Introduction :
Introduction :
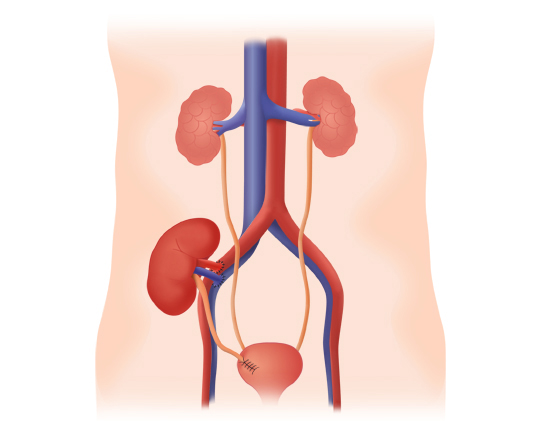
Acute renal failure (ARI) in the renal transplant patient is an acute decrease in glomerular filtration rate (GFR). The IRA in the transplant recipient may be identical in its causes to that of the clean kidneys in a non transplanted subject, with in addition to specific causes related to the dysfunctional kidney transplant state. These specific causes concern ischemia / reperfusion, rejection, vascular and urinary anastomoses, the toxicity of immunosuppressive molecules, the complications of immunosuppression.The future of the graft is related to the early diagnosis and the effectiveness of the therapy.
Definitions:
Acute renal failure:
ARI is defined as a rapid deterioration (hours, days or weeks) of GFR associated with accumulation of nitrogenous wastes. The collapse of urinary flow is a very specific criterion of ARI. However, urinary flow is not impaired in about 50% of ARI cases and therefore oliguria and anuria symptoms do not have good sensitivity.
In the renal transplant patient there are two situations: either the IRA occurs while the GFR has normally increased after the transplant, or there is an initial non-recovery of a GFR in the usual time after the transplant called delayed recovery of the GFR. function (RRF). RRF is a special IRA because it is most often due to tissue damage acquired in the donor or during the period of preservation and declamping (ischemia / reperfusion); the other causes of RRF are not necessarily related to ischemia / reperfusion, but occur early in the first hours of transplantation (vascular surgical complications, ureteral, treatment toxicity, later humoral and cellular rejection). These other causes of RRF are considered with all causes of ARI since they are not related to ischemia / reperfusion. Coexistence is possible between these two types of phenomena, for example that of ischemia / reperfusion phenomena and tubular toxicity of anticalcineurins.
The definitions of ARI are multiple; there is no definition recognized and used by the entire nephrological community.
Kellum identifies 30 definitions of the IRA. Ricci, in a survey of 560 centers, lists 199 definitions.
No standardization exists on serum creatinine level, urine output. The percentage increase in serum creatinine or decrease in GFR in a given time appears to be an acceptable criterion, but the notion of time scale (hours, days, weeks) must be specified.
It should also be borne in mind, when interpreting creatinine variations, that the plasma creatinine concentration depends not only on changes in renal clearance of creatinine (filtration plus secretion), but also in those of production (muscle mass) and volume of distribution.
The International Acute Dialysis Quality Initiative has proposed a classification of the IRA called RIFLE: risk injury failure loss end stage. The five categories are defined according to changes in serum creatinine, urinary flow, and dialysis time since the acute event. The group “failure” is the one with the worst prognostic factors and the worst kidney survival. This classification is not very adapted to the daily management of renal transplant patients, except those requiring resuscitation.
Mehta proposes a four-stage ARI classification based on susceptibility (previous GFR, risk factors: diabetes with microalbuminuria, dehydration, myeloma, congestive heart failure, decompensated cirrhosis), nature and date of kidney aggression. , variations in GFR (according to RIFLE) and urinary flow. The definition of ARI must be adapted to the population studied. Mehta retains 16 different definitions and insists on choosing a definition based on an objective: the IRA defined as the need for dialysis has nothing to do with the definition of ARI of the transplanted subject who must be very sensitive in order to detect dysfunction as soon as possible. The monitoring of the renal function of the transplant patient is indeed intended to give the alert from the first functional impact of a rejection or other complication.
Delayed recovery of the function:
The variable delay of resuming function after the ischemia / reperfusion period requires to define from which values there is a RRF. The graft function definitions used in the Cochrane Collaboration on the value of calcium channel antagonists during harvesting and transplantation. Daly recalls various definitions used in the literature to characterize RRF. These definitions correspond to a delayed recovery or a slow resumption of function. All variants exist between the absence of function (sometimes accompanied by anuria) and the rapid recovery of glomerular filtration with normal glomerular filtration on the fourth day, as is usual with living donors:
• the number of days to obtain a creatinine clearance greater than 10 ml / min (Cockcroft);
• serum creatinine greater than 265 μmol / l (3 mg / dl) on the fifth day after surgery;
• the need for dialysis within 72 hours after transplantation;
• creatinine up, stable or decreasing by less than 10% per day for 3 consecutive days in the first week;
• serum creatinine greater than the figure obtained prior to surgery or urinary flow of less than 300 ml within 6 hours after transplantation with correct blood volume and diuretics;
• less than 30% reduction in serum creatinine or less than 1 liter of urine in the first 24 hours;
• A serum creatinine reduction ratio at d 2 <30%.
