Hypercalcemia is a common biological anomaly whose causes are dominated by primary hyperparathyroidism and hypercalcemia of cancer.
The interview, clinical examination and a few laboratory tests allow the great majority of cases to identify the cause and suggest appropriate treatment.
CALCIUM METABOLISM:
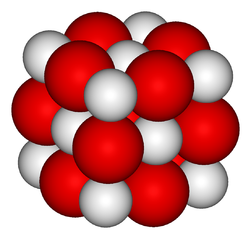
The body of a healthy adult of 70 kg contains about 25,000 mmol (1 kg) of calcium, mainly in the bone (> 99%), while less than 1% is present in the extracellular fluid (ECF) (about 20 mmol or 800 mg). However, the controlled variable is not the content of calcium in the body, but the concentration of calcium in the extracellular fluid. Serum calcium from a normal subject remains at an extremely stable value thanks to the intervention of two organs, bone and kidney. Usually the intestinal absorption of dietary calcium affects calcium levels only temporarily and is not involved in the short-term regulation of serum calcium.
The bones and kidneys are two organs that determine fasting serum calcium value. To maintain a stable serum calcium in this condition the bone releases an amount of calcium to the same amount excreted in the urine during the same time interval. This balancing serum calcium value is controlled by two hormones, parathyroid hormone (PTH) and the active metabolite of vitamin D, 1,25 (OH) 2 vitamin D or calcitriol. PTH is a peptide hormone which acts on the bone, increasing bone calcium release, and on the kidneys by increasing the tubular calcium reabsorption, thus limiting the urinary calcium loss.
Moreover, PTH stimulates the activity of the renal 1α hydroxylase and thus the production of calcitriol.
Calcitriol is a steroid hormone which binds to a specific cytosolic receptor, present in many cell types including renal tubular cells, cells of the intestinal epithelium, as well as certain bone cells. In the short term, calcitriol has an effect on bone and kidney similar to PTH. These two hormones therefore preclude the occurrence of hypocalcaemia.Indeed, a downward trend in serum calcium is immediately detected by the parathyroid cells through a specific receptor, “Calcium-sensing receptor” (CaSR). In response, the PTH secretion is increased, causing the release of bone calcium and the reduction of urinary calcium excretion, and thus the return of serum calcium levels to normal.Conversely, a tendency to rise in serum calcium (e.g., after a meal containing dairy products) causes the decrease of PTH secretion, the decrease in bone calcium release and increased urinary excretion of calcium.
A notable point is that this rapid release of calcium from the bone that is involved in the instant control of serum calcium value is based on a separate process of bone remodeling. Bone turnover, that is to say, the destruction continues activity (osteoclasts) and training (by osteoblasts) of the bone is not involved in monitoring of serum calcium, normal, because these Both activities are closely coordinated, each responsible for a flow of calcium between bone and extracellular fluid identical but opposite the resulting flow remains zero. Even in case of significant increase in bone remodeling, as can be seen in Paget’s disease, serum calcium does not vary, provided that the coupling between osteoblastic and osteoclastic these activities persists.
MECHANISM HYPERCALCEMIA:
Two types of disorders can be the cause of hypercalcemia.
Excess PTH secretion primitive:
The first type of disorder is a primitive excess PTH secretion. In this situation, the increased secretion (and concentration) of PTH leads to an increase of the bone calcium mobilization and increasing the renal tubular reabsorption of calcium filtered, the assembly necessarily resulting in an increase in serum calcium ; it stabilizes at a new value, higher than the normal value, for which the original bone inputs and outputs kidney once again match. In this new situation, calcium balance sheet and, largely, bone mineral mass remain unchanged compared to a normal situation.
Stable hypercalcemia resulting from a primitive alteration of PTH secretion is, therefore, qualified hypercalcemia “in balance”. In the new steady state, serum calcium and high serum PTH is high or normal, inappropriate to hypercalcemia.
Calciuria 24 hours may be normal or increased; in the latter case, it reflects an increase in the intestinal absorption of calcium, usually due to increased synthesis of calcitriol-induced excess PTH. In its usual form, primary hyperparathyroidism is a typical example of hypercalcemia “in balance”.
