Hypokalemia is the electrolyte disorder most frequently encountered in clinical practice, including hospital.Hypokalemia below 3.5 mmol / L was found in about 20% of hospitalized patients.
Most of the time, a simple interrogation in search of iatrogenic causes makes it possible to trace the etiology, but there are sometimes more complex situations of unexplained chronic hypokalemia including Gitelman syndrome or unacknowledged taken diuretics .
PATHOPHYSIOLOGY:
The vast majority of the potassium pool of the body (about 90%) is in the intracellular situation intracellular K + concentration is estimated at 140 mmol / L against 3-5 mmol / L in the plasma sector.
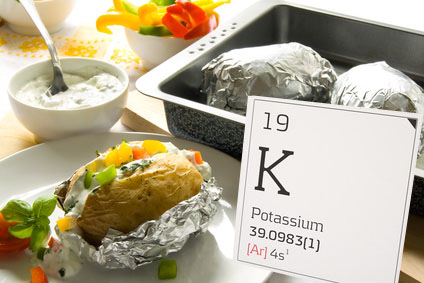
Dietary intake of K + are estimated at 100 mmol / d, mainly excreted by the kidneys.
Regulation of potassium:
Two mechanisms regulating serum potassium.
Intracellular transfer of K +:
He himself is under the control of:
– The acid-base balance. The acidosis has an output of potassium from the cell, while the induced alkalosis contrary hypokalemia;
– Activation of the Na + / K + ATPase membrane: this pump is located on the membrane of all body cells and promotes the entry of the potassium into the cell. This pump is driven by:
– Insulin
– The β2-adrenergic substances,
– Thyroid hormones,
– Aldosterone.
Tubular secretion of K +:
It is principally dependent on the renin-angiotensin-aldosterone system, resulting in an increase of urinary potassium (cortisol also has an intrinsic mineralocorticoid effect).
Complications:
Most hypokalemia are asymptomatic, particularly when moderate (between 3 and 3.5 mmol / L). The onset of clinical manifestations is mainly correlated with the speed of installation of hypokalemia and depth.
Below 3 mmol / L can appear muscle symptoms: fatigue, muscular hypotonia, constipation. Flaccid paralysis, rhabdomyolysis or paralytic ileus may occur for lower kaliémies 2.5 mmol / L.
Cardiac manifestations are mainly represented by arrhythmias.
They usually appear for lower kaliémies 2.5 mmol / L, but can apparaîtrent earlier (Box 1).
Box 1. Situations at risk of arrhythmias during hypokalemia
Treatment digitalis, quinidine
Treatments that prolong the QT interval
Underlying heart disease
Hypercalcemia
The electrocardiogram usually shows:
– First a flattening or even become negative T wave;
– Then the appearance of a U wave with a depression of ST segment; then an enlargement of the P wave, an increase in PR interval, QRS widening.
Complications are represented by supraventricular arrhythmias, ventricular premature beats, ventricular fibrillation or torsade de pointes.
Finally, in chronic hypokalaemia, may be observed polyuria syndrome and the development of chronic interstitial nephropathy.
DIAGNOSIS AND ETIOLOGY:
First, a simple examination on drug taken (diuretics, β-agonists, insulin), the existence of digestive disorders (diarrhea, vomiting), the existence of hypertension and the study of urinary potassium help simply guide the diagnosis (Box 2 and Fig. 1).
Box 2. Key elements of the etiologic diagnosis
Drug intake
Digestive disorders
High blood
Kaliuresis
Chlorurie
Extrarenal losses:
In the digestive losses, urinary potassium is usually low, below 20 mmol / d, but can sometimes be abnormally high due to extracellular dehydration and an associated secondary aldosteronism, and especially because of the chlorine cit challenge upper gastrointestinal losses. It can then steer wrongly to hypokalemia related to renal loss.
High losses digestive, stomach:
They are associated with hypochloremia and a low chlorurie less than natriuresis. Kaliuresis may be low, but is most often high:
– Prolonged gastric aspiration;
– Profuse vomiting, solicitors or not.
