DEFINITIONS AND CLASSIFICATION:
The family Vibrionaceae:
 It includes gram-negative bacilli, mobile or mixed with polar cilia, optional aero-anaerobic growing on ordinary media, reducing nitrate to nitrite, fermenting carbohydrates and giving a positive oxidase reaction.
It includes gram-negative bacilli, mobile or mixed with polar cilia, optional aero-anaerobic growing on ordinary media, reducing nitrate to nitrite, fermenting carbohydrates and giving a positive oxidase reaction.
It consists of four genera: Vibrio Plesiomonas, Aeromonas,
Photobacterium. The Vibrionaceae are aquatic bacteria.The species of the genera Vibrio, Aeromonas, Plesiomonas are encountered in human pathology.
Bacteria of the genus Photobacterium are bacteria in the environment.
The table below shows the main distinguishing characteristics of these four types.
The genus Vibrio:
The genus Vibrio is now well individualized, firstly genres listed above, the other Campylobacter and Spirillum through morphological criteria, metabolic and GC%., Campylobacter (28-35%), Spirillum ( 36-65%)
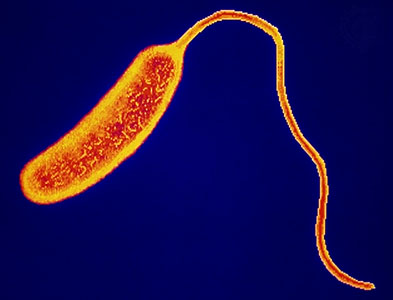
Vibrio are Gram negative bacteria generally isolated, straight or curved, rather short (1.5 to 3.0 | im), sometimes frankly coccobacillary.
When grown in liquid media, they are movable polar flagella surrounded by a sheath, or more rarely monotriches multitriches. In solid media, co-existence can be a double ciliature system; with the presence, in addition to polar flagella inserting bare lateral flagella, shorter wavelength than the previous. This mixed ciliature is often accompanied by invasion phenomenon (swarming).
Chemo-organotrophic, facultative anaerobes capable of respiratory and fermentative metabolism does not denitrify nor fix nitrogen.
Vibrio have no specific nutritional requirement: they are isolated from ordinary backgrounds. Growth is abundant in simple PEPTONES environments. But halophilic species sodium need for optimal growth, unlike halotolerant species requiring only low concentrations of NaCl.
Culture temperature: 18-38 ° C, in a pH range between 6 and 9.
We distinguish halotolerant species
– V. cholerae
– V. cholerae non 0: 1 or NC (non-cholera) or NAG (not by the polyvalent serum agglutinating 0: 1).
– V. mimicus
We distinguish halophilic species
– V. fluvialis – V. damsela
– V. metschnikovii – V. hollisae
– V. anguillarum, V. vulnificus – V. furnissii
– V. parahaemolyticus
– V.fischeri, alginolyticus, costicolus …
Another distinction can be made according to whether or not species are found in human pathology:
– Either as pathogenic for humans: V. cholerae, V. parahaemolyticus
– Either as saprophytes or opportunistic:
V. alginolyticus V. V. fluvialis metschnikovii
V. V. mimicus furnisii V. vulnificus
V. V. damsela hollisae
Vibrio cholerae:
This is the type species of the genus Vibrio.
HISTORY:
Cholera was until 1817 an endemic and epidemic disease limited to the Ganges delta with some inroads in China and in Southeast Asia.
From 1817 develops the first six pandemics due to classical vibrio. It was during the fifth pandemic Koch discovered in Calcutta (1884) the agent of cholera, “Komma Bacillus”.
Between 1910 and 1960, apart from a few epidemics (Egypt 1957), cholera seemed limited again in India.
In 1961, developed the seventh pandemic whose origin was located in the archipelago of Sulawesi (Indonesia). It is due to a V. cholerae a particular biotype El Tor. This biotype isolated for the first time in 1905 at the El Tor Lazaretto in Sinai had previously been considered pathogenic and non-epidemic. Since then, this strain has spread in Southeast Asia, the Middle East and the African continent (North Africa, Black Africa …), where he continues. The South American continent is currently affected by this pandemic (Peru cholera epidemic in 1991).
