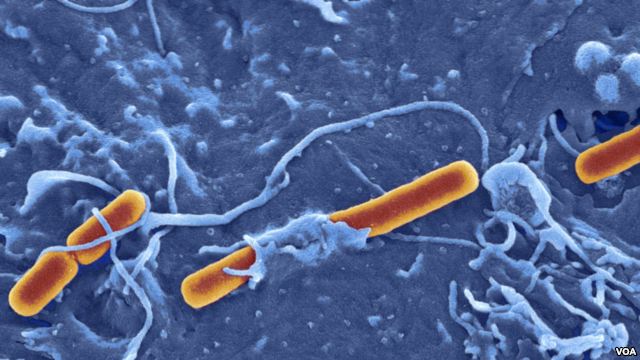
Enterobacteriaceae Shigella are responsible for bacillary dysentery and diarrhea, which are a major public health problem in developing countries.
They are characterized by their low metabolic activity and their genetic relatedness with Escherichia coli (GC% are very close).
I – BACTERIOLOGICAL CHARACTERISTICS COMMON TO ALLSHIGELLA:
In addition to the general characteristics of Enterobacteriaceae strains belonging to the genus Shigella all have the following common characteristics:
– Motionless (broth in exponential phase).
– No culture medium Simmons citrate.
– Lack of LDC and tryptophan deaminase.
– Without gas glucose fermentation (with certain exceptions biotypes of S. flexneri and S. boydii 13 6 and 14).
– Never production of H ^ O.
II – CHARACTERISTICS OF EACH SPECIES:
 The four species of Shigella are distinguished from one another by biochemistry and antigenic characteristics, based on the study of polysaccharide antigens 0. The essential characteristics are reported in Table I.
The four species of Shigella are distinguished from one another by biochemistry and antigenic characteristics, based on the study of polysaccharide antigens 0. The essential characteristics are reported in Table I.
– S. dysenteriae = subgroup A
This species is characterized by the absence of mannitol fermentation.
There are 10 serotypes. S. dysenteriae type 1 and Shiga bacillus has an active beta-galactosidase, is indole (-), and rare in Enterobacteriaceae, does not have catalase. The Shiga bacillus is the agent of the great historical epidemics in Armies in the Field or refugee camps.
– S. flexneri = subgroup B
This species includes six serotypes and two variants.
– S. boydii subgroup C =
This species has 15 serotypes.
– S. sonnei subgroup D =
It is only one serotype. This case differs from the others by the presence of an ornithine decarboxylase and by the fact that the stem does not produce indole. This species can be divided into biotypes.
III – PATHOPHYSIOLOGY:
A – Shiga toxin:
Known since 1903 in S. dysenteriae 1, is localized in the periplasmic space of the bacteria and liberated upon lysis of the bacterium. It is a protein toxin of 70 kDa, encoded by the chromosomal gene consisting of an A subunit (32 kDa) and five B subunits (7.7 kDa). The B subunit consists of 69 amino acids identical to the B subunit of Shiga-like toxin, type 1 or verotoxin E. coli). The multimeric structure of the Shiga-toxin is comparable to that of the cholera toxin and LT toxin of E. coli, but without presenting antigenic community.
The B subunits are responsible for binding to cellular receptors (glycoprotein or glycolipid). Subunit A, after cleavage by a proteolytic enzyme, is reduced in a Al fragment with enzymatic activity that is internalized by endocytosis. The target is the ribosome, where a share on EF1 (exotoxin A of Pseudomonas aeruginosa and B. diphtheria toxin acting on EF2) in the region of the 60S subunit, the toxin causes an inhibition of the elongation of the chain peptide and consequently inhibition of protein synthesis.
The toxin exercises:
– Paralytic and lethal after IV injection in rabbits. The neurotoxic result of neurological disorders secondary to lesions of the vessels of the brain and spinal cord;
– An enterotoxigenic Action, reflected in hemorrhagic fluid accumulation;
– A cytotoxic action on target cells in culture (the most sensitive HeLa, KB cells, monkey kidney). The role of the toxin in the virulence of the bacterium and dysentery is not clearly established.
B – verotoxin:
Different bacterial species produce a toxin characterized by its cytotoxic potency for Vero cells.
This is very close to the Shiga toxin-toxin was found:
– Among strains of E. coli responsible for hemolytic uremic syndrome (Moskowitz disease), ulcerative colitis and in enteric strains (EPEC).
– By other bacterial species: 5. typhimurium, V. cholerae non-01 Vibrio and V. parahaemolyticus.
C – enteroinvasive power:
The enteroinvasive power is related to the presence of plasmids common to the different species of Shigella and E.coli entero-invasive (180 kb in S.
sonnei, S. flexneri at 220 kb) The expression plasmid virulence genes is under the control of temperature. invasive phenotype is expressed at 37 ° C and is reversibly lost at 30 ° C. Different proteins are responsible for invasiveness.
The entero-invasive power is demonstrated experimentally by the Sereny test (keratoconjunctivitis festering within 48 hours after instillation of a suspension of bacteria in the eye of guinea pig) – penetration in HeLa cells and death cells – staining with Congo red. Lipopolysaccharide (LPS) is involved in the virulence of Shigella.
Human disease is the consequence of the invasion of the colonic mucosa. The steps are the penetration into epithelial cells, intracellular multiplication, and the invasion of the adjacent cells and connective tissue of the villi.
This causes a strong inflammatory reaction causing abscesses and ulceration of the colon and the appearance of blood and mucus in the stools. The small intestine is usually not concerned. The infection is limited to the mucosa without passing through the lamina propria. Achieving the submucosa and systemic dissemination are exceptional.
