Introduction:
Introduction:
The kidney and upper excretory pathway (ESV) are paired and bilateral anatomical entities, which constitute the upper urinary tract. The functions of the upper urinary tract are the secretion of urine by the kidneys and then its excretion by the VES. The VES is divided into intrarenal VES, calyx and renal pelvis, and extrarenal VES, the ureter. The latter opens into the bladder, which forms, with the urethra, the lower urinary tract, an anatomical, odd and median entity.The entire urinary tract is outside the peritoneal cavity and the upper urinary tract is retroperitoneal.
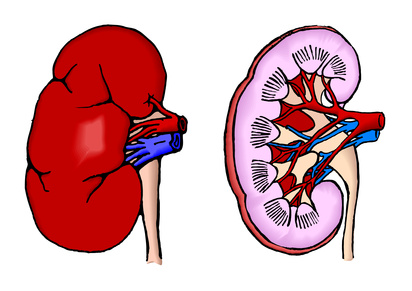
Anatomy of the Kidneys:
The kidneys are solid organs, secreting the urine. They are located on either side of the spine, in the lumbar region, against the posterior wall of the abdomen.
External morphology:
Each kidney has the shape of a flattened ovoid, consisting of:
• two faces, anterior (or ventral) and posterior (or dorsal);
• two edges, external (or lateral) and internal (or medial);
• two extremities or poles, upper (or cranial) and lower (or caudal).
The lateral edge, regular and convex, is called the convexity of the kidney. The medial border, indented, is hollowed out of a cavity at its middle part: the renal sinus. The opening of the renal sinus is called the renal hilum. The renal hilum contains the elements of the renal pedicle and delineates the intrarenal and extrarenal SVs,
also known as intrasinusal and extrasinusal VES. The two edges of the renal hilum are called the anterior (or ventral) and posterior (or dorsal) lips.
The surface of the kidneys is smooth in adults and polylobulated in children. Their color is dark red, their consistency firm.
In the young adult, their average dimensions are: 12 cm in height, 6 cm in width and 3 cm in thickness. The height of the kidneys is proportional to the size of the individual. The renal hilum has a height of 3 cm and a thickness of 1.5 cm.
Each weighs about 140 grams in man and 125 grams in women. The left kidney is slightly larger than the right.
Internal morphology:
The kidneys consist of a parenchyma that surrounds the renal sinus. The renal parenchyma is covered with a fibrous capsule, solid, not very extensible, which adheres weakly to it. The capsule covers the walls of the renal sinus and extends with the vascular adventitia of the pedicle elements and the adventitia of the VES.
The renal parenchyma consists of a central renal medulla and a peripheral renal cortex.
Renal Medulla:
The renal medulla consists of triangular areas called renal pyramids (or Malpighi pyramids). The renal pyramids contain right renal tubules and collecting tubules. They are dark red in color and striated parallel to the major axis of the triangle. They number eight to ten per kidney. Their apex protrudes into the renal sinus and forms the renal papillae.
Renal Cortex:
The renal cortex is the glomerular filtration area. It is reddish in color and of friable consistency. It is 1 cm thick between the base of the renal pyramids and the capsule. It penetrates between the pyramids, and each segment of the interpyramidal renal cortex is called the renal column (or Bertin column). The renal cortex consists of a contoured portion and a radiated portion. The contoured portion constitutes the superficial cortex, in contact with the capsule. It contains the renal corpuscles (or corpuscles of Malpighi). The radiated portion is located in contact with the base of the renal pyramids.
It is made up of numerous striated beams: the cortical pyramids (or Ferrein pyramids), which are extensions of the streaks of the renal medulla corresponding to a condensation of the right renal tubules and their vascularization.
Each renal pyramid, with the area of the renal cortex which surrounds it and extends it to the capsule of the kidney, forms a renal lobule; which is why there is a lobulation of the kidneys in children, which disappears in adults.
Renal Sinus:
The renal sinus is a cavity that contains the ramifications of the renal pedicle and the intrarenal or intrasinusal SEV.
Its walls are made up of renal parenchyma. They are irregular and made of conical projections, the renal papillae.