Primitive alteration of bone remodeling:
The second situation is that of a primitive alteration in bone turnover, resulting in a significant increase in net bone resorption, decrease in bone mineral mass and a negative calcium balance. This occurs when an increase in osteoclastic resorption is associated with osteoblastic bone formation decoupled (that is to say, not increased or inhibited). The large net flow of calcium in the extracellular fluid resulting exceed kidney’s ability to remove calcium, causing a progressive hypercalcemia hypercalcemia called “unbalanced”. Indeed, a decrease in extracellular volume it frequently associated due to vomiting and renal sodium loss directly due to hypercalcemia: the reduction of extracellular volume causes a decrease in glomerular filtration rate and an increase in proximal tubular reabsorption of calcium, which worsen hypercalcemia. In the presence of hypercalcemia, the serum PTH level is low, adapted, and urinary calcium is high, reflecting the excessive calcium entry into the extracellular fluid.
Hypercalcemia complicating the evolution of certain neoplasms is a typical example of hypercalcemia “unbalanced”.
DIAGNOSIS:
Measurement of serum calcium:
The controlled variable is the extracellular concentration of calcium and, more specifically, the concentration of ionized calcium. Indeed, the total serum calcium is a heterogeneous and variable comprises several fractions: about 50-55% of total serum calcium exists in ionized form (free) and is both the biologically active fraction and fraction regulated; the remainder is assumed biologically inert comprising a moiety bound to blood proteins (albumin, mainly) and a fraction bound to serum anions.
Normal values for adults, the concentration of total serum calcium are between 2.10 and 2.53 mmol / L fasting; they are moderately higher – about 0.1 mmol / L – in children and adolescents. It is important to make the measurement fasting because in postprandial period, the concentration of total calcium increases: the observed variation can reach 0.15 mmol / L in normal subjects and is higher in subjects who have absorption the pathologically increased intestinal calcium.
Although the controlled variable is the serum concentration of ionized calcium, the diagnosis of hypercalcemia can often be established on a finding of total calcium concentration abnormally high because variations in the concentration of free calcium are accompanied by parallel changes the concentration of total calcium. However, abnormalities of the concentration of serum proteins and / or faults of the acid-base state are the source of dissociations. Thus, an increase in serum albumin produced an increase in fraction of the total calcium bound to this protein, and thus an increase in serum calcium, without any change in the concentration of ionized calcium; an increase in the serum concentration of certain immunoglobulins (as in myeloma) also causes an increase in total calcium without change of ionized calcium.
Similarly, changes in the blood concentration of hydrogen ions (that is to say the extracellular pH), are capable of inducing changes in the calcium fraction bound to albumin because the hydrogen ions and the ions Ca ++ are competing for the binding to albumin.
Thus, acute alkalosis, characterized by a decrease in the extracellular concentration of hydrogen ions results in a redistribution of serum calcium between the different fractions the calcium bound to albumin increases, the free calcium and reduces the concentration of total calcium varies no. In particular, acute ventilatory alkalosis, which may appear during a painful withdrawal or in an emotional subject, causes a sudden decrease in serum ionized calcium and increased protein bound calcium. Such a change in the acid-base status is recognized by the measuring devices of ionized calcium, which have, in addition to the specific electrode for the measurement of free calcium, a pH electrode. These devices provide a calcium concentration of ionized value “fixed”, that is to say calculated for a blood pH of 7.40. The inclusion of this “corrected” value is lawful in the event of sudden disturbance of acid base status. It is obviously illegitimate if prolonged disorder of acid base status. If the situation continues alkalosis (chronic alkalosis), the concentration of ionized calcium, controlled variable, normalizes, thanks to the intervention of hormones “Calciotropic” and the concentration of total calcium increases. Opposite changes are observed in the case of extracellular acidosis.
In summary, in the absence of abnormality of the blood protein and the extracellular pH, an abnormality of the ionized calcium concentration can be detected reliably by measuring the total calcium. In contrast, in case of either of these anomalies, the direct measurement of the concentration of ionized calcium, thanks to a specific electrode, should be performed.
This measure requires some caution as to the sampling technique, the latter to be carried out on a limb at rest and at best without tourniquet to prevent changes in blood pH. When access to this measure is not possible, we can calculate a serum calcium “corrected”, knowing that each gram of albumin complex normally 0.02 to 0.025 mmol of calcium. Thus, in a subject which is measured albumin 60 g / L, it may decrease the serum calcium measured 0.4 to 0.5 mmol / L for serum calcium a “corrected”. This procedure provides a very approximate result.
