1- Summary:
Pregnancy is a physiological condition favoring the occurrence of venous thrombosis, and sometimes unmasking coagulopathy.
Due to the presence of the fetus, suspicion of venous thromboembolism in pregnant women poses a double challenge to the clinician: a diagnostic challenge, spoke before a set of clinical and confirmed to be using d ‘imaging tests radiating least possible, but also a challenge related to anticoagulant therapy to be devoid of thératogène effect.
Outside a serious context, the only chronic treatment currently approved is heparin syringe pump.
Nonetheless, many obstacles related to mode of administration and supervision of this treatment it currently prefer the use of low molecular weight heparin, although these pharmacological products do not have permission to market in this indication.
The therapeutic attitude to adopt towards the preventive treatment of venous thromboembolism in pregnant women with bleeding disorders, acquired or inherited, or a history of VTE, is not clear.
Further clinical studies are needed to validate the use of LMWH in this setting and specify what to do in certain therapeutic risk situations and during childbirth.
2- Introduction:
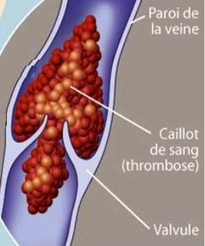
Pregnancy is a physiological state known as favoring the occurrence of venous thrombosis, due to many changes on the venous axis: decreased venous tone, slow flow, increased blood aggregability and compression of the inferior vena cava by the gravid uterus.
Aside from locoregional complications engaging only rarely life threatening, it is the migration of venous thrombus in the pulmonary artery territory that the gravity of this venous thromboembolic disease.
The existence of venous thrombosis in pregnancy poses a double challenge in the presence of the fetus: the diagnosis, due to the limitation of radiation irradiating additional examinations, and of the therapeutic to achieve because some anticoagulant treatment are Placental transfer.
These diagnostic and therapeutic difficulties are increased by the fact that there is no randomized prevention and treatment of venous thromboembolism in pregnant women.
While the number of postpartum venous thrombosis decreases because there is a better prevention, those of pre-partum varied little since firstly the clinical signs are nonspecific, common with those compatible with the pregnancy, and On the other hand it is difficult to track all women at risk.
Finally, one of which comes before pregnancy complicated venous thromboembolic disease imposes a thrombophilia research and prevention, poorly specified, the risk of recurrence.
3- Epidemiology:
The incidence of venous thromboembolic disease in pregnancy is variable according to the authors between 0.5 and 3%. This incidence is higher in patients with a history of thromboembolism, between 5 and 13% according Tengbom et al.
Venous thrombosis of the lower limbs occur preferentially on the left, in 77% of cases after James et al, with a predominance of superficial venous thrombosis compared to non-pregnant women.
The risk of venous thrombosis is uniformly distributed over the three trimesters and postpartum according to some authors, while James et al risk is higher in the third quarter. However, for Ginsberg et al Berggvist et al, it is higher in the second quarter.
However, the third quarter would theoretically be most at risk since firstly the compression of the inferior vena cava by the gravid uterus is maximum at this time and also the changes of hemostasis are more favorable to the occurrence of thrombosis during the first two quarters.
Pulmonary embolism is the second leading cause of maternal death after complications from abortions, its incidence being between 0.15 per thousand and 0.5 per thousand pregnancies.
The low incidence of venous thromboembolism during pregnancy is the cause of the inability to obtain samples of sufficient size for the studies randomized controlled effectiveness of treatment.
4- Pathophysiology:
Several factors contribute to the occurrence of venous thrombosis during pregnancy:
• The pregnancy itself induces a decrease in mobility and sometimes immobilization factor favoring already well known;
• Changes venous morphology, with increased diameter, decreased muscle tone, and compression of the inferior vena cava by the uterus;
• changes in hemostasis: increase of protein C and fibrinogen, decreased protein S and antithrombin III.
These physiological predisposing circumstances may reveal or exacerbate previously known thrombophilia or not:
• Acquired like the antiphospholipid syndrome secondary to lupus disease and other systemic diseases, malignancies or para-neoplastic syndromes, or primary responsible for 1/50 of venous thrombosis during pregnancy . The presence of anti-cardiolipin antibody induces a thrombogenic mechanism hypercoagulability and vascular endothelial injury;
• Constitutional known such deficiency physiological inhibitors of coagulation factors, protein C, S, anti-thrombin III deficiency and resistance to activated protein C.
According Mac Coll et al, the activated protein C resistance is involved in 8% of deep venous thrombosis, antithrombin III in 12% of cases (14% according to 17), the protein C deficiency in one % of cases (4% after 17) and protein S deficiency would be exceptional.