Between the papillae, the parenchyma forms beads called renal columns covered by the capsule. There are regular conical papillae, simple papillae, and others resulting from the union of several simple papillae (from two to four): the compound papillae. In each sinus, the number of papillae varies from 4 to 20 and there are on average 8 to 10 (as many as pyramids). The tip of the papillae is punctured with small holes forming the screened area of the renal papilla, through which the secreted urine is discharged into the VES.
Microanatomy:
The medulla and the cortex are made up of about 1 million nephrons, which are the microscopic functional units of the kidneys. Each nephron comprises two parts: the renal corpuscle and the renal tubule.
The renal corpuscle is also composed of two parts: the glomerular capsule (or capsule of Bowman) and the glomerulus.
The renal tubule consists of three segments: a proximal proximal contoured tubule, in contact with the renal corpuscle, and then the right ascending and ascending renal tubules which constitute the loop of the nephron (or loop of Henlé), and finally a distal circumvented tubule in a collecting tubule.
The collecting tubules are connected to several nephrons and give the pyramids their striated appearance. They end up in the squint area of the papillae.
Vascularization:
Renal vascularization is assured by the elements of the renal pedicle, which is composed in 75% of an artery and a vein. The vascularization of the kidney is of the terminal type. Within the pedicle, the renal artery is the most posterior element and the renal vein is anterior. The ramifications of the renal pedicle are very variable and the most common mode of division of the renal vessels is described.
Arterial vascularization:
Origin, route, termination of renal arteries:
The two renal arteries originate from the lateral surfaces of the abdominal aorta. They are born at the same level, at the lower third of L1, about 2 cm below the origin of the superior mesenteric artery. They are carried transversely, obliquely downwards and backwards, towards each renal hilum. Their diameter is 6 to 8 mm and their length is 3 to 4 cm to the left and 5 to 6 cm to the right. Physiologically, their flow rate is 1.2 l / min, which corresponds to about 20% of cardiac output.
Each artery rests on a pillar of the diaphragm, then on the large psoas muscle, and constitutes the most posterior element of the renal pedicle. To the right, the renal artery passes behind the inferior vena cava and then behind the right renal vein. Each renal artery divides into the hilum into two main terminal branches which run on either side of the VES: an anterior branch known as pre-pyleal and a posterior branch called retropyleal. Each branch then divides into intrarenal branches called upper and lower segmentals.
The caliber of the anterior arterial branches is greater than that of the posterior ramifications.
Microvascularization:
Segmental intrarenal arteries branch into interlobular arteries that cross the walls of the renal sinus around each papilla and travel to the surface of the pyramids to their base. The ramifications of the renal artery are therefore interpapillary then interpyramidal. At the base of the renal pyramids, they give arched arteries, which run between the cortex and the medulla. The arched arteries divide to give the interlobular arteries that run in the radiated portion of the renal cortex. The interlobular arteries are directed towards the capsule of the kidney by capillarizing into afferent glomerular arteries, which vascularize the nephrons. Each nephron thus receives an afferent arteriole, which forms a network of capillaries organized into a pelota called a renal glomerulus (or Malpighi glomerulus), a vascular element of the renal corpuscle.
The glomerular capillaries then meet to form the efferent glomerular artery. The diameter of the efferent arteriole is smaller than that of the afferent arteriole, resulting in high arterial pressure in the renal glomerulus.
Around each nephron, efferent arteriole gives rise to a cortical capillary plexus. The juxtamedullary efferent arterioles and the interlobular arteries also give right arterioles, the vasa recta, which form a medullary capillary plexus traversing the renal pyramids from the base to the top. All these branches are terminal and do not anastomose with each other.
Arterial territories:
The great variability of the ramifications of the renal artery made it impossible to describe a systematic segmentation.
In the case of a division of the renal artery into a pre- and retropyelic branch, the territory of the anterior branch is the most extensive. The ramifications of the anterior branch irrigate the ventral half of the kidneys and an adjacent portion of the dorsal half. There is thus an avascular plane on the posterior part of the renal convexity.
Changes in renal arteries:
In 75% of cases, there is a single renal artery originating from the abdominal aorta and joining the renal hilum. There are variations in the number of arteries, in their level of origin on the abdominal aorta, in their mode of division and in their course. When an artery directly reaches one of the poles without traveling through the hilum, it is called the polar artery (upper or lower). When it is unique, the renal artery can also divide early, before the renal hilum.