Vibrio cholerae classical reappeared in 1979 in Bangladesh. Isolation from 1974 to Guam agglutinating strains by the antiserum 0: 1, but non-toxigenic, was recognized alongside V. cholerae toxigenic all 0: 1 (2 biotypes: classic and El Tor), the existence of:
– V. cholerae 0: 1 atypical (the external environment) non-toxigenic.
– V. cholerae non-0: l (non agglutinating with 0: 1) already known to produce toxins cause diarrhea.
I – HABITAT AND EPIDEMIOLOGY:
The cholera agent is removed in large quantities by the patients in the stool, and can we find of 106-108 vibrios per ml of feces. It is also present in vomit. One can find V. cholerae in the environment. Relatively fragile, ephemeral germ persists in the waters of ponds or rivers. Its survival is prolonged in salt water (lagoon, …); it can survive more than 15 days.
It can also persist in some fresh foods (milk, fish …) for more than two weeks.
Man is the main reservoir for cholera vibrio, whether sick or bearer “healthy”. The vibrio is usually found in 6 to 10 days from the wearer, sometimes longer (chronic carrier). Contamination can be primarily through direct hand contact with a carrier and especially with a sick or dead. Recent work has demonstrated the existence of a natural ecological niche (next to the human reservoir). Estuarine waters and zooplankton (USA, Europe, India …) in it, are a natural reservoir of V. especially non cholerae 0: 1, but sometimes even 0: 1. The infected zooplankton can be consumed by seafood (shellfish, shrimp, crab and fish) and contaminate; these might then be the cause of sporadic cases. Further, in an adverse environment, the cell V. cholerae are able to turn into potentially pathogenic filterable microvibrions.
In dry areas, the transmission is only human to human. In wet areas (coastal, lagoon or river) transmission is mixed, and water-human.
In dry areas, outbreaks are more explosive, may affect 30 or even 70% of the population.
The circumstances favoring the spread of the disease are related to low socioeconomic level and especially the poor stand conditions.
Some cases of cholera are reported annually in France in travelers from affected countries.
Wednesday, 3 September 1986 ALGERIA
Cholera has claimed dozens of lives.
Algiers – Many cholera outbreaks occurred in different parts of Algeria, causing dozens of casualties among more than a thousand cases reported in the whole country since the beginning of the summer. No official information was given about the appearance of the disease, which causes the most alarming rumors among the population.
Cholera has affected most parts of the country, including the capital, medical sources indicate that, however, refuse to speak of an epidemic. Outbreaks of meningitis and typhoid were also identified, in smaller numbers, however.These diseases, which appear every year, took larger proportions in favor of been particularly challenging, marked by an unprecedented wave of heat, which has aggravated the already precarious hygiene conditions in the countryside and the neighborhoods major cities.
In some cities of the interior, which suffer from lack of water, the temperature has exceeded forty degrees for more than a month, whereas in Algiers itself, where work is in progress to renovate a pipeline network decrepit, daily water cuts in some areas are frequent and often lengthy.
The Algerian press calls people to follow certain rules of hygiene to protect against the diseases that it does not say they have been victims. She also slammed officials at the municipal level, who have not taken the necessary preventive measures by not putting bleach in drinking water supplies. These tips seem to have been followed since, including individuals, since this product is rare today among druggists – (. AFP)
II – PATHOPHYSIOLOGY:
After massively crossed the gastric barrier, vibrios multiply rapidly in the intestine; they pass through the mucus layer and adhere to enterocytes by their attachment antigens. The released enterotoxin causes the table of cholera.
Cholera symptoms are related to a fantastic loss of fluids and electrolytes by the intestine. The daily volume of stool may exceed 20 liters and composition of feces is substantially isotonic.
This leak fluid is not due to an invasion of enterocytes of the intestinal mucosa (no mucosal injury, no copro-leukocytes, no fever, negative blood cultures), but the production of enterotoxin CT (CT : cholera toxin) which causes the increase of cyclic AMP levels in enterocytes causing leakage of water and electrolytes into the intestinal lumen.