IV – EPIDEMIOLOGY:
The only reservoir of Shigella is the gastrointestinal tract of man. These bacteria are not part of the normal flora of the gastrointestinal tract. They are present in the feces of patients or healthy carriers (convalescents, sick relatives).Shigellosis is the most communicable intestinal bacterial diseases; ten living germs can cause disease in healthy adults.
The spread of the disease is through food, drinking water contaminated with feces or person to person. Shigellosis occur where the sanitary conditions are defective. Hand washing and improving water supply are measures that reduce the fecal-oral transmission.
In France, about 1000 strains are received annually by the National Center of the Institut Pasteur Shigella. The largest number of strains is received in September-October. This is due to summer temperatures and holiday returns in exotic countries. S. sonnei is most often isolated. S. flexneri comes next. S. dysenteriae and S. boydii are rarely isolated in France. Small outbreaks can be observed in infants or elderly living in institutions.
In developing countries, endemic shigellosis is primarily due to S. flexneri. The morbidity rate is high. Children from one to five are particularly affected. In some countries, mortality is high.
A pandemic of shigellosis due to 5. dysenteriae 1 began in 1969 in Central America. It now encompasses a broad region of Central Africa and the Indian sub-continent. The strain in question is resistant to many antibiotics.
V – PATHOGENICITY:
Shigellosis usually starts with watery diarrhea followed after 24 to 48 hours by the appearance of blood and mucus in the stool. He has a fever, abdominal pain and tenesmus.
Dehydration is possible but in a small proportion of cases.
Mortality, which with S. dysenteriae 1 may exceed 10% of the cases treated adequately, is due to various complications: cachexia, pseudoleucémique state, paralytic ileus, intestinal perforation, rectal prolapse.
The disease is particularly serious when it expresses after measles or when there is a pre-existing malnutrition.Extra-digestive localizations are infrequent. Less rare are urinary tract infections. Sometimes seen septicemic forms, arthritis, meningitis.
VI – BIOLOGICAL DIAGNOSIS:
A – Isolation of the bacterium:
This is the only way to make the diagnosis of shigellosis certainty.
Stool:
This is the method of choice. It is done by seeding freshly voided faeces and mucous phlegm if they contain.
The stool microscopy reveals polymorphonuclear who witness an invasive process.
The isolation of the bacteria is done on a non-selective inhibitor agar: Hektoen, Drigalski, Mac Conkey. The SS medium does not allow the growth of some strains of Shigella. It is therefore not advisable. There is no middle effective enrichment for Shigella.
Suspect colonies (lactose (-) and H2S (-)) are the subject of a more complete characterization. It is important to make a differential diagnosis between Shigella and “Aïkalescens-dispar” which are E. coli motionless and does not produce gas.
Two characters, the LDC and growth medium citrate Christensen, are always negative with Shigella as they are generally positive with “Aïkalescens-dispar.”
Other tests:
Blood cultures. They are rarely used, but may be positive in a small percentage of cases.
Urine. They allow the isolation of the bacterium in cystitis or pyelitis Shigella are rare but not exceptional.
B – Serotyping or serological typing of a strain:
It is only when the diagnosis of Shigella established with certainty that the antigenic typing can be done by slide agglutination. The agglutinating sera are marketed:
1. In group A:
2 polyvalent sera
This subgroup contains 10 serotypes negative mannitol, 2 of which are exceptional (9 and 10).
Al serum: nnti Shigella dysenteriae negative indole: 1, 3, 4, 5, 6.
Serum A2: SMTi Shigella dysenteriae positive indole-2, 7, 8.
2. Under Group B:
1 polyvalent serum, marketed under the SMU-serum flexneri name.
It agglutinates 6 serotypes of this subgroup
3. Subgroup C:
3 polyvalent sera
– Cl driven Shigella boydii indole negative: 1, 2, 3, 4.
– C2: Shigella boydii negative indole: 8, 10, 14.
– C3: SMTi Shigella boydii positive indole: 5, 7, 9, 11, 15.
Serotype 6, closely related to Shigella sonnet Phase II agglutinated by Shigella sonnei serum.
4. Subgroup D:
1 mixed serum: D, marketed under the name of anti-serum mixed sonnei.
It agglutinates the 2 phases of Shigella sonnei.
C – Serologic tests:
It can be done by agglutination, but lacks interest in dysentery syndromes because it is too late and the specificity is uneven across subgroups.
Sometimes it is useful to connect certain rheumatic syndromes to S. flexneri infection. In such cases, it is desirable to take two serums, two weeks apart, to observe the titre of agglutinins.
VII – ANTIBIOTIC SENSITIVITY:
Shigella are irregularly sensitive to antibiotics. Ampicillin, tetracycline, colistin, sulfonamides and trimethoprim are generally active.
However, remember that it was during an outbreak of shigellosis that multiple transferable resistance plasmids were discovered in Japan. Also, today, treatment should be guided by the results of susceptibility testing.
VIII – VACCINES SHIGELLA:
Injectable vaccines containing killed bacteria or oral vaccines based on live attenuated bacteria are ineffective.
By genetic engineering techniques, it was possible to accurately analyze the determinants of pathogenicity and immunogenicity of Shigella. Research is underway to produce a live oral vaccine. This research is done in the following directions:
Production of “hybrids mutants” Shigella attenuated by incorporation of E. gene segments coli producing E. colicontaining genes of Shigella using attenuated Salmonella Typhi containing coding sequences of genes for the synthesis of Shigella antigens.

You must be logged in to post a comment.