Collateral branches of the renal arteries:
Each renal artery gives several collateral branches:
• a lower adrenal artery for the adrenal gland;
• a ureteral branch for the lumbar ureter;
• nodal branches for lymph nodes;
• capsuloadipous branches for perirenal fat.
There exists around the convexity of the kidneys an exorenal arterial circle which is a set of anastomotic branches.From this circle, a few branches can pass through the capsule, but this network is insufficient to ensure renal vascularization in case of obstruction of the renal artery.
In addition to the renal artery, these branches may have as their origin the inferior adrenal artery, the ureteral branch, the gonadal artery, a superior colonic artery, lumbar arteries, or even the abdominal aorta.
Venous vascularization:
Origin, pathway, termination of renal veins:
Each renal vein originates from the union of intrarenal veins within the renal sinus. The so-called segmental intrarenal veins are arranged in a perical and then peripyleal network. In the renal hilum, the peripyelic network is resolved into two or three anterior venous trunks, at the origin of the renal vein.
The diameter of the renal veins is 10 mm and their length is 2-3 cm on the right and 7-8 cm on the left. Physiologically, the flow of the two renal veins represents one third of the inferior vena cava flow, on which two thirds of the total venous return to the right atrium depends.
Each vein has a transverse path, oblique upwards and inwards, and constitutes the most anterior element of the renal pedicle. The renal veins terminate perpendicularly on the lateral surfaces of the inferior vena cava, at the level of the disc L1-L2. Their ostium cellar is avalvulated.
On the right, the renal vein flows directly into the inferior vena cava.
To the left, the longer vein crosses perpendicularly the ventral surface of the abdominal aorta, passing behind the superior mesenteric artery, in the aortomesic forceps.
Microvascularization:
The capillaries of the cortical plexus join to form the star-shaped veinlets which join the satellite interlobular veins of the arteries in the radiated portion of the renal cortex. The blood then passes into the arched and then interlobar veins, which also receive straight venules from the medullary capillary plexus. The interlobar veins, satellites of the arteries, are then at the origin of the intrarenal veins, then of the renal vein. Unlike the arteries, the renal veins are largely anastomosed.
Changes in renal veins:
The renal vein is unique in 90% of cases. In other cases, it can be double, even triple, and accompany a possible polar artery.
Collateral branches of renal veins:
Each renal vein receives a lower adrenal vein of the adrenal gland, an ureteral branch of the lumbar ureter, and capsuloadipous branches of the perirenal fat. Like the arterial network, the adipose capsule of the kidney contains a venous network, the exorenal circle, which pours into the neighboring veins: suprarenal, colic, ureteral. This small collateral network can be hypertrophied in the case of tumor pathology, especially when there is a renal vein thrombus.
The left renal vein receives a greater number of collateral, of larger size:
• the left superior adrenal vein on the upper margin;
• the left gonadal vein on its lower border;
• often the anastomosis of the ascending lumbar vein: reno-azygo-lumbar arch, on its posterior surface.
Lymphatic vascularization:
Renal lymphatic vascularization is rich and the flow of renal lymphatics is equivalent to diuresis. The initial network of intrarenal lymphatics consists of a subcapsular cortical network and a deep network draining along the interlobular vessels in the radiated portion of the cortex and along the right vessels of the medulla. The whole drains then along the arched and then interlobar vessels, up to the renal sinus. The various collectors then emerge from the renal hilum around the renal artery or the point of penetration of a polar vessel. Their number is variable (from five to seven), their caliber is fine (from 1 to 2 mm). The lymphonodes to which the collectors go are different on the right and on the left.
To the right, the pre-arterial collectors follow the renal artery by forming a retrocave network, then inter-aortico-cave, leading to a lymph node located at the lower edge of the origin of the right renal artery. Below it, they will have a descending orientation to end in the precave lymphonodes at the height of the aortic bifurcation and at the origin of the inferior vena cava. The retroarterial collectors are placed against the right pillar of the diaphragm and join the thoracic duct, directly or indirectly via pedicular renal lymph nodes.
