If immune deficiency on the number and / or quality of polymorphonuclear phagocytosis is insufficient and stage of invasion succeeds colonization. The bacteria then overflow cell barriers of defense in the inflammatory focus and multiply; bacteremia is usually seen with secondary locations. Exotoxin production is intense and its wide distribution. Because of the diverse virulence factors of this organism, a single pathophysiological model can not account for the complexity of pathogenic infection.
VII – EPIDEMIOLOGY:
Nosocomial nature of most of the infections with P. aeruginosa necessitates perfect knowledge of the transmission mechanisms. The use of epidemiological markers (serotyping, phage typing, pyocinotypie) reliable to track hospital outbreaks and consider the fight against the sources of contamination.
A – Sources of contamination:
The external environment and water in all its forms or patient himself by his exudates (urine, sputum, stool, …)
The hospital environment: cut flowers (water vessels), potted plants, fruits, raw vegetables or salad (tomatoes, carrots, radishes, lettuce), siphons of sinks or floor, humidifiers, ventilators, distilled water, ( ability to increase up to 107 cells / ml, with no visible disorder).
Antiseptic, eg quaternary ammonium compounds are often inactive and permit multiplication of the bacterium.
B – contamination vectors:
Transmission from a source of initial contamination to a patient or patient to patient, the result of contamination or pollution inert supports, hands of visitors and especially the staff who carry the bacteria in a now classic epidemiological pattern. In intensive care units, tracheotomy patients quickly host B. aeruginosa colonizes the upper respiratory tract. The germ can spread and in service.
C – Epidemiological Markers:
Epidemiological markers available are: serotyping, phage typing and pyocinotypie. The antibiotype is only an indication generally insufficient.
Serotyping is the marker most commonly used as phage typing and pyocinotypie are performed by specialized laboratories.
1. Serotyping:
Antigenic classification Habs currently includes 17 serogroups 0 (corresponding to AgO lipopolysaccharide, thermostable) which identify 90-95% of the strains by blade on an agglutination technique (mimunsérums Diagnostics Pasteur).
0 serogroups most common are 01, 05, 06 and 011 (the latter having the peculiarity of having a hydrolase activity ONPG).
During bacterial, it most frequently isolated serogroups 01, 2, 5, 6, 7, 10 and 11.
The global geographical distribution of serogroups varies widely between, on the one hand, more or less frequent cosmopolitan strains, and also rare strains (014, 15.17) absent in some countries.
The determination of H serotypes (corresponding to the flagellar protein antigens, thermolabile) lowers the percentage of non typeable, but this technique is not commonly used.
2. Phage:
The bacterium Pseudomonas aeruginosa can be lysed by numerous lytic phages. Most strains are lysogens or poly-lysogens. The same strain can host, integrated on the chromosome or on a plasmid, a dozen temperate phages.This high frequency lysogénie is characteristic of P. aeruginosa and is rarely found in other Pseudomonas species.
Phage typing using bacteriophages 17 by the method of LINDBERG allows to score 98% of the strains, and the number of phage is currently close to 300. This is an excellent complementary method of serotyping in the local epidemiological study.
3. Pyocinotypie:
The pyocinotypie consists in highlighting the production of bacteriocins: pyocines = aeruginocines. This technique is relatively simple provided you have some sensitive strains required for the reveal.
The pyocines are classified into two main types:
– Type S: susceptible to proteolytic enzymes, showing no particular form electron microscopy
– Type A: resistant to proteolytic enzymes having a hollow cylinder and dual structure resembling a tail of the bacteriophage by electron microscopy. These could be defective phages. The pyocinotypie allows using the method described by Fyfe, Harris and Govan in 1984 using 13 indicator strains to distinguish 105 main types and 25 subtypes.
One of three methods to mark 90 to 95% of the strains. In difficult cases, the combination of two methods improve this percentage. Epidemiological markers allow to know the flora contaminating a service and thus determine with a high probability of the existence of contamination within the service (known strain) or endogenous contamination (new strain).
