Treponemes belong to the order of Spirochoetales they all general features described above. There are many species of which are saprophytic treponemes mucous membranes. Unlike most saprophytic species, pathogenic treponemes for humans are not cultivable in vitro Three species are pathogenic to humans, it is.:
– Treponema pallidum, the agent of venereal syphilis and non-venereal endemic syphilis or bejel.
– Treponema pertenue agent of yaws.
– Treponema carateum, officer or pinta pinta.
TREPONEMA PALLIDUM
Treponema pallidum and Treponema pallidum, is the agent of syphilis, strictly human disease, almost always venereal transmission. This bacterium was recognized in 1905 by Schaudinn. The Complement fixation reaction described by Bordet was applied in 1906 by Wassermann serological diagnosis of syphilis.
I – EPIDEMIOLOGY:
Several theories exist on the origin of syphilis. According to ancient theory, syphilis was imported into Europe in the fifteenth century by sailors of Columbus. Another theory claims that the disease existed since ancient times. Anyway, syphilis is now disseminated disease worldwide.

The transmission of syphilis is almost always through direct contact venereum: genital chancres, anal or oral incidentally. Treponemes are very numerous in skin lesions and mucous membranes. Their vitality is extremely low outside of the human body, making it non-existent risk of transmission of potentially contaminated objects. The transfusion of blood from a donor with primary secondary syphilis can transmit the disease, which requires serological screening for syphilis in all blood donor.
The number of cases of primary secondary syphilis had fallen sharply because of the effectiveness of penicillin. In recent years there has been a resurgence of the disease due to several factors: human migration, exotic tourism, release of morals, homosexuality. Approximately 4,000 new cases were reported in France each year to health authorities. Today syphilis is not a reportable disease.
II – NATURAL PATHOGENICITY:
After infection, incubation of syphilis, three weeks on average, is completely silent.
– Primary syphilis
“The first clinical manifestation is the chancre, painless ulcer with indurated base, sitting at the inoculation and accompanied by its satellite lymphadenopathy. Untreated, the chancre heals spontaneously in 4 to 6 weeks with or without a scar.
– Secondary Syphilis
This phase begins about two months after the contagion. It is characterized by skin lesions and mucous membranes: roseola followed syphilides mucous patches, warts, alopecia, nail damage, etc … These lesions, due to dissemination of treponemes through blood and lymphatic system, are highly contagious. They may be accompanied by an infectious syndrome and polyadenopathies. These signs disappear spontaneously within one to two years.
– Latent syphilis
When the signs of the secondary period have disappeared, syphilis is asymptomatic and not contagious. The diagnosis can only be made by serological tests. Latent syphilis lasts for several years or even decades, the patient may die of another disease.
– Tertiary syphilis
After these years, some patients show severe damage to tertiary syphilis. These are cardiovascular lesions (aortitis, aortic aneurysm), skin (gums) or neurological (tabes, general paralysis).
– Congenital syphilis
Syphilis can be transmitted to the fetus by a mother with active syphilis. Placental transfer of T. pallidum causes septicemic reached the head of the fetus or fetal death or clinical manifestations of congenital syphilis.
– Endemic syphilis or bejel
It is in Africa and the Caribbean. Contamination is not venereal.
It is often in childhood in contact with infectious lesions. Endemic syphilis is not complicated of late visceral.
III – PATHOGENICITY METHODS:
Although syphilis is a strictly human disease, it is possible to induce experimental infection in animals. The chimpanzee develops a disease that approximates the human syphilis. The rabbit is the animal most used. It can be inoculated by ocular, subcutaneous or intra-testicular.
The intra-testicular injection of T. pallidum causes a rabbit in a few days-rich treponemes orchitis. The Nichols strain, isolated in 1912 from a CRL is regularly maintained by serial passage in rabbit testes. It is used to perform the test Nelson.
IV – BACTERIOLOGICAL CHARACTERS:
A – Morphology and vitality:
The morphology of T. pallidum is described below. Refer to “direct Bacteriological diagnosis.”
Non-culturable in vitro, T. pallidum can nevertheless be collected in a large amount of experimental rabbit orchitis. Its vitality from the body is extremely low. However in vitro treponemes can be maintained mobile and pathogens during several days in the medium described by Nelson survival.
T. pallidum is very sensitive to the action of antiseptics.
B – Antigenic Structure:
T. pallidum has a complex structure. Four groups of antigens were identified.
1. The lipid cardiolipin or hapten Wassermann:
This is a common phosphatidyl glycerol at all treponemes and found in animal tissues. The heart and liver are particularly rich. The syphilitic infection causes tissue remodeling in lesions. Associated with the Treponema proteins, antigenic hapten becomes. The corresponding antibodies are called reagin.