On the left, pre-arterial collectors are located at the upper edge of the renal vein and drain into the pedicular renal lymph nodes located above the origin of the left renal artery and then terminate in the lateroaortic lymph nodes, origin of the renal artery up to the origin of the inferior mesenteric artery. Some join the inter-aortico-cellar, celiac or even iliac lymph nodes. The retroarterial collectors terminate in the thoracic duct.
Innervation:
Renal innervation depends on the autonomic nervous system and the renal plexus. The sympathetic afferences of the renal plexus originate from the sympathetic trunk ganglia of T10 to L1 via the small splanchnic nerve, the splanchnic imus nerve, the first lumbar splanchnic nerve and the celiac plexus. The parasympathetic afferents originate from the vagus nerves.
All these nerves form a periarterial renal plexus which may have small renal ganglia, one of them being nearly constant, the aorticorenal ganglion.
The autonomic nerve network enters the renal parenchyma along the vascular axes and the VES, and is also distributed in the renal capsule. In the parenchyma, it is essentially perivascular, and forms rich plexuses around the interlobular artery and afferent arteries, of which it will control the vasoconstriction.
Reports:
The kidneys are located in the lumbar region, which is a retroperitoneal, even and symmetrical region. Inside each lumbar region, the kidneys are not perfectly symmetrical, since the right kidney is located lower than the left kidney.The relationships of the kidneys are described within this region, then with the other retroperitoneal organs and finally with the intraperitoneal organs.
Reports in the lumbar region:
Kidney Orientation:
Knowledge of renal orientation is necessary to understand the relationship of the kidneys. In the frontal plane, the major axis of each kidney is oblique downwards and outwards, according to the orientation of the large psoas muscles on which the dorsal aspect of the kidneys rests. The major axes of the two kidneys meet in front of the body of the thoracic vertebra T10.
In the horizontal plane, the renal hiles are oriented towards the abdominal aorta and the inferior vena cava, which ensure their vascularization. The axes intersect in front forming an angle of 90 ° open to the rear due to the strong convexity of the lumbar spine. The two faces of each kidney are therefore dorsomedial and ventrolateral. Finally, in the sagittal plane, the kidneys follow the lumbar curvature by inclining 25 ° downwards and forwards.
Means of fixity, renal fascia and adipose capsule:
The means of fixity of the kidneys are the renal pedicle and the renal fascia. The transverse orientation of the renal pedicles, which opposes the force of gravity, shows that the kidneys are also maintained by a solid fibrous envelope, the renal fascia. The kidneys thus appear suspended and mobile, since they follow the respiratory movements.
Renal fascia is a condensation of the retroperitoneal connective tissue delimiting the renal chamber. This contains the kidney, its pedicle, the adrenal gland and the adipose capsule of the kidney. The renal fascia consists of two layers, prerenal and retrooral, which are in continuity and surround the kidney and its adipose capsule. The prerenal leaf (or fascia of Gerota) is fine and adheres to the posterior parietal peritoneum through the mesocolons, ascending to the right and descending to the left. The retorenal (or Zuckerkandl) fascia is denser and more resistant. It is separated from the posterior abdominal wall by fat, except medially where it merges with the iliac fascia of the large psoas muscle. The renal chamber is thus fixed to the posterior abdominal wall and the adipose capsule of the kidney is in contact with the large psoas muscle.
The two leaflets meet at the upper pole and include the adrenal gland, which is separated from the rest of the kidney by a thin intersurrenalorenal wall. Laterally, the two layers merge behind the convexity of the kidney. They extend caudally without being united and form a fatty prolongation of the adipose capsule of the kidney. On the median line, the anterior leaflet adheres to the vascular pedicle so that the right and left kidneys do not communicate.
The adipose capsule of the kidney or perirenal fat is a pale yellow, almost fluid fat, unlike the more compact pararenal fat located outside the kidney box.
It infiltrates the elements of the renal pedicle, in the renal sinus and around the VES. It is vascularized by the perirenal vascular circle and allows the kidney to be mobile inside its box.
Relationship with posterior abdominal wall:
Pararenal fat is the fat in the lumbar region that separates the kidney box from the posterior abdominal wall and the diaphragm. It is mostly abundant in the back of the kidney lodge.