If resistance to activated protein C, 60% of DVT occur in the first trimester of pregnancy while others deficits would be more responsible for venous thrombosis after the postpartum Conard et al: 28% for antihrombine III, 18% for protein C and 17% protein S.
Furthermore, Kupferming et al have recently shown a high incidence of genetic thromboplhilie (protein C deficiency, S, antithrombin III, resistance to activated protein C) in women who experienced complications during pregnancy like pre eclampsia, fetal growth retardation, stillbirth or premature birth. These complications are most likely induced by the strong thrombogenic power related to these coagulation abnormalities.
Exceptionally, abnormalities of fibrinolysis are challenged:
ysfibrinogénémies qualitative and quantitative abnormalities of plasminogen.
5- Positive diagnosis of deep vein thrombosis:
1- The guidance: clinical suspicion:
• The clinic has no specificity compared to non-pregnant women, the diagnosis is suspected in the onset of swelling, pain and redness of the calf or thigh, unilateral distribution, sometimes in a context of low-grade fever.
In pregnant women, edema has little value as is often present in the physiological state. However, its asymmetry and associated hyperthermia should attract attention.
In case of superficial thrombosis, the diagnosis is strongly suspected by the presence of an inflammatory venous cord visible and palpable, usually on pre-existing varices.
• The measurement of D-dimer, the result quickly obtained by Elisa method, has no value in this context because its rate is gradually increased during pregnancy (value of 5288 ng / ml at the 40th week normal pregnancy).
2- diagnostic tests for confirmation of diagnosis:
These examinations pose the problem of fetal irradiation and therefore should be carefully selected according to the circumstances.
The Doppler ultrasound of the lower limbs is of great interest and not radiating to the fetus. Its sensitivity and specificity are greater than 95% if the examination is of good quality and qualified operator. However, the limit of this review lies in the exploration of the inferior vena cava and iliac veins, difficult if the examination is performed near term or in case of multiple pregnancy.
After a thorough clinical examination and completion of a Doppler ultrasound of the lower limbs, or the diagnosis is confirmed (most common), or it is highly suspected and it is then necessary to carry out further tests, or the diagnosis is ruled out with a probability.
The diagnosis is strongly suspected, and other tests will be needed to be able to tell, because the anticoagulant administration could have deleterious effects on the fetus and therefore should be administered in case of presence of thrombosis.
Venography in the water is then carried over (estimated fetal radiation <0.05 rads). If this is not enough venography (rare), a full venography is performed, however, more radiant (0.314 rads after). This dose is far from the teratogenic dose which is 50 000 Gy from Spritzer et al.
6- Diagnosis of pulmonary embolism:
1- The guidance:
a- The clinic:
As for venous thrombosis, it is no different in pregnant women but can be misleading because in this context dyspnea, sweating, malaise and chest pain are often reported in the state of pregnancy and therefore neglected.
The symptoms are usually present: dyspnea, tachypnea type, pleural pain, rather mid-thoracic kind, anxiety, cough and hemoptysis.
Pulmonary auscultation may reveal a decrease in respiratory amplitude reaches the side with evocative dullness pleural pleural effusion.
Sometimes the table can be immediately complicated by signs of acute pulmonary heart and right ventricular failure: jugular turgor, hepatomegaly with hepato-jugular reflux ……
b- The simple diagnostic tests:
The diagnostic value which is similar to that of non-pregnant women are often negative in particular in the first time of pulmonary embolism, and are instead mostly in their differential diagnosis:
The electrocardiogram is insensitive and shows in blockages greater than 40%, non-specific signs suggestive such as sinus tachycardia, an ultra right axis, a complete right bundle branch block, SI appearance QIII or more often as ischemia epicardial in leads V1 to V4.
Chest radiography often faulted, requires a local protection of the fetus by placing a lead apron and by reducing the irradiation zone to a minimum, although the amount of radiation is low, less than 0.001 rads by Ginsberg et al.
It will be possible to observe a basal opacity, pleural effusion of low abundance or elevation of the hemidiaphragm orienting the diagnosis. Chest radiography remains mostly useful for the differential diagnosis.
Arterial blood gases typically found hypoxemia associated with hypocapnia and respiratory alkalosis.
After clinical examination and simple paraclimiques these examinations, the diagnosis can be evoked by but be confirmed by imaging radiant unfortunately due to external radiation but also by the contrast medium injection.
2- Clinical situations:
Either the clinical picture is alarming, combining acute respiratory failure and right ventricular failure: it is therefore a massive pulmonary embolism.
The objective echocardiography dilated right cavities, the presence of a paradoxical septum and elevated systolic pulmonary arterial pressures.
