1- Early complications:
A- rhythm disorders (very common in the early hours):
– Sinus bradycardia, especially in cases of inferior infarction with sweat, pallor, fall in blood pressure (vagal syndrome); reversible under atropine and fluid replacement.
– Sinus tachycardia: common suggestive of left ventricular failure, extensive necrosis.
– AC / FA: frequent and transient risk of embolism. Atrial extension of necrosis or hemodynamic decompensation.
– Ventricular extrasystoles (VES): very common, especially in cases of recanalization (thrombolysis); requires immediate treatment if they are numerous, polymorphic, burst, near the T wave (appearance R / T).
– Ventricular tachycardia: wide QRS complex tachycardia regularly with P wave dissociated fusion events and capturing.
– Ventricular fibrillation
– Idioventricular rhythm accelerated (RIVA) performs a tachycardia with wide QRS appearance ventricular rate <120 / min; usually well tolerated and no adverse prognostic significance.
– Reperfusion syndrome: combines ESV, TV, RIVA sometimes bradycardia.
B- Conduction abnormalities:
– Sinoatrial block: especially in cases of inferior infarction; favored by the beta-blocker treatment; often poorly tolerated.
– BAV at a lower necrosis: progressive installation; well tolerated; QRS end; Relatively fast CF; Transitional good prognosis (reflecting edematous reaction).
– AVB during a previous necrosis: sudden onset; reflecting a low exhaust located; complex and wide QRS slow; risk of syncope; severe prognosis as reflecting an extensive infarction.
C- Heart failure:
– Killip classification (VIP):
* Class I: absence of crackles and B3
* Class II: pulmonary crackles dating back to mid-field or B3
* Class III: crackles back beyond with OAP
* Class IV: cardiogenic shock
– Primary Cardiogenic shock => necrosis> 40%
– Right ventricular failure (rare); she look for: a rupture of the interventricular septum, pulmonary embolism, pericardial tamponade; right ventricular extension of a lower infarction.
D- Mechanical complications:
– Septal rupture with CIV: complicates prior or infero- basal infarction. Holosystolic breath red circle and signs of acute congestive heart failure.
– Break or malfunction of ischemic mitral pillar: especially in cases of inferior infarction; shock, apexo-axillary systolic murmur, OAP. Capillary wave V at catheterization.
– Out of the free LV wall pain, shock, cracking syndrome (reappearance of a current above-epicardial injury?);éltromécanique dissociation;
2- Late complications:
– Dressler’s syndrome: after the third week; inspiratory pain and recurrent fever, joint pain, pericardial friction; common pleural effusion;mild but long evolution NSAID with the possibility of relapse.
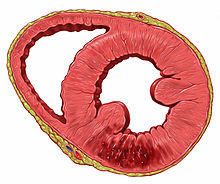
– Ventricular Aneurysm: especially after anterior-apical infarction;diagnosed by double shock peak on palpation (inconstant); persistent lesion current subepicardial after 3 weeks (ST segment elevation). Risk of thrombus adhering; peripheral embolism; severe ventricular rhythm disorders; heart failure, rupture.
– Recurrent angina: requires coronary angiography for possible surgery
– Scapulohumeral periarthritis (shoulder-hand syndrome) -> dystrophy?

You must be logged in to post a comment.