The large muscle psoas, lumbar portion of the iliopsoas muscle, is the most important muscle ratio. On the one hand, the renal chamber is fixed to its iliac fascia by the retro- nal sheet.
On the other hand, the posterior aspect of the adipose capsule and the pedicle elements, in particular the posterior renal artery, rest on its fleshy body. On the surgical plane, the large psoas muscle is therefore an anatomical landmark very useful for the dissection of the renal pedicle. It is a very thick fusiform muscle, which is inserted by fibrous arches of the lateral surface of the vertebral bodies from T12 to L5 and on the corresponding intervertebral discs. The fleshy body thus descends along the lumbar spine, passing behind the diaphragm and then increasing in width from top to bottom. Its oblique lateral edge gives its orientation to the kidney, which is immediately outside. It flanks the convexity of the vertebral bodies and covers the medial half of the square muscle of the loins.
The diaphragm, in its lumbar portion, is inserted on the pillars of the diaphragm and the medial arched ligament. The right pillar descends on the anterior surface of the lumbar spine from L1 to L4, and the left pillar from L1 to L3. The medial, fibrous arched ligament connects the lateral side of L2 with the transverse process of L1.
The pillars of the diaphragm are two muscular bundles which are inserted by two vertical fibrous blades joined on the median line to form the median arcuate ligament. The diaphragm is covered on both sides by a thin aponeurosis.
The kidneys lie behind the last two ribs. The twelfth rib is retrooral and constitutes the lower limit of the pleural cavity.The posterior aspect of the renal chamber is thus related to the pleural cosmetic recess.
The twelfth vasculocervical pedicle travels under the twelfth rib, in front of the square muscle of the lumbos, and then passes through the fascia of the transverse muscle. The iliohypogastric and ilio-inguinal nerves also run in front of the square muscle of the loins, in the pararenal fat, and penetrate the transverse muscle laterally.
Relationship with other retroperitoneal organs:
To the right, the adrenal gland covers the superior pole and medial suprahilar margin of the kidney. It slides back from the inferior vena cava. The upper pole of the kidney responds to the lateral border of the inferior vena cava, when the latter slopes to the right to pass behind the liver. The descending part of the duodenum (or second duodenum) covers the anterior surface of the renal pedicle and the inferior vena cava via the duodenopancreatic fascia (or Treitz fascia).
On the left, the adrenal gland covers the medial suprahilar border of the kidney and rests on the renal pedicle. It is interposed between the abdominal aorta and the upper pole of the kidney, which is thus more distant from the lateral edge of the abdominal aorta. The duodenojéjunal angle covers the medial sub-hilar border via the fascia of Treitz.
Relationship with intraperitoneal organs:
To the right, the angle of the colon covers more or less the anterior surface of the kidney. At this point, the colic wall is separated from the renal fascia by a welding fascia resulting from the weld between the parietal peritoneum in front of the renal chamber and the colonic visceral peritoneum. The liver also responds to the anterior surface of the renal chamber, which is not covered by the colon or duodenum. Between the liver and the upper half of the renal chamber is inserted a peritoneal cul-de-sac, the hepatorenal recess.
On the left, the upper portion of the renal chamber is related to the spleen. The splenic vessels and component parts of the trunk carry forward of the hilum and anterior surface of the left kidney. The tail of the pancreas, covered by the two leaflets of the pancreaticosplenic ligament, is connected with the superior pole and the hilum of the kidney. It is at the middle part of the anterior aspect of the kidney that the posterior peritoneal leaf of the pancreatic tail is reflected on the parietal peritoneum covering the renal chamber.
The left angle, attached to the pancreas and to the diaphragm by the mesocolon and the phrenocolic ligament, passes forward of the left kidney, and continues under the spleen by the descending colon. The renal chamber corresponds to the descending mesocolon, joined by the left retrocolic fascia, and to its vessels, in particular to the left superior colic vessels. The crossing of the left colonic artery and the inferior mesenteric vein, which constitutes the vascular arch of Treitz, is generally situated within the lower pole of the kidney.
Anatomy of the upper excretory pathway:
On each side, the VES consists of the intrarenal or intrasinusal VES, the calyx, the renal pelvis (or pyelon), and the subsequent extrarenal VES, the ureter.