2. A specific protein antigen group:
It is common to all treponemes, pathogenic or not, and carried by the fibrils. This antigen extract of Treponema Reiter, can be used in complement fixation reaction.
3. An antigen polysaccharide envelope:
II is specific for T. pallidum and causes the formation of antibodies reactive in immunofluorescence.
4. treponemal antigens of the body:
Their nature is unclear. They create the T. highly specific antibody pallidum involved in the testing of Nelson.
C – Immunity:
The natural or experimental infection with T. pallidum causes an immune response mediated by both cellular and humoral.
As the infection progresses, there is a superinfection immunity protects against recontamination. The developed antibodies are not sufficient to eliminate the organisms and prevent the disease from progressing.
A subject treated effectively can again acquiring syphilis. The residual presence of antibodies does not protect against reinfection.
There is no vaccine against syphilis.
V – DIRECT BACTERIOLOGICAL DIAGNOSIS OF SYPHILIS:
It is in the primary and secondary syphilis lesions (cankers satellite nodes, mucous patches) or of congenital syphilis (phemphigus, coryza) T. pallidum can be found. This research should be done on any suspicious genital ulcer or erosion, primarily antibiotics and antiseptic before any application on the lesions.
The detection of T. pallidum is made only by microscopic examination since this bacterium does not grow in vitro.
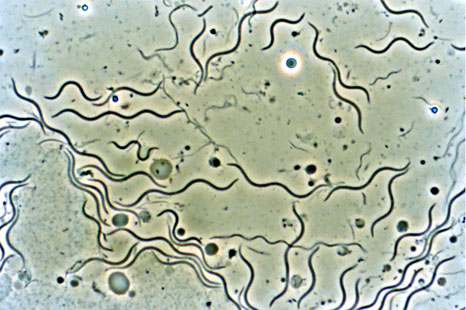
A – Microscopic examination to black or ultramicroscope background:
Because of the great fragility of the bacteria, the removal of serum performed using a lancet or pipette is made in the laboratory. The collected serum is deposited on a slide. covered with a cover slip and immediately examined microscopically black background.
T. pallidum appears as a fine, spiral bacteria at regular turns and clamped to the number of 6 to 12 and the ends are tapered. Its length is about 10 (Jm and thickness of 0.2 [m \ The bacterium has a low refractive power;. Its pale color (pallidum) contrast with the black background.
The mobility of T. pallidum is characteristic. Three kinds of movements are usually combined:
– A movement screw, rotation on its axis,
– A pendulum,
– A wave motion that propagates from one end to the other of the bacterial body.
But only a trained observer can distinguish T. pallidum other treponemes commensal genital mucosa.
A negative research T. pallidum does not eliminate alone diagnosing syphilis and it may be useful to repeat the examination.
B – Examination after staining:
After fixation of the sample on a slide, the use of dye allows to thicken the bacterial body and make it visible to the ordinary microscope. The Vago stain (methyl violet) and the Fontana-Tribondeau (silver salts) have the disadvantage of distorting the bacterial body and void T. pallidum its characteristic morphology. Moreover, it is not possible to observe the mobility. Also these colorations are they neglected today.
C – Immunofluorescence:
The smear is covered with a serous fluid. syphilitic serum containing antibody labeled with a fluorescent dye. After washing, the smear is observed in UV light to search for treponemes become fluorescent.
This technique is difficult, should be done by a trained technician. It does not allow to identify the mobility of the bacterium.
It is always advisable to complete the direct search of T. pallidum by a serological diagnosis of syphilis.
VI – SEROLOGICAL DIAGNOSIS OF SYPHILIS:
It is to look in the blood of the martyrs of antibodies the body’s defense demonstrations. This research is the subject of a systematic screening preventive medicine in particular during the premarital examination and during pregnancy.
Many reactions have been used to highlight reagin, antibodies against cardiolipin. In 1906, Wassermann applied to the diagnosis of syphilis complement fixation reaction described by Bordet.
This is the classic Bordet-Wassermann reaction (BW), which is now abandoned because of its lack of sensitivity.Indeed, it did not detect syphilis or old or very recent.
A decree published in the Official Journal on 12 October 1980 imposes the techniques to implement. These are the following:
– For a routine screening test for syphilis.
A reaction of each of the two groups was made with pure serum.
– Group 1 – Kline
-VDRL
– VDRL – Charcoal
– Group 2 – TPHA
– FTA – Abs.
