1- Myocardial carotid:
+ Carotid:
Optic-pyramidal syndrome with monocular blindness ipsilateral to the occlusion (ophthalmic artery) and contralateral hemiplegia.
+ Superficial Sylvian (frontal and ascending parietal convexity):
– Hemiplegia contralateral to facial predominance brachiocephalic + sensory disturbances in the paralyzed area
– Lateral homonymous hemianopia (HLH) often incomplete
– If major or dominant hemisphere (left) motor aphasia Broca if frontal damage (anterior infarction); Wernicke aphasia understand if posterior infarction (temporal reached). Apraxia (parietal involvement); Gerstmann (posterior parietal damage) combining acalculie, agraphia, finger agnosia and not left right distinction.
– If the minor hemisphere -> Anton-Babinski syndrome: anosognosia (does not recognize his disorder);hémiasomatognosie (does not recognize his paralyzed side of the body); indifference (Anosodiaphoria)
+ Deep Sylvian (internal capsule):
– Proportional massive Hemiplegia
– Hemianesthesia fickle; no HLH
+ Total Sylvian:
– Hemiplegia proportional + + hemianesthesia massive HLH (global aphasia if the dominant hemisphere)
– Combined deviation of the head and eyes toward the lesion (reaching the frontal eye-céphalogyre area) ->
NB: If bilateral MCA infarction -> pseudobulbar affect
+ Brain previous:
– Hemiplegia predominantly contralateral femoral “monoplegia thigh” (reaching the paracentral lobule)
– Sensory Disorders hémicorps predominant contralateral lower limb
– Ideomotor apraxia
– Front Syndrome (grasping reflex)
– If bilateral and complete: akinetic mutism.
+ Previous Choroidal:
Massive and proportional hemiplegia (posterior limb of the internal capsule) with hemianesthesia fickle; HLH fickle;without aphasia.
2- Myocardial vertebrobasilar:
+ Brain post:
– Surface area: HLH often isolated with or without visual agnosia and alexia (major hemisphere) or prosopagnosia (HS minor).
– Deep Territory: thalamic syndrome (see below)
+ Thalamic (deep territory):
– Trouble sensitive to all modes of the contralateral side of the body sometimes hyperpathia (Dejerine-Rousseau syndrome).
– Cerebellar signs in the same territory
– Horner’s syndrome
+ Bilateral involvement:
– Cortical blindness (light reflex conserved)
– Memory disorders, Korsakoff’s syndrome (bilateral involvement of the internal surface of the temporal lobes).Prosopagnosia (ignorance of faces).
NB: achievement of the subthalamic nucleus (horns Luys) -> hemiballismus contralateral.
+ Brain stem (alternate syndromes):
1- Bulbar : Lateral medullary syndrome
– It is a disorder alternates sensitive CT (without hemiplegia) infarction of the lateral portion of the irrigated retro-olivary bulb by the artery of the dimple side of the bulb
– Sudden onset of vertigo with a great balance disorders + + posterior headache vomiting
– The side of the lesion: paralysis of the nerves IX and X (voice and articulation and swallowing); cerebellar hemisyndrome; vestibular syndrome with rotatory nystagmus; achievement of V (thermo-Algonkian anesthetized the hemifacial) syndrome Horner
– On the opposite side: thermo-Algonkian anesthesia hemibody respectfully deep sensitivity.
2- Stems (midbrain) Weber’s syndrome
Paralysis of the ipsilateral III + contralateral hemiplegia
3- Pons: Millard-Gubler syndrome
Paralysis of the ipsilateral VII + hemiplegia of the contralateral side of the body
NB: Locked-in syndrome
– Bilateral Myocardial foot of the protuberance
– Quadriplegia + facial diplegia. The only possible movements are the verticality of the eyes and eyelid movements (the only act strictly stem -> movement of the eyelid III).
3- transient ischemic attack (TIA):
Focal loss of the brain or retinal function for less than 24 hours.
+ Carotid TIA:
They can provide 4 type deficits:
– Blindness amaurosis (amaurosis fugax) reflects ischemia in the territory of the ophthalmic artery, a branch of the internal carotid.
– Aphasia Breach of the dominant hemisphere
– Motor deficit (the brachiocephalic facial deficit is very suggestive of carotid disease) and / sensory ouTroubles
Note: The optical-pyramidal syndrome is pathognomonic of carotid disease and associates: ipsilateral monocular blindness and contralateral hemiplegia.