Upper intrarenal excretory pathway: calyx and renal pelvis
The calyxes are divided into minor and major calyxes. Minor calyxes are the initial part of the intrarenal SEV and collect urine excreted by the renal papillae. The major chalices follow them and collect the urine secreted by the minor calyxes. They throw themselves into the kidney pelvis, the central excretory cavity of the sinus.
External morphology:
Minor calyxes are ducts molded on the renal papillae. They thus form convex cavities towards the exterior, the number of which is equal to that of the renal papillae (from eight to ten). From a length of 1 to 2 cm, they are inserted on the periphery of the areas screened by a circular fibrous ring called fornix.
They thus delimit a peripapillary groove around the papillary cones. Fornix, an element of continuity between the renal sinus capsule and the VES adventitia, is fragile and ruptures in the event of a sudden increase in urine pressure within the VES. Minor calyxes are multidirectional and, like the papillae, there are simple and compound minor calyxes. A compound minor chalice is wider and corresponds to the union of several simple calyxes around a compound papilla.
The major calyces are formed by the confluence of two to four minor calyxes. From a number varying from two to five, the major calyces are arranged in the frontal plane of the kidney. In 65% of the cases, there are two major calyces, superior and inferior, and in 32% of the cases, three are superior, middle and lower. The length and breadth of the major calyces is variable, but they all converge towards the renal pelvis. The upper major chalice is long and narrow, rising towards the upper pole, in the continuity of the ureteral axis. The lower major chalice is shorter and wider, slightly descending towards the lower pole, making an angle of 60 ° with the ureteral axis. It receives the average minor calyxes except when there is a medium major chalice which then drains into the renal pelvis with an angle of 90 ° with respect to the vertical axis of the ureter.
The renal pelvis has a triangular shape. It is flattened from front to back and has:
• two faces, anterior and posterior;
• an almost vertical medial edge;
• a horizontal, concave lower edge;
• a lower vertex, which responds to the ureter abutment to form the pyelo-ureteral junction;
• a base, which receives the major calyces in the renal sinus.
Its morphology is variable and depends on the number of calyces it receives. In the most frequent case, where it receives two major chalices, one speaks of bifid renal pelvis. If it receives three major chalices, it is called pyelic.Rarely, it can receive minor calyxes directly and take a globular form (3%).
In total, the capacity of the intrarenal SEV is low, less than 3 ml. Its excretory function is permanent by collecting the urine secreted by the kidneys, but it does not constitute a reservoir of urine. The reservoir function is entirely provided by the bladder.
Internal morphology:
The wall of the intrarenal VES consists of three tunnels: a mucous membrane, a muscular and an adventitia.
The mucosa is globally identical and has a pseudostratified epithelium (polymorphic or transitional) based on a chorion.
The epithelium is a urothelium, which constitutes a barrier to the reabsorption of urine.
The muscularis is formed by bundles of smooth muscle cells separated by conjunctive spans and has two layers, internal longitudinal and external circular.
The weed is a connective tissue containing vessels, nerves and adipose tissue in contact with the adipose capsule of the kidney.
Vascularization and innervation:
The intrarenal VES receives its vascularization directly from the branches of the renal pedicle.
Its innervation is assured by the efferences of the periarterial renal plexus. There is an autonomous contraction that begins in the calyces and spreads in the renal pelvis to the pyelo-ureteral junction.
Reports:
The intrarenal SV is at the center of the renal sinus and the renal hilum. Minor calyxes are multidirectional and located in the axis of the renal pyramids and their papillae. The major chalices and the renal pelvis are then in the same frontal plane which, due to the obliquity of the kidney, is about 45 ° behind the coronal plane.
The renal pelvis sinks fairly little into the renal sinus: the intrasinusal segment does not exceed half a centimeter. Only the globular kidney pelvis sink deeper into the renal sinus due to the absence of major calyces. The pyelo-ureteral junction is thus extrasinusal. The renal pelvis occupies three quarters or the lower half of the renal hilum.
The intrarenal ESV is separated from the kidney pedicle by the peripheral fat of the adipose capsule. The pericual vascularization is the richest in contact with the walls of the renal sinus. At this point, venous anastomoses are numerous.
