A- Risk factors:
– Five major and independent risk factors are involved in the pathology of atherosclerosis: high cholesterol, hypertension, smoking, diabetes, coronary heredity.
– High cholesterol and smoking are paramount in the development of coronary atherosclerosis.
– Hypertension is a major risk factor for stroke (carotid atheroma)
– Smoking and diabetes are paramount in the development of arterial disease of the lower limbs.
– Dietary treatment and / or medication is likely to regress atherosclerotic lesions.
– Tobacco smoke a direct toxic effect on endothelial cells; it triggers endothelial dysfunction, LDL oxidation and NO production. It is also thrombogenic activation of the release of thromboxane A2 in platelets.
– Atherosclerosis occurs earlier in diabetics; it is also more frequent and more severe.
– Action levels (for primary prevention) are LDL cholesterol levels> 2.2 g / L when there are no other risk factor.
– The first stage of the treatment is the prescription of lifestyle and dietary rules for 3 months. If only ineffective, add the statin.
– Moderate Sports Activities and regular ® k HDL cholesterol.
B- Stable Angina of effort:
– Sometimes the pain is replaced by a respiratory blockage that abruptly slows the patient as soon as it accelerates not (the classic effort blockpnée).Note: Important: 7 out of 10 episodes are asymptomatic coronary
– Intercritical ECG: normal in over 50% of cases.When it is pathological, it can be observed: subepicardial ischemia (T wave inversion), subendocardial injury (sub-ST segment elevation)
– Classification of angina of effort CCS (Canadian Cardiovascular Society)
* Class 1: pain only appear for major efforts, sudden or prolonged
* Class 2: angina resulting in a moderate decrease of daily activity: brisk walking, climbing stairs rapidly, walking or climbing stairs after a stay in the cold, against the wind …
* Class 3: important limitation of ordinary activity, walk 2 blocks on a horizontal plane or ride a floor under normal conditions.
C- Unstable angina:
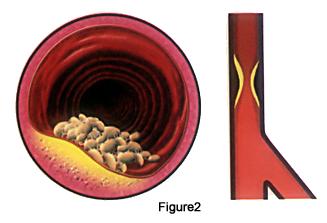
– It is due to a brutal reshuffle at a plaque Þ development of non-occlusive thrombosis in what is often associated vasospasm. This is a high evolutionary potential state; higher risk of MI.
– This is an angina attack with at least one of the following characteristics: occurs at rest is prolonged (> 20 min in the absence of taking nitroglycerin); is recent (1 month) and severe (at least class III); crescendo angina or worse.
– The ECG is normal 8 out of 10 (out of the crisis). In an epicardial ischemia can be observed (negative T wave, sharp and balanced); sometimes subendocardial lesions (in ST segment).
– Troponin does not rise (if one speaks of non-Q wave myocardial infarction).
– The pseudo normalization of a subepicardial ischemia is not a sign of improvement but rather persistent evolution.
– Unstable angina performs 3 clinical pictures:
~ * The resting angina: caution is the rule and monitoring in intensive care is desirable.
~ * Reversals angina after acute MI within 3 weeks after the initial episode (expansion threat).
~ * Angina de novo effort: it is the appearance for less than one month of severe angina, it often manifest overnight for readily modest efforts.
~ * The crescendo angina: breaking pace of a former stable angina by the sudden and rapid change of symptoms;involving changing circumstances of occurrence (minimal efforts); changing the character of the pain (k Intensity further irradiation, duration k)
D- Variant Angina:
– Clinically: spontaneous pain, without any effort intense. Prolonged pain, occurring scheduled and cyclical and relapsing, often at night (part of the night). With the possibility of syncope at the peak of the crisis.
– On the electrical level: during the crisis, significant ST segment elevation systematized encompassing the T wave with mirror image, and the wave amplitude increased R; these anomalies disappear after the crisis.
– Lack of biological necrosis stigma.
– In terms of progression: short-term serious with risk of MI and especially ventricular arrhythmias with sudden death.Justify hospitalization and emergency treatment in the ICU, as well as coronary angiography. The prognosis is favorable when processed.
– The challenge test Methergin: performed after coronary angiography which showed a normal coronary system (against-indication in case of stenosis).
E- test effort:
– He has a diagnosis and prognosis
– Main Indication: stable angina of effort. Unstable angina with pain in the previous 48 hours is a cons-indication
– The positivity criterion is the appearance of at least 85% of theoretical maximum rate (220 – age):
* A shift in more than 1 mm horizontal or descending 0,08s after point J.
* More rarely, ST segment elevation in the absence of infarction (severe injury, spasm, especially if it occurs after exercise)
* Pain that increases during exercise is less common than the sub-shift
– The sensitivity of the stress test is 75% but the specificity is low especially among women and in case of pre-existing abnormality on the ECG (valve disease, BBG, HCG, HTA)
– Some parameters have an important prognostic value and demonstrate severe triple vessel lesions or stenosis of the common trunk of the left coronary and should lead to rapid coronary angiography:
* Early Positivity
* Sub-offset> 4 mm extended to several derivations
* Slow standardization recovery
* Ventricular extrasystole to the effort
* Hypotension or absence of elevated BP during exercise
F- myocardial scintigraphy:
– Thallium 201 binds only on myocardial cells whose metabolism is normal. The sensitivity was 80% and the specificity is 90%.
– The scan enables the precise location of the ischemic territory and therefore probably artery in question
– It is performed for the diagnosis of coronary heart disease when clinical and ECG are not enough pure diagnosis. It is useless if the diagnostic evidence is provided by the ECG and / or the clinic. The stress test has no interest in the event of BBG (false positive).
– Myocardial scintigraphy with dipyridamole test (Persantine®: antiagrégant with vasodilating action on normal coronary arteries) is made if unable to make an effort.
Indications:
– Stable Angina effort (ECG unrealized crisis)
– Evaluation of the effectiveness of antianginal treatment
– After the acute phase of MI
– Rhythm disorders in the effort
Cons-indications:
– IDM acute and very recent
– Unstable angina
– Obstacle to ventricular ejection (RA, obstructive cardiomyopathy)
– Severe uncontrolled hypertension
– Trouble ventricular rhythm
– In all cases where it may be poorly tolerated (severe anemia, respiratory failure …).
G- Coronary angiography:
The indications for coronary angiography are large (especially young subjects) but should not be systematic in angina. The main indications are:
* Chronic stable angina unimproved by medical treatment
* Unstable angina at high risk; spontaneous angina
* Suspected vasospastic angina
* Immediate myocardial infarction Suites with positive stress test
* Recurrence of angina after a treaty IDM
The results of anginal disease:
– Includes forever: a detailed clinical examination, laboratory tests and atheromatous FDR; stock extension of atheromatous disease; a resting ECG; an exercise ECG and echocardiography.
– Most often (but not always) coronary angiography for accurate assessment of coronary lesions for possible revascularization
– When in doubt: Holter ECG; isotopic examinations; stress echocardiography (dobutamine)
H- Treatment:
Angina stable exercise: The crisis -> nitroglycerin lingual per

You must be logged in to post a comment.