Other definitions are encountered. The reported incidence of RRF in kidney transplantation varies according to the sensitivity of the definition. A percentage of 20 to 40% for transplants with RRF is reported in most published studies.Perico reports 4-10% RRF for living donors and 2-50% for cadaveric donors.
Diagnosis of acute renal failure in transplant patients:
Function measurement:
The goal is early, sensitive screening to quickly diagnose graft dysfunction for immediate administration of appropriate therapy. Methods of measuring DFG using external markers (inulin, 51 Cr-EDTA, 99m Tc-DTPA, 125 I-iothalamate, iohexol) give values close to physiological values. These are specialized tests used quite extensively in clinical research but not in the daily clinic because of their complexity and cost, especially during the acute period after transplantation.
The evaluation of GFR by measuring serum creatinine is simple, imprecise, but of great clinical utility.
Gaspari et al. analyzed in the kidney transplant patient the performance of 12 predictive equations of GFR taking the iohexol clearance as a reference; they do not recommend these estimates for clinical trials with an overestimation of GFR (from 3.43 to 30.19%) and an overestimate of the decline in GFR over the 15 months following the transplant.Walser’s and MDRD’s (abbreviated modification of diet in renal disease) formulas are the best in the GFR estimate (Cockcroft and Gault’s is seventh out of 12), and the Walser, and Cockcroft and Gault formulas are the closer to the reference method in assessing the decrease in GFR in the 15 months following the transplant. Their data thus indicate a possible use of the formulas of Walser, abbreviated MDRD and Cockcroft and Gault in daily clinic, knowing that only the formula of Cockcroft and Gault is easily calculable. The simplified MDRD formula is more successful in older subjects than Cockcroft and Gault. This formula is more and more used.
Another Poggio study in kidney transplants specifies the best performing approach of DFG. Measurement of serum creatinine with FGD estimation by calculation therefore remains the most practical means, the most used by general practitioners and nephrologists to diagnose the IRA graft, and to assess its evolution and the functional sequelae. The situation is often that of an ARI on a background of chronic renal failure. Another marker, cystatin C, is currently evaluated as an indicator of GFR; Herget-Rosenthal et al. demonstrated that the diagnosis of ARI could be earlier with cystatin C, with anticipation being 1 to 2 days. This dosage is not yet widespread.
During the follow-up of a transplanted patient, the variation of the function is more important to consider than the absolute value of the GFR, and a simple and even discreet elevation of the serum creatinine is a sensitive and specific sign. Changes in serum creatinine not related to changes in GFR are due to changes in extracellular volume, which in the immediate post-transplant period are not negligible and may account for small fluctuations in serum creatinine.
The daily weight curve should be available when interpreting serum creatinine immediately.
Acute or organic acute renal insufficiency?
An IRA is, in the subject grafted as in other situations, organic or functional. The distinction is made based on the presence of clinical elements predisposing to functional renal failure (dehydration), the use of drugs that can modify GFR (angiotensin converting enzyme inhibitors, AT1 receptor antagonists II, nonsteroidal anti-inflammatory drugs).The classical biological criteria, not always present, which plead for a functional renal insufficiency (low urinary sodium, inverted sodium / potassium ratio, low excreted fraction of sodium and urea, ratio of the urinary concentration to the high creatinine plasma concentration) have sometimes also a diagnostic interest.
Acute renal failure in renal transplant patients Acute renal failure of ischemia / reperfusion:
This term covers a set of biological reactions that take place during the preservation of the kidney after its removal (cold ischemia during transport and warm ischemia essentially at the time of transplantation) and at the time of revascularization which occurs at the unclamping of the anastomosing vessels. Ischemia / reperfusion is responsible for a delayed recovery of function or a definitive primary non-function. Dahmane et al. found 7.7% non-functioning in a group of at-risk donors (kidneys transplanted between 1992 and 1998 after being rejected by two teams) and 1.8% in a control group. Ischemia / reperfusion increases the probability of acute rejection. It is also associated with chronic rejection and long-term loss of renal function.
Clinically, ARI secondary to ischemia / reperfusion results in non-function and anuria as soon as surgery is performed;however, anuria can occur after 24 hours of diuresis and sometimes it is a non-function preserved diuresis.