At the renal hilum, the two faces of the renal pelvis respond to the pre- and retropyelic vascular ramifications. In its extrasinusal portion, the renal pelvis is located behind the renal pedicle. On its anterior surface, the arterial branches of the prepapiae are horizontal, and the intrarenal veins join to form the renal vein. On its posterior surface, the retropyelic arterial branch, vertical, follows the posterior lip of the renal hilum, thus leaving uncovered the extrasinusal portion of the renal pelvis. The surgical approach of the renal pelvis is therefore indicated on its posterior face.
Through the renal lodge, the extrasinusal renal pelvis rests on the large psoas muscle. On the right, it is covered by the second duodenum and to the left by the tail of the pancreas.
Extrarenal upper excretory pathway: ureters
The ureters, right and left, are the urinary ducts that connect the renal pelvis to the bladder.
External morphology:
The ureters extend from the pyelo-ureteral junction to the ureteral meatus in the bladder. In adults, they are 25 to 30 cm long. They are divided into four segments: lumbar (10 to 12 cm), iliac (3 to 4 cm), pelvic (10 to 12 cm) and intravesical or intramural (2 cm). They terminate in the bladder by a submucosal oblique path and participate in the constitution of the bladder trine.
The course of the ureters is sinuous, and their lower pelvic curve is the most pronounced. Applied on the posterior abdominal wall, they descend almost vertically to the upper strait. At this point, they describe a curve with an anterior convexity, which follows that of the iliac vessels. Then they follow the pelvic wall and the sacral concavity by describing a curve with antero-internal concavity which leads them to the bladder.
Along their path, the diameter varies from 3 to 6 mm, and presents three constrictions:
• at its origin, at the pyelo-ureteral junction;
• in the iliac region, with respect to the intersection with the iliac vessels;
• in its intramural portion.
Throughout their journey, they are animated by a peristalsis which allows the urine to progress towards the bladder.
Internal morphology:
The ureters are cylindrical muscular ducts, made up of three tunics:
• a mucosa, the urothelium, which is in continuity with that of the renal pelvis and the bladder;
• a muscularis, the composition of which is identical to that of the renal pelvis in the upper two-thirds of the ureter, and which in its lower third consists of three layers, longitudinal internal and external, and medium circular;
• an adventitious, periureteral fascia, containing vessels, nerves and adipose tissue on its dorsal surface, thus constituting a narrow vessel-carrying plate. The ventral surface of this fascia is attached to the posterior parietal peritoneum.
Reports:
The ratios of the ureters differ according to their segment: lumbar, iliac, pelvic or intravesical.
Uretera lumbar:
Through the pararenal fat of the lumbar region, they rest on the iliac fascia which covers the large psoas muscle. The pyelo-ureteral junction is usually projected in relation to the costiform process of the second lumbar vertebra. The lumbar ureters then project on the tip of the costiform processes of the lumbar vertebrae L3, L4 and L5, from which they are separated by the large psoas muscles. They cross the anterior surface of the genitofemoral nerves.
Their previous relations are different on the right and on the left.
The right ureter is separated from the second duodenum and genius inferius by the fascia of Treitz. Lower, it is covered by the ascending mesocolon. The left ureter is covered over its entire extent by the descending mesocolon.On each side, they cross the gonadic vessels to place themselves within these vessels below the crossing. Laterally, they are related to the lower pole of the kidneys, and then with the large psoas muscles. Medially, the right ureter is 2 cm from the inferior vena cava. On the left, it borders at a distance the angle of the duodenojejunal, the abdominal aorta, the left colonic artery and the inferior mesenteric artery.
Ureteric iliacs:
Upon entering the upper strait, the ureters pass forward of the iliac vessels. In general, the right ureter passes forward of the external iliac artery, and the left ureter crosses the primitive iliac.
Outside, they respond to the medial margin of the large psoas muscles and the genital vessels that remain parallel to them.
In front, the right ureter is crossed by the lower extremity of the mesentery and by the termination of the ileocolic artery. On the left side, it is covered by the secondary root of the mesosigmoid, and then by the pelvic parietal peritoneum.