+ Vertebrobasilar TIA:
Drops-attacks;
bilateral sensorimotor deficit () or rocking;
balance disorders (ataxia); visual disturbances (HLH if unilateral occipital ischemia, cortical blindness if bilateral ischemia). Other (diplopia, dizziness, dysarthria, faintness).
Note:
– Systematic Dextro to any sudden neurological signs
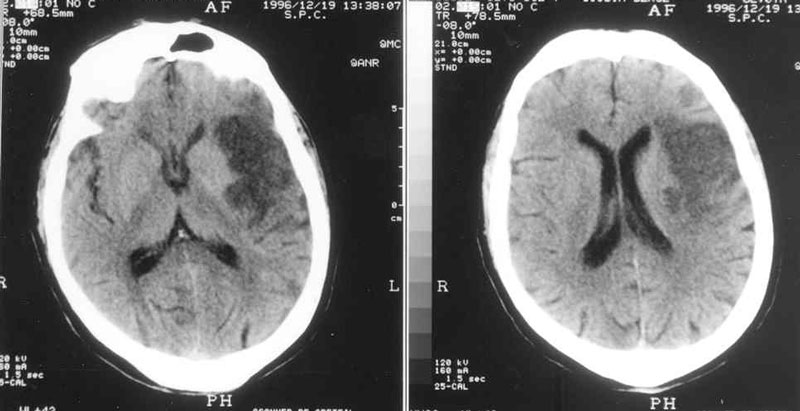
– The brain scan is systematic (differential diagnosis: brain tumors)
4- brain Gaps:
Four tables are suggestive of neurological deficiencies:
– Pure motor hemiplegia (internal capsule)
– Hypoesthesia or paresthesia of an hémicorps or cheiro-oral predominance: thalamic gap
– Dysarthria + clumsy hand (foot protrusion)
– + Ataxia hemiparesis: pyramidal signs and corticocérébelleuse route is a shortcoming of the corona radiata (hemispheric white matter) or pontine gap.
The incomplete state (multiple gaps) is responsible for a pseudobulbar syndrome associating; disorder of phonation and swallowing + spasmodic laughter and tears. Often present signs bilateral pyramidal syndrome + walk in small steps; sphincter disorders; vascular dementia.
5- stroke by venous thrombosis:
– Especially the superior sagittal sinus thrombosis (otitis, sinusitis, malignant staphylococcal infection of the face)
– Table of HIC headache vomiting + + papilledema and impaired consciousness
– Focal signs: cerebral infarction does not correspond to an arterial territory, frequent bleeding, unilateral or bilateral;toggle hemiplegia (very evocative)
– Epileptic seizures
6- Treatment:
– Aspirin in the acute phase: 100 to 1000 mg / d IV. Beneficial effect on mortality and disability; reduces the risk of recurrence.
– Anticoagulants: After eliminating bleeding (systematic scanner). Heparin (300 to 500 IU / kg / day) or LMWH two sc injections / d.
* Indications: AIT repeatedly (threatening syndrome), cardiac embolism, dissection of the cerebral arteries; cerebral thrombophlebitis.
* CI: massive stroke; loss of consciousness; very old person; Poorly controlled hypertension
* The long-term VKA are indicated in cases of heart disease or embolic cerebral thrombophlebitis.
– Thrombolysis: rt-PA (Actilyse) IV for ischemic stroke within 3 hours
– Blood TA frequently rises initial stage of stroke. At very high BP (systolic> 220 or diastolic> 120) and / or heart or kidney repercussions => progressive fall in BP
– Early Physiotherapy
Anatomy
Vascularization of the brain is provided by 4 arteries: internal carotid and two vertebral arteries 2. It is a protected traffic as the 4 arteries are uniting to form an anastomotic circle (circle of Willis). Occlusion of one of these arteries can theoretically have no consequences for the brain.
The vertebral arteries unite to form the basilar artery and irrigate the brain stem, cerebellum and occipital-temporal lobes. The branches of division of vertebrobasilar system are: the anterior spinal artery, cerebellar artery and posterior cerebral arteries.
The carotid system for major side branches: the anterior choroidal artery, ophthalmic artery, anterior cerebral artery, the middle cerebral artery.
The two systems communicate by posterior communicating arteries. The anterior communicating artery provides communication between the right and left carotid systems.
Physiology: cerebral blood flow is an average of 50 mL / min / 100g brain. Flow control is through vasodilation and vasoconstriction capacity of cerebral arteries constituting a real cerebral blood reserve. The blood oxygen extraction by the brain can be increased if necessary.