This mechanism of action is also observed that the LT toxin (close antigenically to the toxin CT) E. coli ETEC IgG and IgA in the gut may have a neutralizing effect on the seed and its toxin.
Diarrhea caused by Vibrio non-0: l are caused either by their cholera toxin, or by analogous to those of E enterotoxins. coli.
III – PATHOGENICITY:
A – Experimental:
1. In animals:
It is impossible to reproduce cholera in adult animals after administration of V. cholerae per os. By cons, administered by this route in newborn animals (rabbit, dog) it is possible to reproduce the disease.
By injecting the toxin CT (about 1 pg) into ligated loops of rabbits, fluid leakage to the lumen is observed. This is achieved as with the culture the culture filtrate of V. cholerae. As the toxin LT E. coli, exotoxin V. cytotonic choleraeproduces an effect on cells Yl adrenal or CHO (Chinese hamster ovary cells).
2. In men:
USA tests were performed on volunteers ingesting strains of V. cholerae 0: 1
– Must 108-1011 germs to cause severe diarrhea in 50% of volunteers;
– By cons, if oral administration is accompanied bicarbonate, 104 bacteria are sufficient to cause severe diarrhea in 70% of recipients.
Indeed, normal gastric acidity destroyed vibrios. The hypochloremia in malnutrition states may also explain the intestinal colonization.
Only certain strains not 0: 1 may produce experimental diarrhea in volunteers but at doses of 109.
B – Natural:
1. cholera due to V. cholerae 0: 1
Cholera is a strictly human disease. The incubation period varies from a few hours to 5 days depending on the infecting dose.
CHOLERA IN 1989 IN THE WORLD
1.1 Severe forms.:
They realize a typical table with a sudden onset dominated by epigastric and abdominal pain, malaise and diarrhea quickly resulting in significant fluid loss with risk of acute dehydration.
At the state phase diarrhea is characterized by watery diarrhea made of clear liquid with whitish flakes, “rice water” appearance. They are odorless.
The number of bowel movements is variable from 10 to 50 bowel movements per day (3 to 15 liters, can be eliminated in 24 hours).
The stools are emitted uncontrollable manner; the patient has muscle cramps associated with electrolyte losses.
This table is not accompanied by fever, but vomiting are common.
In the absence of rapid and massive rehydration, the disease progresses to a cardiovascular collapse with anuria and acidosis.
1. 2. Benign forms:
They are not exceptional with simple diarrhea (1-20 stools per day), fecal stool, abdominal pain, vomiting and no moderate or no dehydration.
1.3. Atypical forms:
They see themselves especially in children, can give pseudoméningées forms.
In adults older or debilitated cases one may encounter “dry cholera.” Death occurs before the onset of diarrhea. Of typhoid forms can meet.
If cholera is treated, the mortality is 1 to 5%; against by, in the absence of treatment, it exceeds 50% of cases.
2. Infections Vibrio cholerae non-0′.l
Serotypes of V. cholerae non-0: s are responsible for digestive diseases: gastroenteritis, diarrhea and cholera-simple.
Extra-intestinal manifestations are observed especially in immunocompromised.
Infections of wounds or ear follow contact with seawater.
IV – BACTERIOLOGICAL CHARACTERS:
A – Morphology and cropping characters:
– Classically: Gram-negative bacilli, curved comma 2 pm / 0.5 | Jm, isolated, sometimes grouped by two or more movable single polar eyelash, non-spore forming, not encapsulated.
– Atypical morphologies can be observed: spheres aspects pears, long forms, missing bend or immobile forms.
– V. cholerae preferential aerobic metabolism, facultative anaerobic. H is undemanding optimum temperature 30-40 ° C, resistant to 4 ° C.
. pH 7.6 to 9.6 tolerated, supports alkaline pH (isolation media)
. salt tolerant (0.5-7% NaCl)
. resistant to bile, bile salts and surfactants (circles in Teepol)
– Culture. liquids: rapid culture with sail surface
. solid media: in 24 hours, flat and transparent colonies, greyish, non iridescent appearance by obliquely.