– For a check-up.
Before or during the reaction quantitative treatment of the two groups is made with serum dilutions of the patient.These reactions allow to know the antibody levels and to monitor progress.
Besides these common reactions, the test of Nelson or immobilization treponemal test (TIT) is a technique that should be used to resolve difficult situations.
A – Description of reactions:
1. Reactions of Group I:
These are agglutination tests that detect reagin, anti-lipid antibodies. Reactions Kline and VDRL (Vénérai Disease Research Laboratory) are based on the same principle. They involve contacting a patient’s serum blade and an antigen composed of cardiolipin, lecithin and cholesterol placed in colloidal suspension. After stirring, the presence of reagin causes the formation of clumps. The micronized coal addition to the VDRL-charcoal or latex for the latex-VDRL are recommended because the technique is more sensitive and thus the proportion of false negative responses is reduced.
Despite a lack of sensitivity, these reactions in group 1 have a significant advantage: simplicity. As for the specificity of these reactions, it is not perfect. False-positive reactions were described during viral diseases, collagen diseases, malaria, pregnancy, dysglobulinémies. But they are rare enough that these reactions retain their value.
2. Reactions of Group II:
They are more specific than the reactions of group 1 because they use treponemal antigens.
a / TPHA (Treponema pallidum haemaglutination assay):
The reagent is a ultrasonnat of Treponema pallidum (Nichols strain) attached to sheep red blood cells. Patient sera is diluted in an absorbent consisting of ultrasonnat of sheep red blood cells and Reiter nonpathogenic treponemes, which aims to remove nonspecific agglutinins. Patient’s serum and the sensitized sheep erythrocytes are brought together in a microtiter plate. A positive reaction results in hemagglutination ply in the cup. A negative response in the absence of antibody, results in a sedimentation of the erythrocytes to the bottom of the cup.
Due to the simplicity of its execution and its specificity, TPHA is a reaction to advocate in current practice.
b / F.TA. Abs. (Fluorescent treponemal antibody absorption test):
This is an indirect immunofluorescence reaction. The antigen consists of Treponema pallidum, Nichols strain.Patient’s serum is previously diluted 1/5 in an absorbent made of a Treponema Reiter extract to remove non-specific group antibodies. The antigen and the serum of the patient are brought into contact on a slide. If it contains specific antibodies they bind to the treponemes and will be highlighted by an antiglobulin labeled with fluorescein isothiocyanate. If the response is positive, the fluorescent treponemal are seen in a microscope equipped with UV light
The FTA-Abs. is an extremely delicate and difficult standardizable reaction. It should be reserved for highly trained laboratory and can be common reaction. Well codified, it is very specific.
3. The test of Nelson or treponemal immobilization test (T P I…):
This test is highly sensitive and reserved for specialized laboratories. Indeed, it uses as an antigen a live strain of T.pallidum strain Nichols maintained by passages in rabbit testes. Treponemes can be maintained in vitro in the mobile environment, as specified by Nelson. Sera from patients with treponematosis cause in the presence of complement, immobilization treponemes. The results are expressed as percentage of immobilization in the reaction tube compared to a control tube devoid Complement. The interpretation of this test is as follows:
0 to 20% negative serum
20 to 50% serum doubtful
50 to 100% positive serum.
Nelson’s test is a standard method because it is highly specific and has a good sensitivity. Because of its price and difficulty of implementation, it must be booked in contentious situations. However, no more than the other reactions, it distinguishes them different treponematosis.
To be interpretable, the Nelson test must be made on blood collected sterilely and containing no drugs tréponèmicides (antibiotics).
4. Specific IgM Search:
Search IgM antitreponemal can be done by two techniques:
a / F.TA.- Abs. IgM:
This technique is the oldest. It lacks sensitivity and specificity.
False positive reactions in the presence of rheumatoid factor or anti-nuclear antibodies can be observed.
b / HAPS (Solid Phase Hemagglutination Assay) test or IgM immunocaptation:
This technique is simpler, more sensitive and more specific than the last.
The principle of the test is the capture of the IgM anti-human IgM monoclonal antibody (μ chains) attached to the inner surface of the wells of a microtiter plate. Test sera are distributed in the wells. During the incubation time, the IgM antitreponemal possibly present in the serum is captured in the wells. The presence of IgM results, after washing, by the agglutination of RBC sensitized with a treponemal antigen. In the absence of IgM, there sedimentation of erythrocytes.