Pelvic Uretera:
Upon entering the small pelvis, the ureters describe a concave curve forward and inward. They present a parietal portion, then visceral. Their relationships differ according to sex.
In women. In their parietal segment, the ureters descend below the pelvic parietal peritoneum, along the internal iliac artery. In most cases, the right ureter is in front, and the left within the artery. They correspond to the origin of the branches of the anterior trunk of the internal iliac arteries: umbilical artery, obturator artery, uterine artery, lower vesical artery, vaginal artery, middle rectal artery. Through the parietal peritoneum, the anterior relations of the ureters are: the ovaries, the ampullary pavilions and a possible pelvic vermicular appendix on the right side.
Their parietal segment ends in the base of the broad ligaments.
In their visceral segment, the ureters engage forward and inward in the parameter. At about 2 cm outside the uterine cervix, the uterine arteries which were behind and outside the ureters make a crook, intersect their ventral surface to move inwards. At the same level, the vaginal arteries accompanied by uterine and vaginal veins run along the posteromedial margin of the ureters and cross their dorsal surfaces. The ureters are then accompanied by anterior branches of the lower hypogastric plexus, and by arterial and vesicovaginal venous branches. They then pass out of the anterior vaginal cul-de-sac and penetrate into the posterior bladder wall.
In the man. In their parietal segment, the ureters also descend under the pelvic parietal peritoneum, along the internal iliac arteries. The branches of the anterior trunk of the internal iliac arteries are different: umbilical artery, obturator artery, lower vesical artery, middle rectal artery. On the inside, the ureters are in relation with the lateral faces of the rectum from which they are separated by the lower hypogastric plexus.
In their visceral segment, the ureters also engage inward and inward, behind the umbilical arteries. They pass in front of the rectum, cross the posterior surface of the vas deferens, the vesiculodeferential artery and engage in the bladder wall. In the back, they are separated from the seminal vesicles by the anterior plate of the rectoprostatic fascia (Denonvilliers fascia).
Intravesical Uretera:
The ureters traverse the bladder obliquely downwards and inwards. Their path is about 2 cm long: 1 cm through the muscularis and 1 cm under the mucosa. The ureteral meatus is located at the lateral extremities of the bladder trigone and is connected by an inter-lateral muscle bar. In their muscular traverse, the fibers of the ureteral muscularis combine with those of the detrusor. The outer longitudinal muscular layer is individualized to form a sliding zone with the rest of the ureteral wall. The inner longitudinal muscular layer flourishes in the trigone and the inter-lateral bar.Their submucosal path is dilated. Above this dilatation, the wall of the ureter is constituted by a hemicircular mucous fold.
The intramural and submucosal path forms an antireflux system.
Vascularization and innervation:
The arterial vascularization of the ureters is segmental. It is rich for the iliac and pelvic segments, and poorer for the lumbar segment. Their initial lumbar portion receives the ureteral branch of the renal artery, anastomosed to the arterial circle of the kidney. The second important branch comes from the internal iliac artery. The rest of the arterial supply is made by branches coming from the numerous arteries crossed on their way. The lumbar ureters thus have a more precarious vascularization since they receive essentially branches from the gonadal arteries. Their pelvic segment receives numerous small twigs from the visceral branches of the internal iliac arteries.
The arterial branches are anastomosed by a network of periureteral collaterals, especially rich against the posterior wall of the ureter, and intraparietal collateral.
The venous vascularization is satellite of the arterial vascularization. The ureteral veins flow mainly into the renal, gonadal, internal iliac and lower vesical veins.
The lymphatic vascularization consists of a submucosal and intramuscular network. The lymphatic collectors of the ureters run into the adventitia and then drain into neighboring lymph nodes following the arterial vascular axes. The lymphatic collectors of the right ureter drain into the latero-cava and interaorticocaval lymphomas.
The lymph collectors of the left ureter drain into the lateroaortic lymph nodes on the left from the origin of the renal artery to the bifurcation. The collectors of the iliac ureters join the primary iliac lymph nodes and those of the pelvic ureters, the internal iliac and vesico-inferior lymph nodes.
The innervation of the ureters is rich and depends on the autonomic nervous system. It is derived from renal plexuses for the lumbar segments, hypogastric plexuses for the iliac and pelvic segments.