VIII – TREATMENT AND PREVENTION:
A – Sensitivity to antibiotics:
P. aeruginosa is only sensitive to some antibiotics and the choice of treatment is important. Despite the effectiveness of some, success is often relative and control efforts against infections with B. aeruginosa must come first through prevention: hygiene or vaccination.
P. aeruginosa is resistant to many antibiotics (benzylpénicillines, aminopenicillin, cephalosporins first and second generations phenicols, tetracyclines, trimethoprim). This resistance has three mechanisms:
– The impermeability of the wall to certain antibiotics (intrinsic resistance to penicillins M = methicillin, cloxacillin; acquired resistance involving porins = ticarcillin, cefsulodin, imipenem)
– Enzymatic inactivation (17 beta-lactamase plasmid, several types: PSE = Pseudomonas Specifies Enzyme, PSE-1 and PSE-4: CARBécillinases; OXA = oxacillinases; TEM 1 and 2), natural resistance to the first beta-lactam synthesis by a chromosomal beta-lactamase usually repressed (Case = inducible cephalosporinases of Sabath)
– Changes in the affinity of the antibiotic to the target (PBP).
– There are at least thirty resistance plasmids known in P. aeruginosa can encode multidrug affecting beta-lactams and aminoglycosides. Forming ten incompatibility groups, they distribute schematically into three categories: specific plasmids of the genus Pseudomonas, plasmids can flow between Pseudomonas and Enterobacteriaceae usual plasmids Enterobacteriaceae sometimes found in Pseudomonas.
These are some general data explain the very different resistance phenotypes that are observed and how hard it is on the basis of the value of MIC published to establish a hierarchy among the proposed antipyocyaniques molecules. The variable epidemiological situation of a hospital and a service to another, make any forecasting sensitivity.
The choice of a beta-lactam may be based on susceptibility testing among carboxypénicillines (ticarcillin, ticarcillin + ac Association. Clavulanic) with good speed-kill as imipenem, the acyluréidopénicillines (aziociiïine, piperacillin) acylpénicillines (apalcillin), cephalosporins (ceftazidime and cefsulodine) monobactam (aztreonam), carbapenem (imipenem). In addition, the most effective combination of a beta-lactam with an aminoglycoside is often sought to be rapidly bactericidal in generalized infections. Among the several aminoglycoside resistance phenotypes were observed, amikacin remaining the most active. The decrease in permeability to beta-lactams also affecting aminoglycosides makes some particularly resistant strains. P. aeruginosa is resistant to nalidixic acid but the 2nd generation quinolones have an interesting activity: pefloxacin, norfloxacin, ofloxacin and ciprofloxacin giving the lowest MIC.
Aminoglycosides associated with beta-lactam antipyocyaniques are the first-line treatment.
The sensitivity of P. aeruginosa colistin is constant, but its in vivo efficacy is disappointing. Some strains are sensitive to fosfomycin but this antibiotic should be involved to avoid the rapid emergence of resistant mutants.
In the embodiment of the antibiogram, too heavy inoculum is a pitfall to avoid.
This is due to the tendency of bacterial bodies to form agglutinais.
B – Protection by vaccination:
Prevention of infection, especially in hospitals, requires above all general hygiene measures and the choice of antiseptics.
Much work has been devoted to immunoprevention infection with B. aeruginosa.
Experimental studies began in 1960 and were formed in several directions. USA: pseudogene vaccine (serotypes 7 – valent
Preparation lipopolysaccharide), the United Kingdom soluble polyvalent vaccine (surface antigens – 16 serotypes – EPI vaccine-01), Romania: heated bacterial suspension (11 serotypes), France: versatile combination vaccine (10 serotypes, heated bacterial suspension + Staphylococcal + staphylococcal toxoid).
Their clinical applications can now summarize the use of two types of vaccines:
– Bacterial vaccines (suspension heated bacteria)
– Acellular vaccines (purified extracts various, but usually containing LPS).
In France, the versatile cell vaccine is used for prophylaxis in major burns.
Immunotherapy is sometimes recommended with natural or hyperimmune immunoglobulins.
You must be logged in to post a comment.