Pathophysiology:
Ischemia results in decreased oxidative metabolism, adenosine triphosphate (ATP) depletion, sodium / potassium / ATPase pump inhibition, and anaerobic glycolysis.
The accumulation of lactic acid lowers the intracellular pH and weakens the lysosomes with proteolytic activity.
Some intracellular metals are in free form and this generates oxygen radicals. There is also a probable deleterious role of nitric oxide with a production of peroxynitrite which alters the proteins. The cytoprotective mechanisms involved during ischemia would be less active when it comes to kidneys taken from brain-dead patients. Depletion of ATP results in necrosis or apoptosis of tubular epithelial cells. The altered cell release products such as the high mobility protein group 1 (HMG-1) result in tumor necrosis factor (TNF) alpha production and leukocyte infiltration. Inflammatory cells can synthesize interleukin (IL) 1 which causes synthesis of TNF and IL6 by tubular cells. The toll-like receptors are activated by molecules derived from tubular epithelial cells and cause the synthesis of inflammatory cytokines via NF-kappa B.
Reperfusion results in warming and reoxygenation, return to aerobic metabolism and ATP production. This is also accompanied by a major synthesis of superoxide anions, hydrogen peroxide, resulting in the peroxidation of lipid membranes. The antioxidant mechanisms are outdated and there is cell death by apoptosis.
These phenomena are responsible for the release of pro-inflammatory cytokines and chemokines. IL8 and the C5a fragment, for example, are responsible for the attraction of polymorphonuclear cells. Expression of the IL8 gene (neutrophil and macrophage chemotaxis) increased by 50% at the time of reperfusion in a living donor and increased 13-fold at the time of reperfusion of cadaveric donor kidney. This demonstrates the link between the importance of ischemia and inflammation. The adhesion molecule intercellular adhesion molecule (ICAM) 1 and vascular cell adhesion molecule (VCAM) 1 (and their ligands, leukocyte integrins) play a role in the experimental lesions of ischemia / reperfusion. Endothelin is responsible for vasoconstriction after ischemia / reperfusion. The immunogenicity of the allograft is increased by ischemia: in the postischemic period, there is an increase in the expression of major histocompatibility complexes in the tubulointerstitial situation. Interferon gamma, IL10, transforming growth factor beta, granulocyte-macrophage colony stimulating factor are mediators of this action. The proteins modified by ischemia can become antigenic.
The complement system is activated after ischemia / reperfusion by the alternative way. In the clinic, acute rejections are more common in RRF cases in a large number of studies.
Immunosuppressive agents given experimentally before autologous transplant ischemia / reperfusion reduce the intensity of the lesions. Inactivation of the C3 and caspase 3 gene prevents experimental ischemia / reperfusion injury in mice.
Histopathology:
In the absence of other phenomena, the histological lesion induced by ischemia-reperfusion is that of a tubular necrosis with dilation of the tubes, loss of the brush border, necrosis or apoptosis of the epithelial cells and cylinders.Tubulo-interstitial cell infiltration is possible.
Risk factors:
Published risk factors for RRF were analyzed by Perico et al. At the time of sampling, it concerns the sampling with stopped heart, the administration to the donor of molecules with inotropic effect, cold ischemia time. In the donor, it is the age above 55 years, high blood pressure, diabetes. In the recipient, the risk factors are hemodynamic components (hypovolemia, hemodialysis with ultrafiltration within 24 hours before transplantation), the weight of the recipient and the number of prior transplants. The difficulty of the surgery can indeed lead to deleterious hot ischemia times for the graft.
Treatment:
The prevention of ischemia / reperfusion injury and RRF is a major goal in renal transplantation, with RRF a poor long-term predictor. The use of second generation infusion solutions (University of Wisconsin solution, Celsior ® …), volume expansion of the recipient, use of diuretics (mannitol and furosemide) are common. Continuous infusion of the kidneys is still little used in France. The use of calcium channel blockers in the donor and recipient was evaluated by a meta-analysis; the favorable effect exists but is not major. Other substances have been proposed for experimentation such as prostacyclin, natriuretic peptide, selective and non-selective endothelin receptor antagonists, antioxidants (N-acetyl-cysteine, nitric oxide synthase inhibitors) and factors modulating inflammatory phenomena. These include, for example, platelet activating factor receptor (PAF) antagonists, anti-TNF alpha antagonists, IL1, IL10, IL13 cytokine inhibitors or antagonists, membrane cofactor protein (MCP) 1, anti-ICAM1, anti-factor B monoclonal antibody, complement inhibitors, statins, CTLA4 immunoglobulin immunoglobulins (Ig), mycophenolate mofetil (MMF), soluble ligand of P selectin glycoprotein.