Symptoms of hypercalcemia:
Whatever its cause, hypercalcemia is even better tolerated it is more moderate and, above all, she moved more slowly. This explains the large number of hypercalcemia is discovered incidentally in patients with no call sign. Symptoms attributable to hypercalcemia, where they exist, concern different devices: cardiovascular, central nervous system, digestive system, renal system, and are detailed in Table I.
Diagnosis of hypercalcemia:
Apart from the examination (specifying the age of hypercalcemia, the use of potentially hypercalcemic treatments such as lithium, thyroid hormones, alkali metal salts at high doses of calcium, vitamin A or derivatives of vitamin D, the existence of an underlying disease already known) and clinical examination, diagnosis of hypercalcemia requires a principled approach in which the measurement of certain biological variables is essential. This approach is summarized in Figure 1.
Estimation of PTH secretion:
The cornerstone of the diagnosis of hypercalcemia is the estimate of PTH secretion.
In the presence of hypercalcemia, a concentration of high or normal PTH shows its inappropriateness and allows the diagnosis of hypercalcemia parathyroid origin (primary hyperparathyroidism or, more rarely, benign familial hypercalcemia).
In contrast, a low concentration of PTH, suitable for hypercalcemia, is wearing the original diagnosis of hypercalcemia extraparathyroïdienne whose causes are dominated by cancers. PTH secretion is not clinically measurable, it is estimated by measuring serum PTH, which allows excellent separation between the values of patients with hyperparathyroidism and those with hypercalcemia of cancer or sarcoidosis. In 20 years of use, this type of measure has amply demonstrated its diagnostic performance.
Measurement of fasting urinary calcium:
Serum calcium fasting is kept stable because mandatory renal calcium loss, which then is exactly offset by a net inflow of bone-calcium. Thus, urinary calcium measured fasting estimates net bone resorption, provided that there is no intestinal origin of calcium entry at the time of measurement. This condition is generally met by imposing on the subject, in addition to a total overnight fast, an impoverished calcium diet, obtained through foreclosure milk, dairy products and mineralized drinking water, the eve of the measurement. Urinary calcium flow must be reported to creatinine flow, so as to eliminate errors in urine collection. In normal subjects, the value of this ratio (expressed in mmol / mmol) is between 0.03 and 0.36.
Measuring the concentration of PTHrP:
The hypercalcemia situations in which the concentration of serum PTH is low, adapted, are dominated by cancers. In this group, the syndrome of humoral hypercalcemia of neoplasia (HHC) account for 80% of hypercalcemia. PTH-rP (or related peptide PTH) secreted by the tumor plays a central role in this syndrome: by binding to renal and bone PTH receptor, it explains much of the biological signs that characterize this syndrome. Its measurement is therefore essential to establish the diagnosis of HHC. Furthermore, by binding to kidney PTH receptor, stimulates the production of cyclic AMP by the tubular cells, essentially proximal. The flow rate of cyclic AMP production by the tubular cells is nephrogenic cyclic AMP and dissociation between a low concentration of PTH and a high production of cyclic AMP is nephrogenic pathognomonic HHC syndrome.
Measurement of metabolites of vitamin D:
Outside the context of cancer, some hypercalcemia with low PTH secretion are due to poisoning by vitamin D (or its metabolites) or excessive endogenous production of calcitriol granulomatosis.
In daily practice, only measures the 25 (OH) vitamin D and 1,25 (OH) 2 vitamin D have an interest: the first because it represents the best estimate of the capital of vitamin D and it alone allows the diagnosis of defi cit or intoxication with vitamin D; the second because it is the biologically active hormone.
The 25 (OH) vitamin D is formed by circulating hepatic hydroxylation of cholecalciferol (vitamin D3) of endogenous or animal origin, and ergocalciferol (vitamin D2), of vegetable origin. Hepatic hydroxylation being a direct function of the amount of precursor, measurement of blood levels of 25 (OH) vitamin D reflects the state capital vitamin D2 and D3. In France, the values are considered normal in the range of 20 to 50 ng / ml (50-125 nmol / L). A high value is compatible with intoxication, knowing that the tolerance to treatment with high doses of vitamin D varies considerably from one patient to another.