B – biochemical characters:
– Respiratory Metabolism oxidase (+) Catalase (+), nitrate reductase (+)
– Carbohydrate metabolism:
. glucose (+) fermented without gas, sucrose (+)
. lactose (-) (or slow), ONPG (+), arabinose (-)
. VP (-) to classical biotype, (+) El Tor
– Protein metabolism:
. gelatin (+), indole (+). In peptone water containing nitrates, the simultaneous presence of nitrite and indole product in the presence of H2SO4 the appearance of a pink color or “cholera Roth”. This historic reaction is not specific.
. LDC (+), ODC (+), DHA (-)
– Lipid metabolism:
. Esterase (+), lecithinase (+).
– Hemolysis of red blood cells varies with the animal species and the biotype.
V. cholerae is sensitive to the compound vibriostatic 0/129 (2.4 diamino-6,7 diisopropylptéridine) and novobiocin.
0/129 resistant strains were isolated in Zaire and Ivory Coast. It is known that in vitro resistance is transferable 0/129E. coli to V. cholerae.
The appearance of such resistance can not therefore surprise; it complicates the diagnosis.
C – Differentiation biovars:
We distinguish among the species V. two biovars cholerae, classical and El Tor.
The main differences are summarized in the table below.
Recently an oligonucleotide probe corresponding to the hly A gene encoding lliémolysine allowed to distinguish the two biovars more effectively than conventional tests.
D – antigenic Constitution:
– Ag flagellar H thermolabile protein
It is not specific and antigenic communities with other vibrios exist. Serotyping is not used in practice.
– Somatic Ag 0 thermostable polysaccharide.
There are more than 100 0 serogroups.
Pathogenic strains of V. cholerae (classical and El Tor biotype) belong to serogroup 0: 1
This serogroup 0: 1 has three antigen specificities, b, c for both classical and El Tor; the combination of antigens leads to the individualization of serotypes 3, the antigen is still common.
The Ogawa and Inaba serotypes most frequently isolated.
There antigenic communities between 0: 1 and other bacterial species (some serovars enterocohtica Yersinia, Salmonella, Brucella), leading to potential cross-reactions.
E – developed substances:
Vibrio cholerae develops many extracellular enzymes (Lecithinase, protease, neuraminidase and mucinase) that play an important role in facilitating the crossing of the mucus layer (mucinase) and coming into contact with the vibrio on the brush border of intestinal cells .
Some substances play a key role in adhesion to intestinal cells and the colonization of these. These are the pili or fimbriae, which are of two types, one of them is (TCP toxin coregulated pilus) because it is expressed at the same time that CT toxin production.
The soluble hemagglutinin (not inhibited by D-mannose and L-fucose) protease, which cleaves the polypeptide subunit of the CT toxin within the disulfide bridge in Al and A2, and a factor said accessory factor colonization (ACF) play a role as a complementary adhesion factors.
The antigen 0: 1 and the glycocalyx, intervene in fixing and adhesion of bacteria to enterocytes.
As serotype 0: 1, strains of V. cholerae non-0: the produce various extracellular enzymes: protease, neuraminidase mucinase … enterotoxin A similar to cholera toxin have been demonstrated as well as enterotoxins LT, ST, a cytolysin and a cytotoxin Shiga-like
F – cholera toxin:
It is the prototype of enterotoxins causing diarrhea by activation of adenylate cyclase (AC) of epithelial cells of the small intestine.
Cholera toxin is heat labile protein oligomeric classified in the group of real exotoxins.
The native toxin (84 kDa) consists of:
– A central subunit A (28 kDa) and
– 5 B subunits devices (11.5 kDa).
The A subunit and the B subunit are linked noncovalently.
The subunit contains two peptide chains Al (22.5 kDa) and A2 (5.5 kDa) linked by a disulfide bridge. Subunit A2 serve as the signal sequence of the translocation of the A subunit 1 in the cytoplasm.
The B subunits bind to GM1 gangliosides of the membrane surface, resulting in a conformational change in the toxin, resulting in the creation of a hydrophilic channel through which the A subunit is internalized. The germ of the neuraminidase transforms di trisialogangliosides membrane and in GM1.