It can also be growth factors such as insulin-like growth factor. It has been shown experimentally in pigs that immunosuppression with MMF and tacrolimus decreases production after transplantation of free radicals and pro-inflammatory cytokines (TNFα, IL6 and IL8) and increases the protective effect of ischemia training. At present, few specific treatments for ischemia / reperfusion injury are used in the human clinic.
In the case of RRF, the patient should be treated symptomatically and graft biopsies performed at regular intervals to diagnose a possible rejection that can not be demonstrated by studying the evolution of serum creatinine. Vigilance is all the more necessary as there are risk factors for rejection (prior immunization, loss of a first graft rejection …) and there are few risk factors for tubular necrosis (shock in the donor, long ischemia time). The biopsy is performed both in the case of primary nonfunction and in case of breakage of the curve of favorable evolution of serum creatinine. An extemporaneous examination allows a rapid diagnosis of rejection within one hour after the biopsy.
Acute renal insufficiency, other than those related to ischemia / reperfusion:
All causes of ARI on clean kidneys can have the same effects on a transplanted kidney. There are also specific transplantation-related causes, whether related to transplant surgery, allogeneic transplantation, immunosuppressive drugs, immunocompromised status, or the treatment of infectious complications specific to transplantation.
ARI in transplant patients can be classified according to the time of onset or according to the mode of toxicity and altered renal structure. They are described according to the point of impact of the responsible phenomenon.
Tubular and interstitial lesions:
Acute cellular and humoral rejections:
They are less frequent with intensification of immunosuppression. Mostly encountered during the first year of transplantation (from 10 to 20% of transplants depending on the series), they are of cellular or humoral type. Acute cellular rejection is the most common. It is expressed by an interstitial lymphocytic infiltrate and the penetration into the tubular epithelium of the lymphocytes of the recipient, realizing an appearance of tubulitis. The intensity of the phenomena is measured according to the Banff classification.
Borderline discharges and rejections of grade IA are the most commonly encountered. The treatment is essentially steroid-based. These rejections can occur throughout the life of the graft. Late after 1 year, they suggest an interruption of immunosuppressive therapy. Cell rejections can also be glomerular and / or vascular. Humoral rejections generated by antibodies are rarer; they are vascular, often seen in patients immunized in the human leukocyte antigen (HLA) system before transplantation. The presence of the complement C4d fraction in the peritubular capillaries on the biopsy is one of the signatures of the vascular humoral discharges. Hyperaussive rejections occurring with preformed specific antibodies to the circulating graft before transplantation are very rare due to the detection of this specific immunization by cross match techniques.
Anatomically, there are intrarenal thrombotic lesions.
Pyelonephritis:
Most often, the donor ureter is implanted in the bladder of the recipient with reconstitution of a submucosal antireflux pathway. However, there is vesicoureteral reflux in some patients; it is a risk factor for pyelonephritis. Pyelonephritis of the graft has the same characteristics as that of clean kidneys. Renal function deteriorates during the infectious episode. It is necessary to make sure of the freedom of the excretory way. Ultrasound and if necessary CT scan can eliminate an obstacle and highlight parenchymal inflammatory areas. The treatment meets the same requirements for initial dual antibiotic therapy and duration (3 weeks). The recurrence of pyelonephritis leads to search for reflux by cystography. In a series of 1,022 transplants, Kamath et al. observe 16.5% of patients with pyelonephritis. In this study, ureteral stent placement, urological malformation of the native kidneys, cytomegalovirus infections, mycophenolate treatment and acute rejection are risk factors for pyelonephritis. Giral et al, in a single-center series of 1,387 patients, report 180 cases of acute graft pyelonephritis. Fifty-seven patients had more than one episode of pyelonephritis. The episode of pyelonephritis does not appear on a global analysis as an independent factor influencing graft survival. The episode of acute pyelonephritis occurring in the first 3 months of the transplant is a very significant independent risk factor for graft loss (relative risk = 3.6, p <0.007). In this series, graft pyelonephritis is more common in women, cytomegalovirus infection is an independent risk factor for graft pyelonephritis and the presence of Escherichia coli during the first episode is the only risk factor for relapse. identified.
Polyomaviridae infections:
For the past ten years, kidney infection with BK virus has been a concern for transplant practitioners. BK and JC viruses are viruses of the polyomaviridae family. BK against which 80% of the population has antibodies is a virus capable of destroying the renal parenchyma of immunocompromised patients. The diagnosis is based on the presence in the urine of tubular cells with a cytopathogenic effect, the decoy cells. Their absence has an excellent negative predictive power. Other diagnostic tools are the cytopathic effect seen on the graft biopsy, a positive immunofluorescence of the renal biopsy with SV40 antibodies, the positivity of in situ hybridization and the positivity of the polymerase chain reaction on the blood and urine. Some patients are treated, due to interstitial infiltrate, for rejection before the diagnosis is made. Treatment is primarily a decrease in immunosuppression, an antiviral agent can be used, cidofovir or leflunomide.