The synthesis of 1,25 (OH) 2 vitamin D is primarily renal and strictly controlled by serum calcium and phosphate (which inhibit) and PTH (which stimulates). Precisely because of this close control, the measurement of the concentration of calcitriol is not an estimate of the capital vitamin D dosage indications are situations in which the synthesis is abnormally low (cit challenge hereditary synthesis of calcitriol , renal failure) or abnormally high (granulomatous idiopathic hypercalcemia in infants, lymphoma), and the suspicions of intoxication with calcitriol (Rocaltrol®) or α-calcidiol (A Alfa®). Normal values for adults are usually between 20 and 50 pg / mL (48 to 120 pmol / L) and are negatively correlated with calcium intakes. Physiologically highest values were observed in children and during pregnancy (in which there is a placental production calcitriol).
CAUSES HYPERCALCEMIA:
Original parathyroid hypercalcemia:
Primary hyperparathyroidism:
Primary hyperparathyroidism (PHPT) is the leading cause of hypercalcemia. It is defined by excessive secretion of PTH, inappropriate to the value of serum calcium. Specific complications have become rare: nephrolithiasis is only present in less than 20% of patients, fibrocystic osteitis in less than 1% and the neuromuscular syndrome has virtually disappeared.
Thus, the vast majority of patients did not sign directly attributable to PHPT at diagnosis.
Hypercalcemia is usually moderate (2.7 to 3 mM) and remains remarkably stable for years. Thus, the finding of a raised serum calcium value a few months or years ago is a very strong argument for primary hyperparathyroidism.The serum PTH concentration was high in 90% of patients. In 10% of patients, the concentration of PTH is not really high, but in the upper half of the normal values, inappropriate to hypercalcemia. Renal tubular reabsorption of phosphate is often diminished because of the PTH hypersecretion, causing hypophosphatemia in 60-70% of patients. Hypercalciuria was observed in 40-50% of patients, due to increased synthesis of calcitriol stimulates intestinal calcium absorption. The acid-base status is usually normal, hyperchloraemic metabolic acidosis being observed in cases of severe phosphate depletion or nephrocalcinosis.
Benign familial hypercalcemia (HFB):
The benign familial hypercalcemia (hypercalcemia family hypocalciuric) is much rarer than PHPT, but it is the main differential diagnosis against-shows parathyroidectomy. This is an autosomal dominant disease with high penetrance due, most often, a mutation inactivating the gene coding for CaSR. This pathology associated hypercalcemia often moderate in the first weeks of life and urinary calcium values in the low normal.
In half of the cases a moderate hypermagnesaemia is observed. The phosphate is usually normal. PTH concentrations, 25 (OH) vitamin D and 1,25 (OH) 2 vitamin D are normal. The majority of patients are asymptomatic.Nevertheless, one can observe in rare cases of complications such as acute pancreatitis, and, paradoxically, nephrolithiasis.
The treatment is conservative and the patient should not be put in low calcium diet.
Treatment with lithium:
Lithium by prolonged treatment reduces the clearance of calcium and magnesium may increase PTH secretion, causing hypercalcemia sometimes regress when treatment can be discontinued.
Hypercalcemia extraparathyroïdienne:
Hypercalcemia of cancer:
The occurrence of hypercalcemia in the development of cancer is a common event since its annual incidence was estimated at 150 cases per million inhabitants.
However, all neoplasms do not have the same ability to be complicated by hypercalcemia: this event is common in lung cancer, carcinoma of the head and neck, breast cancer and certain hematological malignancies such as multiple myeloma . In all cases, the initial mechanism of hypercalcemia is intense osteolysis resulting from a decoupling between bone formation and bone resorption. The flow of calcium in the extracellular fluid quickly exceed the renal elimination capacity, especially if there is kidney failure or increased tubular reabsorption of calcium. The hypercalcemia develops and worsens rapidly.
Humoral hypercalcemia of cancer (HHC):
Humoral hypercalcemia of cancer is a syndrome that occurs in patients with solid neoplasms, most commonly due to the production of tumor humoral circulating factor (endocrine) that causes hypercalcemia. These patients have therefore not necessarily of secondary bone localization of their malignancy.