Al subunit stimulates adenylate cyclase. The mechanism of action is: the membrane adenylate cyclase is stimulated by Gs-GTP complex protein; this activation ceases after the hydrolysis of GTP to GDP by the GTPase activity of the subunit of the Gs protein. Subunit ADP-ribosyl the Al subunit by inhibiting its GTPase activity. The AC driven and permanently increases considerably the level of intracellular cAMP causing a very significant water leakage by inhibition of sodium absorption and by stimulating chloride secretion.
CT: cholera toxin, GM1 = monosialoganglioside, Gd = disialoganglioside, G1 = trisialoganglioside,
AC = adenylate cyclase, Gs = stimulating regulatory subunit of AC (GTP binding protein), cm = calmodulin = PK protein kinase. It = calcium stores
1: glycohydrolase activity
2: ADP ribosyltransferase activity
3: GTPase activity
Scheme proposed by Gill DM to explain the mechanism of entry of fragment A of cholera toxin.
to; subunits B recognize their specific receptors
b; the B subunits induce a change in the conformation of the wall and inserted into the membrane of the enterocyte.
c; a hydrophilic channel is thus created that allows the intracellular passage of the A subunit
d; disulfide bridge is destroyed and the Al fragment can activate adenylate cyclase in the cytoplasm of the enterocyte.
Subunits A and B enterotoxin CT are encoded by two contiguous genes ctx A and ctx B forming an operon on the chromosome. Sequence analysis shows 75% homology between the genes ctx A and fi elt AB genes encoding the LT toxin of E. coli ETEC. Strains of V. cholerae carry multiple copies of the ctx operon B. A tox R gene responsible for the activation of the ctx operon AB control of other genes involved in virulence, TCP (pili), omp V (membrane protein) and ACF.
G – Phage:
Can be isolated in endemic areas, vibriophages from the stool of patients, healthy carriers, water sewer or rivers.
These phage allow phagetyping 14 phages are used in practice. Types III, IV, V and VI are specific to the classical biotype, types 1 and II of the El Tor biotype. Phage typing provides interesting information in epidemiology.
H – Sensitivity to antibiotics:
Realized in vitro gene transfer possible to obtain multi-resistant strains; such strains may occur spontaneously and trigger epidemics.
Of strains carrying resistance plasmid were isolated in Calcutta, but also in North Africa, Black Africa, USSR ….
Reported resistors interests include tetracyclines, sulfonamides, which poses chemoprophylaxis and cure problems.Without always achieving high levels of resistance, these strains are characterized often by simply raising the CMI and instability.
It was possible to transfer this plasmid resistance to E. coli.
Finally resistances colistin and polymyxin are conventional El Tor.
V – BACTERIOLOGICAL DIAGNOSIS:
A complete bacteriological examination is carried out in Europe and in industrialized countries before a suspected cholera but it is clear that endemic area is limited to presumptive tests.
1. The levies and transport:
-Prélèvements Of human origin: they search the cholera vibrio in stool, rectal swabs, vomiting, in samples of intestinal contents during autopsies. Blood cultures have no interest.
– Collection of the external environment:
– Waters. if slightly turbid concentration fiÏtration;
. so cloudy, mix water from the concentrated alkaline peptone water 10 times, possibly by the method of floating gauze.
– Sewer: selective media
– Food: they must be homogenized and enriched in alkaline peptone water.
The ideal is to seed the enrichment media and culture there. This is not always possible and can be deposited stool sample on blotting or filter paper and sent to the laboratory in a sealed envelope.
If possible make on site seeding alkaline or saline peptone water (2% NaCl) at pH 9, and send the screw tube in the laboratory.
2. Bacteriological examination:
a / Direct examination:
It can be suggestive if observed between slide and coverslip mobility “in fish” and monomorphic Gram Gram negative flora more or less curved.
b / Cultivation:
It is recommended (Figure 3) to seed in parallel enrichment and isolation media.
– Enrichment media can be used:
– An alkaline peptone water at 1 or 3% NaCl
– A taurocholate tellurite peptone medium.
For any medium, conducts a subculture on solid medium after 6-8 hours of incubation at 37 ° C (sometimes used a second enrichment step).