Lymphoproliferative syndromes:
Lymphoproliferative syndromes after renal transplantation are sometimes localized in the renal parenchyma; they are then responsible for an IRA with increased volume graft.
These are B proliferations (CD20 positive) most often induced by an Epstein-Barr virus (EBV) infection. The appearance of a monoclonal immunoglobulin is often associated.
The diagnosis is pathological with markers of lymphocytes and EBV. The treatment begins with a decrease in immunosuppression and then the use of a monoclonal anti-CD20 antibody; CHOP chemotherapy is used in the third line.
Interstitial nephritis immunoallergic:
Interstitial immunostatic nephritis with the presence of eosinophilic cells within the interstitial tissue may occur, for example, after the administration of antibiotics or during a viral infection with viruses other than the BK virus, for example an adenovirus .
Toxic tubulopathy:
Toxic tubulopathy is most often related to the use of anticalcineurin. Pharmacological monitoring (punctual dosing or calculation of the area under the curve with a variable number of points) is an indispensable tool to avoid an inappropriate dosage of ciclosporin or tacrolimus.
Overdose exposes to nephrotoxicity, inadequate dosage to rejection. The introduction or interruption of immunosuppressive molecules (mycophenolate) or not (macrolides, dihydropyridines, anticonvulsants …) must be accompanied by a question about the possible interaction of these treatments with the metabolism of ciclosporin. The toxicity of ciclosporin has vascular tropism (protein deposits) in the arteriolar wall) and tubular (isometric vacuoles).The use of sirolimus is difficult in the immediate post-transplant period because of its responsibility in the delay of function. This effect has been attributed to its antiproliferative action. Cases of ARI associated with myoglobinuria have been described with sirolimus. Pelletier et al. found tubular necrosis lesions in 10.5% of all patients transplanted between 2002 and 2004, and in a quarter of these cases myoglobin cylinders that are only found in patients taking sirolimus. Stopping sirolimus restored anterior renal function in these patients.
Aminoglycosides should be prescribed with caution taking into account the estimated GFR. Reinjections are made according to the serum level. The first injection is done at normal dosage regardless of the level of renal function.Intravenous Ig are administered with immunological or anti-infectious objectives (parvovirus B19). Renal failure is due to osmotic nephrosis. The toxicity is greater with immunoglobulin preparations containing sucrose. The nephrotoxicity of iodinated contrast products is of course related to the renal graft (CT angiography, arteriography). If administration is necessary, the usual precautions should be taken: correction of any dehydration of the patient; stopping diuretics;alkalinization; administration of N-acetyl-cysteine (no very strong argument); use of products best tolerated by the kidney.
Tubular obstruction:
The use of sirolimus may be associated with episodes of ARI. Smith et al. reported in 2003 cylindrical tubulopathy in patients treated with sirolimus by day 0 and tacrolimus, the cylinders disappeared after stopping sirolimus.
The accumulation of light chains and the formation of tubular cylinders can lead to ARI in case of monoclonal dysglobulinemia. These light chain deposits in the glomeruli and tubular basal membranes (kappa more often than lambda) can cause deterioration of graft DFG. This disease of the deposition of light chains can appear de novo or pre-exist in the patient before his transplantation. In 50 to 60% of patients, there is a proliferative disease (myeloma most often), in others the monoclonal globulin is of undetermined significance. The syndrome of lysis in the case of treatment of a highly tumoral lymphoma in a transplanted can be at the origin of an IRA.
Glomerular lesions:
Glomerular rejection is reflected more in a chronic fashion with allograft glomerulopathy characterized by double contour images. The recurrence of the initial glomerular disease (nephrotic syndrome, focal and segmental glomerulosclerosis) is evoked by a sometimes massive and early proteinuria; renal function may degrade.
Vascular lesions excluding thrombotic microangiopathies:
Big trunks:
Arterial thrombosis, which is infrequent since it is evaluated at 1% or less of grafts, is a complication that usually signifies graft loss. The diagnosis is that of a postoperative anuria to be feared especially if there is no RRF factor. A special situation is compression of the artery by hilar lymphoma, a compression that can progress to thrombosis and secondary anuria. Diagnosis is based on arterial Doppler examination, CT angiography or magnetic resonance angiography (MRI). Venous thrombosis, the frequency of which is estimated at around 4 to 6% of transplants, may be favored by thrombophilia in the recipient or the positioning of the kidney in the iliac fossa.
