Chronic bacterial infection endemic, human, Mycobacterium leprae. Very contagious, leprosy is spread by close, direct contact, especially at the family level. Children are particularly receptive.
Clinical signs:
Leprosy should be considered in any hypopigmented skin lesions or peripheral neuropathy. In case of suspicion, do a complete physical examination:
– Skin and mucous membranes (sick undressed)
– Neurological examination: tactile sensibilities, Algonkian (the picnic key test) and thermal (hot-cold test)
– Palpation of nerve pathways.
There are different clinical forms and different classifications of leprosy.
Classification of Ridley and Jopling has 5 forms determined by bacteriological index.
The simplified clinical classification of the WHO only 3 forms (see below).
Tuberculoid leprosy:
– Hypertrophic neuritis are prominent: pain, induration and increased volume of nerves; loss of thermal, then tactile and Algonkian. They are responsible for plantar ulcers and mutilations of the extremities.
– Lesions are single or few:
• plaque with a well-demarcated raised border and an atrophic hypopigmented center or
• erythematous macule on pale skin, hypopigmented on dark skin.
– Hypo or cutaneous anesthesia, no sweat and hair.
Lepromatous:
– Multiple mucocutaneous lesions are prominent:
• macules (léprides), papules or nodules infiltrated (lepromas) bilateral, symmetrical, pigmented, initially without loss of sensitivity, localized to the face, pinna, the upper and lower limbs;
• crusted rhinitis with bloody discharge;
• edema of the lower limbs.
– Neuritis late hypertrophic.
Borderline leprosy:
Intermediate forms between tuberculoid and lepromatous forms.
Indeterminate leprosy (form I)
Unclassified form in the Ridley-Jopling classification, frequent in children: single well-demarcated macule, hypopigmented on dark skin, slightly erythematous on pale skin. The absence of sweat and hair, and loss of sensation are inconstant.
It heals spontaneously or becomes determined leprosy: tuberculoid or lepromatous.
Lepra reactions:
– Reversal reactions: in a borderline patient under treatment, progression to tuberculoid. Changing Skin lesions become swollen and painful with a risk of necrosis and ulceration. Occurrence of acute painful neuritis (ulnar nerve) requires urgent treatment because risk of permanent sequelae.
– Degradation reactions: in an untreated borderline patient evolution towards lepromatous. They are difficult to distinguish from reversal reactions.
– Erythema nodosum: dermal-subcutaneous nodules, sensitive, rougeviolacés then yellowish, relapsing. See themselves exclusively in lepromatous leprosy during the first year of treatment.
To facilitate the diagnosis and to promote rapid initiation of treatment, WHO simplified clinical classification of leprosy and differentiates only 3 forms:
– Multibacillary leprosy = more than 5 skin lesions
– Paucibacillary = 2 to 5 skin lesions
– Paucibacillary single skin lesion
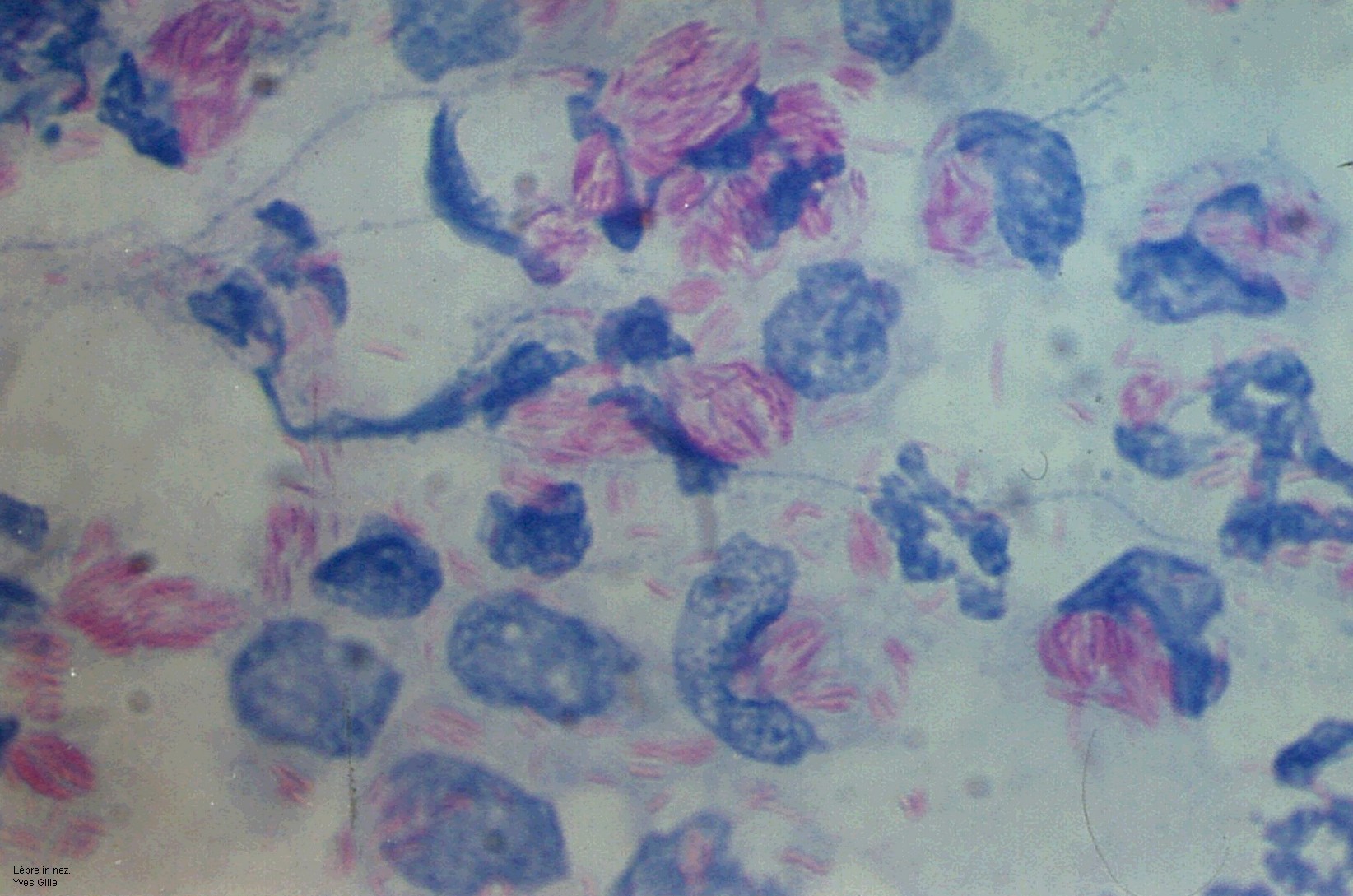
Laboratory:
Search acid-resistant bacilli by Ziehl-Neelsen:
– On nasal smear,
– Smear obtained by bloodless skin biopsy of the earlobe and injury.
In general, in tuberculoid bacilli are not found.
Treatment:
Treatment of leprosy:
– Leprosy is a curable disease. Early antibiotic treatment prevents functional sequelae and transmission of the disease.
– In endemic countries, there are national programs. Will know.
– High resistance and recurrence rates after monotherapy led to use effective and easy to administer combined treatments in the field for which no resistance has been reported.
– Teach the patient to recognize and quickly report a lepra reaction or relapse in order to modify or restart treatment.
Treatment of leprosy reactions:
– Reaction reversion or degradation: prednisolone (or prednisone) PO: 1 mg / kg / day for 3-5 days and then continue decreasing the dose gradually (reducing every week the 10% dose).
– Erythema nodosum leper clofazimine PO 100 to 300 mg / day associated with NSAIDs. (Do not administer doses ≥ 300 mg for more than 3 months).


You must be logged in to post a comment.