The presence of a venous thrombus Doppler ultrasound of the lower limbs feasible to bed of the patient, will be an additional argument in favor of a pulmonary embolism.
The prognosis is engaged, anticoagulant therapy is administered rapidly even before the completion of any further consideration.
In the other case the prognosis is not quickly engaged and the suspected pulmonary embolism, the realization of a single infusion lung scan or ventilation-perfusion is required. This examination the advantage of being irradiated and not contain iodine injection but rather technicium whose half life is short (6 hours) and low trans-placental passage, thereby repeat the examination.
After completion of the scan, three situations:
Scintigraphy is normal and the diagnosis can be excluded;
Scintigraphy is high probability and finds a typical segmental perfusion defect with normal ventilation, suggestive of pulmonary embolism;
But many patients have an intermediate position and 21-40% of them have a pulmonary embolism. In this context, Doppler ultrasound of the lower limbs becomes important, since viewing a thrombus will be in favor of a pulmonary embolism. If this review did not find any thrombosis, pulmonary spiral CT seems to be justified, although more radiant than scintigraphy.
Pulmonary angiography performed in cases of discrepancy and doubt remains the gold standard. It will be performed if possible on a digital mode because this technique requires less product than simple clouding angiography. It will be limited to the suspect lung, and conducted by brachial route.
7- Treatment and care of venous thromboembolism during pregnancy:
1- Curative treatment of venous thromboembolic disease not involving the short-term prognosis:
a- Contention:
In the case of a deep or superficial vein thrombosis with or without pulmonary embolism not engaging the short-term prognosis, treatment consists in producing first a venous compression using low, with decubitus first time.
b- conventional treatments:
An unfractionated heparin therapy will be initiated by the intravenous route, heparin being recognized without deleterious effects to the fetus as it does not cross the placenta. Thus, it does not increase the rate of prematurity, spontaneous abortions, neonatal death, or birth defects.
Side effects of heparin, bleeding, thrombocytopenia and osteoporosis are not influenced by the state of pregnancy.
The initial dose of heparin is 5000 IU followed by a maintenance dose of 400 to 500 IU / kg / hour, to obtain an ATT between 1.5 and 2.5 times the control. The intravenous treatment will be maintained for 4-5 days.
Many studies have shown comparable efficacy of intravenous and subcutaneous heparin calcium and the relay can be taken quickly.
Low molecular weight heparins (LMWH) have also been used primarily in the preventive treatment of venous thromboembolic disease, but also in deep vein thrombosis and pulmonary embolism successfully, even on land at risk such that pulmonary embolism associated with placenta previa.
They have the interest to be able to deliver in one or two daily injections and requires less monitoring of effectiveness heparin calcium.

In addition, they show no trans-placental passage as evidenced by studies confirming the absence of serum heparin in the fetus.
However, they still do not have the Authorisation on the market for this indication.
The control will be done by the anti-Xa activity at the beginning of treatment and then monthly. Its effectiveness remains stable during pregnancy according to Nelson-Piercy et al, while others have suggested a decrease in the effectiveness imposing an increase in dose in the second half of pregnancy.
The vitamin K antagonists (VKA) are against-indicated during the first trimester of pregnancy, but may be indicated in the second or third trimester and in postpartum.
c- Thrombectomy:
Its main clinical indication is phlegmasia caerulea dolens this interesting technology appearing at the functional level in cases of thrombosis in iliofemoral territory. By cons, this treatment does no better than medical treatment for post-phlebitis sequelae.
d- Thrombolysis:
It has already been performed with success in situ catheter with rtPA, urokinase or streptokinase.
e- Indications for IVC interruption:
The accepted indications are: The recent deep vein thrombosis, with against-indication to anticoagulant treatment because in these patients the risk of pulmonary embolism is of the order of 50%, half of the recurrences being fatal, the occurrence of a pulmonary embolism anticoagulant and extension of thrombosis anticoagulant.
Most Discussed indications are: The very proximal thrombosis, iliac or cellar, the floating thrombosis, defined as a blood clot which most proximal 5 mm at least are free in the venous lumen, thus not adhering to the wall and thrombosis after embolectomy pulmonary surgery.
There is a situation of temporary interruption of the inferior vena cava cava filter, discussed and not related in the literature related to the particular situation of the pregnant woman, the recent diagnostic fee thrombus in the immediate vicinity of the term. Indeed, in this situation, the risk of thrombus migration is enhanced by the removal of the uterine obstacle on the inferior vena cava and the venous pressure in the blockpnée during labor.