This complication is of very poor prognosis, surgery is rarely followed by effect. The exploration is done by doppler, angio-MRI, angioscanner or invasive angiography. Thrombophilia must be sought: protein deficiency S or C, mutations of the clotting factor gene (factor V Leiden, prothrombin G20210A …), antiphospholipid antibodies, lupus disease, preformed anti-HLA antibodies are risk factors for thrombosis. Cortical necrosis of the graft has been described in a patient with a G20210A prothrombin gene mutation. Thrombophilia states must be detected in families at risk in order to have a preventive action. The thrombotic manifestations must be prevented postoperatively (heparin then aspirin, or heparin then antivitamines K).
Anastomotic or juxta-anastomotic stenosis may be the cause of graft dysfunction, the prescription of drugs blocking the renin-angiotensinealdosterone system is likely in such a case to cause an IRA: Doppler ultrasound is the examination of choice, but MRI angiography is sometimes useful. Angiography is only performed with the ulterior motive of angioplasty. The iliac artery above the anastomosis with the graft artery may be the site of progressive atheromatous lesions with graft ischemia downstream.
The subcapsular hematoma after graft biopsy can be accompanied by an IRA for a few days without ultrasound or densitometric images evoking an obstacle on the excretory tract. The mechanism invoked is that of an increase in graft pressure (page kidney).
Microvascularization:
Hyperacute rejection by preformed antibodies occurs early (day to day), with biopsy of infarcted areas with polymorphonuclear cells. Cellular vascular rejection is negative C4d with involvement of vessel endothelium, without necrosis of the entire wall. The antibody-dependent (humoral) vascular rejection has C4d deposits in immunofluorescence.
There is necrotizing arteritis, fibrinoid necrosis of the arteriolar wall, neutrophil infiltrate; IgG and C3 are present in the wall of the arteries. Non-vascular humoral rejection is associated with the presence of C4d in the peritubular capillaries. Humoral vascular rejection (induced by antibodies) is treated with intravenous Ig, plasma exchange and antiCD20 antibodies.
Atheroma is common in patients with renal failure and endovascular maneuvers, and anticoagulants are risk factors for embolization of the graft by cholesterol crystals.
The diagnosis is clinical if another localization is visible as livedo, blue toes or punctiform necrosis. Biology shows eosinophilia. The biopsy shows the ghosts of the crystals in the vessels of the grafted kidney.
Thrombotic Microangiopathies (MAT):
IRA is accompanied by hemolysis with haptoglobin loss, increased anemia, increased lactate dehydrogenases, and thrombocytopenia. The different types of MAT can be found in kidney transplantation. They may be secondary to a recurrence of the initial disease or a deleterious effect of certain immunosuppressors with de novo microangiopathy.Hemolytic and uremic syndromes (HUS) are either due to verotoxigenic bacterial toxins (SHU + diarrhea) or secondary to congenital deficiency in complement system factors (H, I and MCP factors) or secondary to drug prescriptions (contraceptives, mitomycin C, ticlopidine …). HUS diarrhea – without congenital deficiency in complement factors may be associated with still uncharacterized deficits. Thrombotic thrombocytopenic purpura (TTP) may be due to a congenital deficiency of von Willebrand factor-mediated metalloprotease (ADAMTS13), or secondary to anti-ADAMTS13 immunization with decreased cleavage activity. In the first case with congenital deficit, the clinical picture is similar to congenital HUS. After transplantation, there are de novo HUS triggered by immunosuppression (5 to 15% of patients on ciclosporin and 1% of patients on tacrolimus, cases have been reported with mammalian inhibitors target of rapamycin [mTOR]). . Cyclosporine could trigger an immune response against ADAMTS13 protein and thus inactivate cleavage of von Willebrand factor. Vascular rejection is also associated with anti-ADAMTS13 immunization.Familial HUS associated with mutations in the H and I genes of the complement system recur on the graft in at least 50% of cases, on average 30 days after transplantation. The risk of graft loss is important. This should make it very cautious for a living donor and encourage the etiological investigation to be carried out as far as possible (see the website of the European Society of Pediatric Nephrology, http://espn.cardiff.ac. uk /).
If the mutation concerns the MCP protein, there is no recurrence because the non-circulating, transmembrane protein is highly expressed in the transplanted kidney. The risk of relapse is 33 to 56% in patients with idiopathic MAT. The risk of recurrence on the graft is negligible in case of HUS associated with diarrhea, calculated at 0.8% in children. It is also weak in the case of toxic MAT. If you have a history of MAT, you should avoid using drugs that induce MAT.