The HHC is common during the development of squamous cell cancers of the bronchi, head and neck, but she has also been described in all types of cancers, including hematological malignancies. Hypercalcemia of rapid deterioration, poorly tolerated and is associated with a low serum PTH, adapted, in contrast to a high production of cyclic AMP nephrogenic, an increase in tubular reabsorption of calcium and a decrease in tubular reabsorption of phosphate; the blood concentration of calcitriol is normal or low and decreased intestinal absorption of calcium. The principal factor involved in the onset of HHC is the secretion by the tumor, PTH related peptide (PTH-rP).
Measuring the concentration of PTH-rp has several benefits in patients with HHC:
– It allows the diagnosis; it can be used as a tumor marker to assess tumor response to treatment;
– It predicts: life expectancy is shorter in patients with the concentration of PTH-rP is highest; moreover, a very high concentration (> 12 pmol / L) predicts a poor response to treatment with bisphosphonates.
Local malignant osteolysis:
Malignant local osteolysis (OLM) reports 20% of hypercalcemia complicating cancers. The mechanism is an increase of bone resorption, activated by a paracrine mechanism by malignant cells infiltrating the bone marrow and secrete cytokines (PTH-rP acting on the paracrine fashion interleukins 6 and 11, VEGF) acting on osteoclasts.Typically, this mechanism is observed in multiple myeloma and breast cancer. Serum calcium is high, usually normal serum phosphate and calcium excretion very high, reflecting the massive entry of bone calcium in the extracellular fluid. PTH concentrations of calcitriol and the cyclic AMP production are low, adapted to hypercalcemia.
Finally, hypercalcemia associated with excessive production and unregulated calcitriol was observed in some lymphomas.
The hypercalcemia mechanism is the same as that of granulomatosis.
Sarcoidosis and other granulomatous:
A majority of patients with sarcoidosis hypercalciuria and hypercalcemia 10-20% develop during the course of their disease. The accepted pathophysiologic mechanism involves an increase in digestive and bone-related inputs to a decrease in the kidney’s ability to excrete calcium due to renal failure linked to specific interstitial nephropathy. The increase in calcium entry is allocated to excessive and unregulated synthesis of calcitriol macrophage granulomas.1α-hydroxylase activity of macrophages is different from that normally expressed in renal tubule cells, in that it is not regulated by the concentrations of calcitriol and PTH: for this reason, macrophage synthesis of calcitriol is extremely dependent on the availability of the substrate 25 (OH) vitamin D which explains the occurrence of hypercalcemia (and hypercalciuria) is favored by sun exposure and / or ingestion of vitamin D administered to the same physiological dose.
In addition, 1α-hydroxylase activity of macrophages is inhibited by glucocorticoids, chloroquine and ketoconazole, which explains the efficacy of these treatments. Indeed, glucocorticoids, the daily dose of 40 to 60 mg of prednisone, produce a decrease in the concentration of calcitriol, normalization of serum calcium and calcium excretion in days: they are the treatment of choice of hypercalcemia granulomatous.
Poisoning by vitamin D:
Hypercalcemia can occur during a treatment, excessive doses of vitamin D or one of its metabolites. The main mechanisms are then increased intestinal calcium absorption and an increase in net bone resorption, resulting in exacerbation of the biological effects of the metabolites of vitamin D. The recommended dose of vitamin D is of the order of 400 to 800 units per day: much higher doses, of the order of 30 000 to 50 000 units per week, are necessary for the occurrence of hypercalcemia, due to the low affinity of the vitamin D and 25 hydroxyvitamin D for the receptor for vitamin D. Treatment with alfacalcidol or calcitriol, used in patients with renal osteodystrophy are frequently responsible for hypercalcemia, especially as the calcium renal excretion capacity is reduced in these patients.
Other causes:
Other causes of hypercalcemia, the pathophysiological mechanisms and their biological characteristics are listed in Table II.
TREATMENTS HYPERCALCEMIA:
The indication of the symptomatic treatment of hypercalcemia depends on several factors.
Symptomatic patient with a serum calcium or exceeds 3.25 mmol / L requires urgent treatment.
An asymptomatic patient with a serum calcium is less than 3.25 mmol / L does not require immediate treatment, except in cases where this is hypercalcemia due to cancer because it is then likely to worsen quickly. The treatment of hypercalcemia should be individualized, taking careful account of several factors: the cause of hypercalcemia, its pathogenesis, and against the existence of specific indications for a particular type of treatment.