Lower gastrointestinal loss (diarrhea):
They usually associate with metabolic acidosis, linked to a loss of digestive bicarbonates: Acute diarrhea, villous tumor, VIPoma, Zollinger Ellison syndrome.
Disease laxatives:
Its diagnosis is sometimes difficult because laxatives is not declared:
– Women desire to lose weight;
– Diarrhea and laxative ulterior;
– Low urinary potassium.
Diagnosis is based on the finding of a colonic melanosis or the laxatives detection in stool or urine.
Skin losses:
Extensive burns.
Renal losses:
They are characterized by an abnormally high kaliuresis 24 hours, over 20 mmol / day.
The causes are distinguished primarily by the presence or absence of hypertension (Fig. 2). The diagnostic tree is summarized in Figure 3.
Apart from situations where the diagnosis is obvious (diuretics, corticosteroids, chemotherapy with cisplatin …), it should be emphasized rare causes of unexplained chronic hypokalemia.
Unspoken taken diuretics:
The land is: women, especially psychological field desire to lose weight.
The biological profile can vary depending on whether you are in a time of taking diuretics or remotely. Typically, kaliuresis is high with a metabolic alkalosis, but it may be low at a distance from the outlet.
The diagnosis is usually worn by the search for diuretics in urine. The main differential diagnoses are Gitelman syndromes (which mimics taking a thiazide) and Barrter syndrome (which mimics a hold of loop diuretics, furosemide, for example)
Vomiting ulterior:
The land is: women in anorexic profile.
Include metabolic alkalosis (loss of HCl in gastric juice) with hypochloremia, hypochlorurie and abnormally high kakiurèse (related to chlorinated deficit leak tubular level).
The “test” treatment involves hospitalization with physiological saline infusion that controls vomiting and correction of serum potassium by the simple correction chlorinated deficit.
Tubular acidosis:
Biological picture is evocative, with hyperchloraemic metabolic acidosis and normal anion gap.
Gitelman syndrome and Barrter syndrome:
These autosomal recessive disorders result both by chronic hypokalemia “unexplained” of renal origin (urinary potassium> 20 mmol / day) without hypertension.
Gitelman syndrome:
It is diagnosed in adulthood, usually accidentally, or muscle signs. Patients are usually asymptomatic despite extremely low kaliémies and cardiac complications are extremely rare. An inactivating mutation in the gene encoding the SLC 12A3 Na-Cl channel (channel that acting thiazide) of the distal convoluted tubule is responsible Electrolyte disturbances, resulting in a pattern similar to that of a thiazide:
– Hypomagnesemia;
– Low calcium excretion;
– Risk of early articular c hondrocalcinose?
Syndrome Barrter:
This is a pediatric disease, the diagnosis being carried in the neonatal period or in early childhood (polyhydramnios, stunting).
Hypokalemia is related to an inactivating mutation of a sensitive channels of loop diuretics, making the same biological array to a taking furosemide:
– No risk of urinary calcium with éphrocalcinose;
– Normal serum magnesium versus Gitelman syndrome.
Rare causes related to intracellular K + transfer:
These are the following:
– Insulin;
– Treatment with β2-agonists;
– Acute alkalosis;
– Poisoning chloroquine, theophylline;
– Family hypokalemic paralysis Westphall;
– Hyperthyroidism.
TREATMENT:
The terms depend mainly potassium supplements:
– The importance of hypokalemia (<2.7 mmol / L);
– Symptomatic character;
– The existence of an arrhythmia or an aggravating factor (Box 1).
In all three situations, hospitalization for intravenous bumping is required.
In some situations, hospitalization may be indicated etiologic purpose, especially in complicated situations such as vomiting or hidden ulterior diuretics taken.
In other cases, oral supplementation can be provided (Diffu K®, Kaleorid®, Kaleorid LP®), with a suitable diet rich in potassium (bananas, chocolate). Hypomagnesemia should be routinely detected and corrected, especially if there is a Gitelman syndrome or associate tubulopathy.




You must be logged in to post a comment.