This temporary interruption of the inferior vena cava is associated with anticoagulation with heparin (fractionated or not). The filter can be removed within one week after delivery.
Apart from this particular situation, the only indication to remember for filters is against cellar-indication to anticoagulant therapy and recurrence of pulmonary embolism in many led anticoagulation. The establishment of a caval filter appears sour is effective for the prevention of pulmonary embolism as evidenced by the experience of some authors.
2- Treatment of pulmonary embolism rapidly life-threatening:
The use of fibrinolytic therapy is then required, especially with APTN at doses of 100 mg in 3 hours to study Baudo et al, 43 mg and 5:30 for Flossdorf Coll or 60 mg for 8:20 Study Seifried et al. The infusion of rtPA was consistently associated with heparin injection by syringe pump.
Others have successfully used streptokinase. Only a small concentration of this product crosses the placenta (0.1 to 1% of the dose), which makes this product an excellent pharmacological treatment of severe pulmonary embolism in pregnant women.
However, streptokinase causes a release of fibrinogen degradation product having an inhibitory action on uterine contractility, a formidable if deliverance is near.
Surgical treatment is indicated in cases of cons-indications to fibrinolytic therapy and in case of massive pulmonary embolism, this surgery is burdened with significant fetal mortality. At the same time the operative embolectomy vena cava filter will be set up.
In the majority of cases of pulmonary embolism, the prognosis is not engaged in forward rate and the recommended treatment will be described previously started with the intravenous heparin and LMWH or VKA relay.
In front of venous thromboembolism in pregnant women, especially with an etiological research exploration of hemostasis (décit Protein C, S, antithrombin III and resistance to activated protein C) will be systematically performed.
3- Preventive treatment:
Venous compression methods, early mobilization and mobilization are recommended.
Low molecular weight heparins have good efficacy and good tolerance for preventive treatment: Enoxaparin, Tedelparine, dalteparin. The main side effects are bone demineralization (32% according to Nelson-Piercy et al), clinical expression in less than 3% of cases, and thrombocytopenia.
• For patients with a deficit known clotting factor (protein C, S, and antithrombin III), it is established that the risk for venous thrombosis is eight times greater compared to women without deficit .
In these patients, and those with an antiphospholipid syndrome or a history of venous thrombosis, heparin prophylaxis with low molecular weights could be made from the beginning of pregnancy until six weeks after birth, or even heparin syringe pump or by standard heparin because of an injection of 5000 IU every 12 hours during the first two quarters and then using heparin syringe pump adapted to TCA in the third quarter. Other authors propose prevention only in the third quarter and postpartum.
For resistance to activated protein C, the thrombogenic risk seems important during the first trimester of pregnancy, which theoretically would necessitate effective anticoagulation at this stage.
Studies are currently underway to establish a practical course of action in such situations at risk.
The therapeutic abstention is also possible provided to achieve regular monitoring by Doppler ultrasound of the lower limbs offered weekly by Demers et al.
8- Delivery and venous thromboembolic disease:
The low molecular weight heparin does not appear to increase the risk of bleeding during delivery vaginally or by caesarean section (for enoxaparin for the Dalteparin) and even that is no hemorrhagic complication post delivery.
Attitude is now to opt-in subcutaneous heparin 24 hours before the onset of labor. If a severe thrombotic risk of intravenous heparin is administered and stopped only 6 hours before delivery.
However, due to the residual effect of heparin, which can be effective until the 28th hour after administration, Ginsberg et al proposes a stop heparin syringe pump 24 hours before delivery, using protamine sulfate in case of hemorrhagic issue or epidural.
After delivery, heparin is reversed with vitamin K relay after 24 hours they are compatible with breastfeeding.
Low molecular weight heparins do not increase the risk of complications and local hematoma when performing epidural anesthetic referred, as evidenced by studies with Tedelparine and enoxaparin.
9- Conclusion:
Pregnancy is a predisposing factor for venous thromboembolism and can sometimes be indicative of a congenital abnormality of coagulation.
Diagnostic tests and therapeutic management of thrombosis are limited by the presence of the fetus, and only heparin therapy by syringe pump currently owns Authorisation on the market for this indication.
Other treatments have proven effective in particular the low molecular weight heparins whose simplicity and safety of use would make a treatment choice. It therefore seems appropriate to rapidly conduct clinical trials of these pharmacological agents to obtain marketing authorization in the indications for prophylaxis and treatment of venous thromboembolism during pregnancy, but also to establish their side effects when the issuance or epidural.
Further studies are also needed to determine how to proceed in the face of pregnant women at risk thrombogenic superimposed (vein thrombosis or bleeding disorder).


You must be logged in to post a comment.