The basic principles of treatment of hypercalcemia are correcting the extracellular volume contraction, increasing the kidney’s ability to remove calcium and decreasing calcium entry in the extracellular fluid.
Restoring normal extracellular volume by intravenous infusion of normal saline is the first step in the treatment of severe hypercalcemia. Daily administration of 3 to 6 liters of isotonic saline increases the glomerular filtration rate and decreases the renal tubular reabsorption of calcium, so a decrease in serum calcium in the range of 0.4 to 0.6 mmol / L can be achieved by treatment alone. The amount of solute administered is, of course, guided by cardiovascular tolerability.
The use of high doses of loop diuretics has often been advocated in the past.
Such treatment, which requires that the extracellular volume is normalized previously, is no longer useful, in the majority of patients, because of the effectiveness of current treatments.
The use of moderate doses (20 to 40 mg of furosemide per day) can still be useful in patients with cardiovascular tolerance to the expansion of extracellular volume is poor.
Drugs that inhibit bone resorption are an extremely effective way to treat severe hypercalcaemia, especially when it is due to cancer.
Calcitonin inhibits bone resorption and increases renal excretion of calcium.
Administered at a dose of 4 units MCR / kg every 12 hours by subcutaneous or intravenous route produces a decrease in serum calcium in a few hours, with a maximal effect obtained at 12 to 24 hours. However, the effect of calcitonin is generally moderate, serum calcium rarely falling by more than 0.5 mmol / L and above all transitory.That is why it is necessary to combine it with a treatment whose effect is extended such that administration of bisphosphonates. Bisphosphonates are synthetic analogs of pyrophosphate stable and are potent inhibitors of osteoclast activity. Administered intravenously, etidronate, clodronate, pamidronate or zoledronic acid (in ascending order of effectiveness) lead all decreased serum calcium which only appears 24 to 48 hours after initiation of treatment, maximal effect occurring during the first week. A single dose of pamidronate intravenous infusion of 4 hours (30 to 60 mg if the serum calcium is less than 3.40 mmol / L, 90 mg if it is greater than this value) is, in general, suffi cient to cause a normalization long (sometimes up to a month) in serum calcium.
Other previously used treatments (mithramycin, gallium nitrate, phosphate infusion) are also effective, but their toxicity is high which explains their disaffection.
CASES THE PROCESSING OF PRIMITIVE HYERPARATHYROIDISM:
Today, 80% of patients with diagnosed primary hyperparathyroidism are asymptomatic, that is to say the disease is not complicated by fibrocystic osteitis symptomatically calcium nephrolithiasis or classical neuromuscular syndrome.This raises legitimately question whether it is appropriate to radically treat these patients, knowing that the only treatment we can offer is the first-line surgical treatment. To answer this question, two American consensus conferences were held, the last in 2002.
Surgery is the only treatment that can be offered as first-line in patients with classic complication of primary hyperparathyroidism (osteitis fibrocystic, recurrent calcium nephrolithiasis, severe gastrointestinal complications, neuromuscular syndrome). It is also recommended for asymptomatic patients with the most severe forms of the disease, defi ned by the following criteria:
– Calcemia than 0.25 mmol / L (0.10 mg / L) upper limit of the laboratory standard; occurrence of an episode of threatening hypercalcemia;
– The 24-hour urinary calcium greater than 10 mmol (400 mg) / day;
– Reduced creatinine clearance of more than 30%;
– Osteoporosis defined by a Tscore <-2,5DS to, at least, a measurement site;
– Finally, surgical treatment is also recommended for those aged under 50 and those whose medical care is not provided.
In about 50% of patients, no surgery criterion is present at diagnosis and monitoring can be proposed. This monitoring includes six-monthly measurement of serum calcium and the annual measurement of serum creatinine and bone mineral density. Furthermore, it is necessary to advise to avoid situations that can cause an increase in serum calcium (immobilization, extracellular dehydration, vitamin D intake in excessive dosages) or bone demineralization (depleted calcium diet, vitamin D deficiency) .
Recently a CaSR agonist (Cinacalcet HCl) was introduced on the market in the field of primary hyperparathyroidism, its use is restricted to parathyroid carcinoma and patients whose prior surgical treatment resulted in failure.




You must be logged in to post a comment.