Search IgM allows to locate the age of infection, especially in the absence of clinical signs. The presence of IgM is the best sign of disease activity. IgM antibodies are the first to appear and, if untreated, can persist until the end of the secondary period, about 2 years. Three situations can be observed:
– IgM positive and negative TPI: primary syphilis
– Positive IgM and positive TPI: secondary syphilis
– Negative IgM and positive TPI: latent syphilis may, in the absence of treatment, progress to tertiary syphilis.
B – antibodies title Evolution:
The antibody titer is the greatest serum dilution giving a patient a positive reaction.
– Primary syphilis
– The antibodies detected by FTA-Abs. appear the first, 5-8 days after the chancre, about a month after the contagion (Figure 1).
– TPHA positive is about 12 days after the chancre.
– The reagin, detected by Kline and VDRL, appear about 20 days after the chancre is 5 to 6 weeks after the contagion. After early treatment, the antibodies négativent few weeks. The immobilisines detected by the test of Nelson, may not be positive (Figure 2).
– Secondary Syphilis
All reactions were strongly positive. The immobilisines appear at the beginning of second period, about two months after the contagion. It is the latter antibodies is negated in the treatment effect.
– Congenital syphilis
Treponemes can cross the placental barrier. The birth of a child to a mother with positive serology imposes a serological study of cord blood. Differentiation of IgG and IgM is through immunofluorescence.
The presence of IgM is evidence of congenital syphilis. IgM does not cross the placenta, they have been developed by the infected newborn. IgG crosses the placenta. So it can be passively transferred antibodies from the mother. If the child is not contaminated, these antibodies have been transmitted to disappear in a few months.
– Antibodies in the CSF
Antibodies can be found in the CSF during neurosyphilis and sometimes during the secondary period. Their title is still lower than that of serum antibodies.
– Serology of the African
Serology does not distinguish between the different treponematoses. Positive serology is often related to a non-Aboriginal former venereal infection that poses no threat of contamination or complication. Under these conditions, no therapy is warranted. But regular clinical and serological surveillance is necessary because venereal syphilis recent is always possible.
– Latent syphilis
A slow decrease in antibody levels occurs spontaneously. The cardiolipidiques antibodies may disappear completely. The specific treponemal antibodies persist at low rates.
– Post treatment
The antibodies diminish more quickly that treatment early.
The reagin are the first affected by the treatment, hence the interest of their assay to monitor the effectiveness of treatment.
If syphilis has been evolving for more than 6 months, it may be difficult to obtain negativity treponemal reactions. The persistence of a “serological scar” does not protect against recontamination resulting in a new increase in antibody titer.
VII – TREATMENT:
A – Curative treatment:
– T. pallidum is always sensitive to penicillin G.
Benzathine penicillin G or penicillin G procame molecules are recommended today. The administration methods vary depending on the stage of syphilis. Penicillin G is very active treponemes actively multiplying the primary phase or second phase. It is less active on treponemes that multiply little in the tertiary syphilis lesions.
– In patients allergic to penicillin, erythromycin or tetracyclines are used.
– A Herxheimer reaction may appear in the hours following the start of antibiotic treatment. It is manifested by malaise, and worsening of symptoms and allergic observed mostly at the secondary stage.
It seems to be due to a secondary allergic reaction to the release of constituents of the bacterial body during lysis of treponemes.
B – Prevention:
As there is no vaccine for now, prevention is based on early, clinical and serological screening of the disease and the treatment of patients to quickly sterilize their rich lesions treponemes. It is difficult to control the spread of syphilis.This requires identifying and addressing any new cases partners.
OTHER treponemes:
I – TREPONEMA LOSS NUE:
Treponema pertenue is now considered a subspecies of T. pallidum. The bacteria causes yaws, tropical countries disease characterized by the appearance on the skin swelling (or yaws) with granular surface having the appearance of a raspberry. Late lesions can reach the bone, but yaws is milder than syphilis and visceral complications are rare. The transmission is not venereal. It is done through various contacts, often in childhood, and is favored by poor hygiene.
II – TREPONEMA carateum:
T. carateum is responsible or pinta pinta observed in Central and South America. This is a non-venereal infection characterized by erythematous, scaly skin lesions that reach the hands, feet and scalp. Visceral complications are rare.
Infections T. pallidum, T. pertenue and T. carateum can not be distinguished from each other by serological tests.
III – treponemes PATHOGENIC FOR ANIMAL:
T. hyodysenteriae is responsible for diarrheic syndromes in pigs. It can be grown anaerobically.
T. paraluiscuniculi is responsible for a venereal infection of the rabbit.


You must be logged in to post a comment.