AURICULAR EXTRASYSTOLES
AURICULAR EXTRASYSTOLES
CLINICAL SIGNS:
* none or palpitations or feeling of heart failure.
* sometimes lipothymia in the elderly if in bursts.
ETIOLOGY:
* idiopathic, benign.
* hyperthyroidism.
* mitral valve prolapse, mitral stenosis, hypertension.
* atrial disease.
ADDITIONAL TESTS:
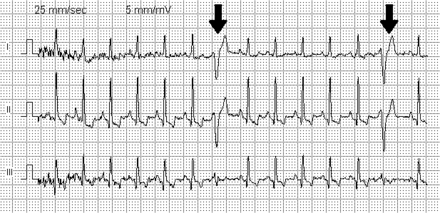
* ECG :
QRS premature and normal configuration (duration 0.08 sec).
– sometimes branch block appearance.
The wave P ‘precedes QRS, but its morphology is altered:
– if low atrial: negative P ‘wave in D2, D3, VF.
– if left atrial: negative P ‘wave in D1, VL.
– if right atrial: appearance close to the P wave.
– space P’R is normal or elongated. The space PP ‘is shorter than the space PP.
They can be isolated, twinned, trigeminal, in doublets or triplets.
– if they are numerous, they can make fear a passage in AC / FA.
Trap: P wave masked by the previous T wave followed by a ventricular aberration that resembles a VES.
– in the “wandering” pacemaker: PP ‘> PP.
* blood ionogram: look for hypokalemia.
* TSH.
echocardiography and holter ECG in a second time.
TREATMENT:
* none or sedatives if necessary: benzodiazepines or Atarax or Natisedine per os.
* if badly tolerated:
– Stop digitalis, correct the cause.
– oxygen therapy.
– if there is a risk of passing into complete arrhythmia by atrial fibrillation:
– heparinotherapy.
– and antiarrhythmics: Cordarone, betablocker, Sotalex.
JUNCTION EXTRASYSTOLES
CLINICAL SIGNS:
* idem.
ETIOLOGY:
* idem.
ADDITIONAL TESTS:
* ECG :
– normal configuration QRS (duration 0.08 s).
– the P ‘wave is negative at D2, D3, VF, it precedes (P’R <0.12 s) or follows QRS (RP’ <0.12 s), sometimes P-wave absent, included in the QRS .
* blood ionogram: look for hypokalemia, TSH.
echocardiography and holter ECG in a second time.
TREATMENT:
* none or sedatives: Benzodiazepines, Atarax, Natisedine per os.
* if poorly tolerated: oxygen therapy and antiarrhythmics, beta-blockers.
VENTRICULAR EXTRASYSTOLES
CLINICAL SIGNS:
* idem.
* onset or aggravation with the effort so serious.
ETIOLOGY:
* idiopathic
* underlying cardiopathy , ischemic or not.
* hypokalemia, dysthyroidism, hypoxia, severe infection.
* abuse of alcohol, coffee, tea, narcotics.
* anxiety.
iatrogenic: digitalis, theophylline, betamimetic, antiarrhythmic.
DIAGNOSTIC TESTS:
* scope.
* ECG :
– broad QRS, not preceded by P wave and followed by a T wave opposite to that of QRS.
– may be bigeminal, trigeminal, interpolated, compensating or shifting.
– if aspect of BBD: origin in left ventricle, if aspect of BBG: origin in right ventricle.
– serious ventricular extrasystoles:
– polymorphism: more than 2 different morphologies on the same route.
– early onset with respect to the previous T wave.
– wide> 0.18 s.
– QT long.
– numerous, increasing with heart rate, or in bursts.
* blood ionogram, TSH.
* holter ECG, echocardiography in a second time.
TREATMENT:
* delete or correct the cause.
* sedatives if necessary: oral benzodiazepines or Atarax 25 or Natisedine.
* if benign ventricular premature beats poorly tolerated:
– Tenorine: ½ -1 cp / day or Sotalex 160: ½ -1 cp / d.
– or Isoptine 120: 1 cp x 2-3 / d.
* if severe ventricular extrasystoles:
– Isuprel if bradycardia and long QT.
– or Xylocaine: 1 mg / kg IV slow then 1 to 2 mg / min to the electric syringe if myocardial ischemia.
– or Cordarone: 5 mg / kg IV slow then 150 mg / 6 h. to the electric syringe.