– Isolation media in parallel will be used with little or no selective media and solid selective media
-Shortly selective: nutrient agar with 0.1% Teepol. On this medium, colonies eltor are not iridescent, producing oxidase is preserved
– Selective: TCBS agar (thiosulfate-citrate-bile-sucrose). The colonies are large, yellow, convex, often green if the incubation is prolonged (El Tor).
Reacting the oxidase is random.
Other selective media exist. Include:
– Lauryl sulfate tellurite
– Deoxycholate-citrate-lactose
– Gelatin-taurocholate tellurite-Trypticase (WPTT Monsur.)
Routinely TCBS medium may be advised. It is quite selective and generally Pseudomonas etAeromonas do not grow. By cons, Proteus, bacilli spore or cocci, can grow by giving yellow colonies.
Some strains of V. cholerae can grow on agar SS and Me Conkey.
c / Identification:
Suspect colonies are identified will study at least 5 different colonies.
– Presumptive tests
– Oxidase (+), mobility (+), Gram-negative
-agglutination slide with polyvalent serum anti 0: 1; if negative resume agglutination after heating at 100 ° C for 2 hours. Then use specific sera.
These tests may be acceptable during an epidemic, but to an isolated case, the beginning or the tail of an epidemic is obtained or not agglutination, proceed to a full identification.
– Definitive diagnosis
It makes a complete gallery of identification
– Is easily deviates Pseudomonas which are aerobic, oxidase (+), and resistant to 0/129.
– Aeromonas and Plesiomonas are more difficult to remove, but they are DHA (+) and 0/129 resistant (Aeromonas) or variable (Plesiomonas) (Table I).
More difficult is the differentiation with other species of Vibrio.
The main characters for this distinction are summarized in Table III. Among the Vibrio frequently encountered in human pathology, differential diagnosis arises especially with V. parahaemolyticus (sucrose (-) ONPG (-), more tolerant to NaCl) (Figure 3).
– Diagnosis of biovar
Differentiation between classical and El Tor biotype is based on the characters shown in Table II, further El Tor is conventionally VP (+), and agglutinate chicken red blood cells unlike conventional serovar.
– Identification of the CT toxin
Only 67% of isolated cholera strains or of contacts are positive CT. The research of the toxin can be from crops in particular using commercially available kits using coagglutination or agglutination of latex particles (VET-RPLA). Use may also be of conventional ELISA techniques, or the reaction itself GM1-ELISA, or finally a technique called GERYDO inhibition hemadsorption on the ganglioside GM1; these techniques are used on crops, but developments are possible by directly searching the toxin on the stool by these processes.
– V. cholerae 0: 1 “atypical”
These are agglutinating strains polyvalent sera 0: 1, but not producing enterotoxin. They may have abnormalities compared with epidemic strains (slow fermentation of sucrose particular behavior vis-à-vis the phages). These strains are found in the waters, shellfish and sometimes in subjects without diarrhea stool.
In addition to these conventional techniques cholera diagnosis by isolation and identification of the strain, research is underway to investigate the cholera toxin not only stem, but also directly in the saddle cholera, or the gene encoding the toxin probe or polymerase chain reaction (PCR).
3. Indirect diagnosis:
Given the emergency nature of cholera, for antibodies is of no interest for diagnosis. It is only useful for monitoring immunity.
– Agglutinins are detectable from 10-15 th days. We must demand a rise in antibody or as reaching over 1/100 to bring a late presumptive diagnosis.
– The search for antibodies vibrocidal the combination vibrio + serum containing antibody + complement causes lysis of vibrios. An increase of these antibodies is observed in over 90% of cholera.
The dosage of antitoxin antibodies experiencing renewed interest because it would detect not only cholera antibodies, but also against the LT toxin of E. . al Several techniques are available: immunohémolyse radial, ELISA …
VI – TREATMENT:
A – Prevention:
1. Hygiene measures:
This is a quarantinable disease notifiable. You have to take individual and collective hygiene measures.
Boil water, cook the food. Wash hands carefully, excreta disposal, even in healthy subjects.
For the sick and the “healthy” carriers, to screen, perform isolation (5 days), disinfect linens, droppings, clothing, beds, transportation, take vis-à-vis measures corpses. Chemotherapy decreases the duration of the carrier.