Protocols with anti-CD25 monoclonal antibody, mycophenolic acid and corticosteroids may be provided. Congenital ADAMSTS 13 deficiency is associated with thrombotic thrombocytopenic purpura relapses post-transplantation with probably a favoring factor such as calcineurin inhibitors, mTOR, acute rejection, viral infection. The treatment comes down to regular infusion of fresh frozen plasma. Treatment is difficult in relapses of HUS with mutation of H and I factors; Plasmatherapy is recommended, liver transplantation, theoretically curative deficit, has not yet given good results confirmed. Rituximab could be proposed in the form of ADAMTS13 deficiency with antibodies given its action in nontransplanted subjects.
De novo MAT associated with the prescription of a calcineurin inhibitor has a better prognosis than relapses; the treatment involves stopping the calcineurin inhibitors; the use of tacrolimus instead of ciclosporin could be proposed, as well as a supply of fresh plasma (plasma exchange), possibly intravenous Ig.
Excretory way:
Urinary fistula (about 3%):
Urine leakage occurs in the distal region of the ureter at the level of bladder reimplantation in case of ureterovesical anastomosis, which is very much the case. It is either an ischemic ureteric necrosis, or leakage of the surgical anastomosis. The ultrasound shows the urinoma, a computed tomography scan can locate the leak. The drain, if it is still in place, allows the analysis of the drained liquid, which suddenly becomes more abundant. The concentration of creatinine in this liquid, close to that measured in the urine, makes it possible to make the diagnosis of urinary fistula.The treatment is surgical.
The donor ureter is either reimplanted into the bladder or anastomosed with the recipient’s own ureter. A ureteral wound may occur longer after transplantation during endovascular urological procedures.
Ureteral stenosis of ischemic origin:
The ureter of the transplanted graft has a terminal vascularization by branches of the renal hilar arteries. During collection, some of these ureteral arterial branches may be damaged and the distal portion of the ureter reimplanted into the bladder of the recipient will be ischemic.
This results in stenosis occurring in the weeks following the transplant. Clinically, it is an ARI with pyelic and ureteral dilatation. The treatment is either endoscopic by endoprosthesis, or surgical with the same solutions as those used for urinary leakage.
Extrinsic stenosis by compression by a lymphocele:
The lymphocele, which can complicate the dissection of the iliac fossa, in some cases compresses the excretory tract with dilatation upstream and IRA. The diagnosis is ultrasound by showing the reports of the ureter and the lymphatic collection.
An uroscanner is sometimes useful for confirming the cause-and-effect relationship. The treatment of the lymphocele is most often surgical (peritoneal drainage); an evacuating puncture may be previously attempted in order to confirm the responsibility of the compression on the function of the graft.
Other causes of ureteral stenosis or obstruction:
Other causes of ureteral problems are dysfunction of the suture, torsion of the ureter (kinking), edema of the ureterovesical anastomosis, compression by hematoma, calculus, periuretal fibrosis, abnormality of the junction in the donor, a clot after biopsy of the graft.
The ureter may be clogged by clot following a graft biopsy. Ureteral obstruction may be secondary to precipitates: Guitard et al. published a case of juxtavésicale ureteral lithiasis of N-acetyl-sulfadiazine in a patient treated for toxoplasmosis. Ureteral obstruction may be secondary to the migration of a transplanted calculus with the kidney. The unprepared image of the area, the ultrasound and sometimes the uroscanner participate in the diagnosis.
Renal transplantation alone in case of oxalosis is not recommended because of the rapid recurrence of lithiasis manifestations in the graft; a liver-kidney transplant must be proposed. Extrinsic stenosis by lymphomatous mass is possible. The treatment is urological to ensure urinary drainage, at first a probe rise can be attempted but the ureteral orifice is sometimes difficult to catheterize because of its position in the bladder in the transplanted subject. Treatment of the lymphoproliferative syndrome may allow the passage of urine; Interventional urological or radiological drainage solutions must be found in the meantime.
Prostatic obstacle:
Upon removal of the bladder catheter in the graft suites, bladder retention may occur. Men on dialysis and anuric at the time of registration on a transplant list are not very good candidates for resection of prostatic adenoma or bladder neck because of the absence of urinary flow. It is at the time of removal of the bladder catheter after transplantation that the rate of urination, the existence of a residual postmixture, must be monitored and, if necessary, resection of the cervix and / or adenoma. An ARI can be established if the free flow of urine is not assured.
Cystitis:
Adenoviruses can be responsible for hemorrhagic cystitis, fever, graft dysfunction and emotional pain. Diagnosis is made with urine culture and biopsies for virus, serology and in situ hybridization. Thirty-six out of 37 reported cases occurred in the first year of transplant and all patients spontaneously recovered.
Functional renal insufficiency:
Many subjects will have, because of arterial hypertension, diabetic disease, proteinuria, treatment with ACE inhibitors or angiotensin II receptor antagonists. It can even be the two associated molecules. The vascularization of the graft may be compromised due to nephroangiosclerosis of the arterioles or because of atheromatous stenosis of the artery;in these cases, the GFR may decrease after prescription of these molecules. Coprescription of diuretics may increase this effect of the blocking agents of the renineangiotensin-aldosterone system. It is accepted that a 20 to 25% increase in serum creatinine is acceptable if it is the price to pay for good blood pressure control and a reduction in proteinuria.ACE inhibitors or angiotensin-2 receptor antagonists are well tolerated in the post-transplant period (first 3 months) when serum creatinine is less than 265 μmol / L.
Practical driving:
Renal transplant patients should be monitored according to specific procedures mentioning the frequency of visits and the nature of the biological and morphological assessments performed.
These are variable according to the teams. The frequency of serum creatinine measurements can be, for example, twice a week for the first 3 months, then weekly until the sixth month and biweekly until the first birthday of the transplant. The subsequent frequency of the evaluations depends on the clinical situation of the recipient. Each biological evaluation is followed by a medical consultation which is carried out according to the habits of the center with a doctor of the transplant center and / or the treating nephrologist and / or the general practitioner (voluntary and informed) who all consult a file common (paper file circulating with the patient or computerized record remotely accessible). Any deterioration of function must after confirmation lead to the achievement of an adapted report after a careful clinical examination. Examination of the progression of creatinine in the medium term is rich in teaching, a spontaneous improvement after deterioration should not necessarily lead to inaction because the function can thus deteriorate gradually.
A minimal evaluation to be made to a degradation of the function of the graft involves the taking into account of the old and recent history of the graft, the clinical examination, a blood count, an echography of the graft, an assay of the anticalcineurine if the patient receives it (ciclosporin, Neoral ® or tacrolimus, Prograff ® ). First, the questioning is about possible new drugs that can interfere with the metabolism of anticalcineurins and increase the serum level (macrolides for example). It is also necessary to check the absence of prescription of nephrotoxic drugs the previous days, in particular the administration of iodinated contrast media. The molecules blocking the renin-angiotensin system are susceptible, in case of introduction or increase of dosage, in particular in the dehydrated patient, to cause a degradation of function; this occurs when the graft has impaired vascularity. In the absence of a rapidly obtained explanation, a biopsy of the graft after checking the haemostasis should be performed in search of a parenchymal cause (rejection, toxic tubulopathy …).
Treatment of severe acute post-transplant renal failure:
If, because of the severity of the renal insufficiency, an extra-renal treatment is necessary in the continuation of a graft, a daily frequency is advised by analogy with the IRA in general. Schiffl et al. have shown that daily hemodialysis reduces mortality without increasing the morbidity due to hemodynamics. For patients on peritoneal dialysis, manual or automatic exchanges must be resumed; special attention should be paid to patients whose peritoneal cavity was opened during the transplant, a consultation with the surgeon is necessary before starting the peritoneal dialysis.Extrarenal treatment conditions for ARI are also available in transplant patients. Nutrition during this period is an important part of the prognosis.
The monitoring of the rejection is made difficult by the non-function of the graft and it is important to perform biopsies of the graft to ensure the absence of inflammatory immunological reaction. Systematic bacteriological monitoring of the urine, if any, of the possible drainage fluids (drain), peritoneal dialysis fluid, natural orifices, is useful to detect as early as possible a portage, an infection and to envisage the treatment.
Preventive treatment:
There are many preventive measures, both at the time of collection and transplantation, and afterwards. The reduction of cold and hot ischemic time is a major objective to take into account in all organizational changes.
Measures to prevent the nephrotoxicity of drugs and diagnostics must be systematic; serum levels of nephrotoxic drugs should be ascertained and nephrotoxicity of contrast agents should be maintained (correction of dehydration, discontinuation of diuretics prior to examination, nature and volume of iodinated contrast medium best suited, possible use of N acetyl-cysteine). In case of RRF, discontinuation or dose reduction of nephrotoxic immunosuppressants should be discussed depending on the patient’s immune profile.
Conclusion:
The glomerular filtration rate at 1 year is an excellent prognostic marker of graft function in the longer term, for example 5 years. It is important to follow patients very closely in the first year in order to treat episodes of ARI as quickly as possible, whatever the cause, in order to have the least possible sequelae. Due to the ARI etiologies specific to the transplantation situation, there is a need for close collaboration between the attending physician, the treating nephrologist, the transplant center practitioners, and the pathologist for patient follow-up. The next years will be those of early diagnosis of rejection and monitoring of therapeutic efficacy by urinary proteomics and transcriptome analysis.