2. Cholera vaccines:
After a cholera protection conferred is of the order of 90%; this makes early in 1885 Ferran devised to protect against cholera by vaccine.
Currently several types of vaccines are available.
a / vaccine containing killed vibrios (whole cell)
– Parenteral: the conventional vaccine available. It contains in each dose 4,000 million killed vibrios, Inaba and Ogawa. This vaccine gives
– Local and mild systemic reactions;
– An order of protection from 55 to 60% for 3 to 6 months; but it is not protective in young children.
– An immune response with production of antibodies circulating vibrocidal, agglutinating antibodies but no antitoxin.
– Oral: tests were taken in 1010 by vibrio / day for 5 days. Protection would be of the order of 60%.
b / Vaccines with purified components:
Toxin (toxoid)
Of the toxin may be used detoxified by:
– Formalin
– Glutaraldehyde
– Heat: The toxoid is heated to 65 ° C for 5 minutes, or better for 25 minutes to reduce the residual toxin (<1%).
Purified fraction
Dodin proposed a vaccine administered orally due to attachment factors of the bacterium to intestinal cells (small peptides) and LPS polysaccharide which is responsible for power vibriocidal induced by the vaccine.
Purified subunit B
This type of vaccine causes the appearance of intestinal IgA that persist longer if the administration is oral. This approach is interesting but insufficient. Holmgren also he proposed to combine purified subunits B and killed vibrios administered orally.
An oral cholera whole cell vaccine + B subunit reaches the end of its development, administered twice 4 weeks apart; It provides protection from 85% in the first six months and 63% over the first year. After three years, the protection is still 50%. Note that this vaccine confers significant protection, but short against diarrhea in E. colienterotoxigenic (ETEC).
c / attenuated strains of V. cholerae:
Naturally attenuated strains. Non-toxigenic V. cholerae 0: 1 does not confer protection.
Attenuated strains by mutagenesis:
– Hypotoxinogène mutant strain obtained by nitrosoguanidine 569 B (M 13) used . po It gives 60% protection, but tends to a toxin reversion.
– Other mutants, such as the Texas Star-strain (3083), which produces B subunits, but not subunit A. When usedorally it causes the appearance of vibriocidal antibodies (85% of subjects) and antitoxin ( 25%), the protection is less than 75% for 1 to 2 years. Among the disadvantages we can note a little diarrhea during vaccination, and one can imagine a possible reversion to virulence.
d / recombinant strains genetically engineered:
Different recombinant V. cholerae were used. It was possible to obtain because the genes encoding the subunits A and toxin B were sequenced; were obtained strains synthesizing only the B subunit, others no synthesizing two subunits … These vaccines are being evaluated. They confer significant protection … but we still lack hindsight to judge the results.
Another approach has been tried: the genes encoding the LPS was introduced V. cholerae in a strain of Salmonella typhi avirulent (S. typhi Ty 2), this strain EX 845 is perfectly avirulent, but proved poorly immunogenic and non-protective in volunteers.
3. Chemoprophylaxis:
It is usable only short-term prophylaxis (short stay in endemic areas). It prevents disease and removes the portage.
Sulfa-delays are used (Fanasil®) or tetracycline (doxycycline).
Monitoring of V. cholerae sensitivities to these antibiotics is essential, given the existence of resistance.
B – Curative treatment:
Properly treated cholera causes about 1% of deaths, but when it occurs in disadvantaged areas, health facilities were quickly overwhelmed in front of several dozens of daily cases. Mortality can then reach 50%.
Curative treatment includes:
– A massive rehydration parenterally by saline and bicarbonate according to the dehydration (often 5-6 liters perfused in 3-5 hours) or orally (oral rehydration solution: WHO-ORS);
– Antibiotics whose interest is often questioned. It reduces the size and duration of diarrhea and shortens the duration of the carrier. Sulfonamides used, trimethoprim-sulfamethoxazole, chloramphenicol or tetracycline (provided that the sensitivity of the epidemic strain has been verified).
Other Vibrio:
Outside V. cholerae other vibrio species have been found in humans. The main ones are described below.
VIBRIO PARAHAEMOLYTICUS
After V. cholerae is the most important species.
I – HABITAT AND PATHOGENICITY:
Bacteria in seawater in coastal waters, fish, shellfish, mollusks. Vibrio parahaemolyticus is responsible for acute diarrhea in humans, stemming from ingestion of contaminated food.
Diarrhea begins 2-6 hours after eating. Feces are often water, sometimes bloody, the temperature is low; diarrhea persists 4-7 days.
This Vibrio produce a heat-labile enterotoxin, but diarrhea mechanism is rather complex and entero-invasive combined action enterotoxin is not excluded.
II – BACTERIOLOGICAL DIAGNOSIS:
A – samples:
The bacteria can be sought from feces, fresh seafood, frozen, or water.
Research should be systematic, even in France, from the stool, if one has the notion of consecutive food poisoning from the ingestion of marine products.
B – Culture:
It is advisable as with V. cholerae to make a double seeding:
– Of enrichment media (salt peptone water 3% NaCl)
– And isolation media (TCBS)
(Enrichment media being transplanted after 6-18 hours isolation media).
Incubations culture media are at 30 ° C. Blue-green colonies on TCBS is observed. Note that these colonies can grow (slowly within 48 hours) on various media for Enterobacteriaceae (Drigalski, Mac Conkey, Hektoen, SS).
C – Body type:
Bacilli rights, rather short, very mobile by monotriche polar cilia.
D – biochemical characters:
Apart from general characteristics common to other vibrios, Vibrio this must be differentiated particularly on the one hand, of V. cholerae and V. mimicus and, secondly, of V. alginolyticus.
V. parahaemolyticus is VP (-), ONPG (-), sucrose (-), arabinose (+), while V cholerae is variable VP, ONPG (+), sucrose (+), arabinose (-), and V. alginolyticus is VP (+), ONPG (-), sucrose (+), arabinose (-). The difference with V.mimicus is the ONPG character (+) and moderate halophilic of this species.
In addition, V. parahaemolyticus tolerates 7-8% NaCl, while V alginolyticus support up to 10% NaCl.
A character is interesting to look for V. haemolyticus; it is the p hemolysis on Wagatsuma medium, supplemented with 5% human or rabbit defibrinated blood. If hemolysis is present, the strains are called “Kanagawa +” is the case of pathogenic for humans. Those from the external environment are generally “Kanagawa -” without that we know the nature of hemolysis-virulence link.
Note that the gene tdh encoding hemolysin thermostable V.parahaemolyticus has high homology with the genes encoding the hemolysin of V. cholerae non 0: 1, V. mimicus and V. hollisae suggesting a common ancestor.
E – antigenic constituents:
We recognize antigenic specificities 12 0 and 59 K. antigens Under the terms of culture, two types of flagella are observed, monotriche M or L. lophotriche There antigenic communities between flagella V. parahaemolyticus and V.alginolyticus (flagella M and L) and not with V. cholerae (flagella M).
Serotyping is not routinely performed.
F – Sensitivity to antibiotics:
The strains are resistant to ampicillin sensitive to gentamicin and tobramycin, tetracycline, chloramphenicol, and trimethoprim-sulfamethoxazole.
Vibrio alginolyticus:
I – HABITAT AND PATHOGENICITY:
It is a halophilic vibrio devoid of enteropathogenic power, which can be isolated from skin infections (ulcers, cellulitis), often as a result of contact with seawater.
II – BACTERIOLOGICAL DIAGNOSIS:
V. alginolyticus has much in common with V. cholerae apart from its halophilic character very marked. It presents as some Proteus a diffusible nature of colonies on blood agar.
Vibrio vulnificus:
I – HABITAT AND PATHOGENICITY:
V. vulnificus is a species of the marine environment. It is responsible, in humans, two types of infection: severe septicemic, occurring 24 hours after ingestion of seafood, in patients with compromised defenses (eg cirrhosis) and subsequent skin forms trauma and contact with sea water or of fish foods.
II – BACTERIOLOGICAL DIAGNOSIS:
The rapid nature ONPG positive lactose and constant resistance to colistin are the major elements of orientation that diagnosis.









You must be logged in to post a comment.