Introduction:
Introduction:
Acute renal failure (ARI) is defined in general terms as a sudden decrease in renal function, sufficient to lead to nitrogen waste retention and disrupt hydroelectrolytic homeostasis. While this qualitative definition is generally accepted, there is no consensus on the quantitative importance of the decrease in renal function necessary for the diagnosis of ARI. Commonly used definitions include an increase in serum creatinine (S Cr ) of the order of 50 μmol / l or more from its baseline value or a 50% or more reduction in calculated creatinine clearance. The clinician should keep in mind that in patients with normal renal function, S Cr is a poor indicator of a change in renal function. Significant reductions in glomerular filtration rate (DFG) initially produced only small increases (10 to 25 μmol / l) of S Cr . As a result, even small increases in S cr should be carefully considered.
ARI is frequently encountered in medical practice today, particularly in inpatients. A wide range of pathophysiological events leads to identical ARI clinical pictures.
The regression or attenuation of an ARI requires rapid identification and treatment of the underlying condition.
Moderate forms of ARI are often reversible and several studies have shown a direct relationship between the magnitude of S Cr increase and IRA mortality.
Any increase, even moderate, in S Cr therefore requires a complete clinical evaluation. In this chapter we review the clinical and biological characteristics of the various causes of ARI and propose an approach to ensure the earliest diagnosis.
Circumstances of discovery of acute renal failure:
ARI is most often diagnosed in the presence of an increase in CrS or blood urea. Typically, the blood urea / S Cr molar ratio is about 50: 1 and the mass ratio is about 15: 1. In the event of complete disruption of glomerular filtration, blood urea and S Cr increase daily of about 1.5-2.5 μmol / l and 90-130 μmol / l, respectively.
However, there are several situations that preferentially affect the concentration of blood urea or that of S Cr , which alters the ratio between the two values. In addition, factors other than a reduction in GFR may lead to an increase in blood urea (eg, catabolic status) or S Cr (eg rhabdomyolysis or drugs that interfere with the excretion of creatinine or its measurement).
S- Cr is usually a better marker for GFR than blood urea. At steady state, S Cr is approximately doubled whenever GFR is reduced by 50%.
For example, at steady state, GFR of 100, 50, 25 and 12.5 ml / min are correlated to S Cr of 90, 180, 270 and 360 μmol / l, respectively. However, ARI is usually not a state of equilibrium because the factors that determine S Cr(production, volume of distribution and renal clearance) vary. In addition, the increase in S Cr occurs with a lag time compared to the process leading to the IRA.
Unfortunately, techniques that allow real-time monitoring of DFG are expensive and are not routinely available. In some intensive care units, the GFR is used to collect urine samples at short intervals, for short periods of time and according to a precise chronology. The reliability of this approach remains to be established.
The installation of an IRA can also be recognized through a decrease in urine output. The presence of an oliguria (<400 ml / 24 h) or anuria (absence of urine) testifies to an ARI. Most cases of ARI encountered in current clinical practice are inherently accompanied by diuresis preservation. Recent clinical studies have shown that urine production is strongly correlated to residual glomerular filtration but little to tubular function. The higher level of residual glomerular filtration observed in non-oliguric patients is associated with lower severity of renal insufficiency and lower mortality than in oliguric IRA.
ARI may be detected either by biological abnormalities (hyperkalaemia, acidosis, hypocalcaemia, hyperphosphatemia, hypermagnesaemia, anemia) or by clinical signs (fluid overload, psychic disturbances, nausea, anorexia, pericarditis) are the consequence.
In clinical practice, it may be difficult to determine whether a high concentration of S Cr or blood urea is due to an acute process or a chronic process. A review of past laboratory history and results is essential in this context. If there is no previous result, the clinician must prioritize the assumptions that lead to possible treatment. The small size of the kidneys (<10 cm) in imaging is an argument in favor of the diagnosis of chronic nephropathy. The non-enzymatic carbamylation of the terminal valine of hemoglobin is proportional to the duration and intensity of the increase in blood urea. A recent study of 28 patients with ARI and 13 patients with chronic renal failure showed that a carbamylvaline level of less than 80 μg per gram of hemoglobin had a sensitivity and specificity of 96% and 84.2%, respectively, for the differential diagnosis between ARI and chronic renal failure.
Causes of acute renal failure:
Traditionally, the IRA is classified as prerenal, intrarenal or postrenal.
Prenary (or functional) acute renal impairment:
The IRA is referred to as prerenal if the cause of filtration failure is related to renal hypoperfusion. Prenal processes are the most frequently encountered causes of ARI. When unrestrained, prerial IRA may progress to acute ischemic tubular necrosis (NTA). In the prerenal IRA, decreased renal perfusion pressure, constriction of afferent arterioles, or dilation of efferent arterioles have the effect of decreasing glomerular hydrostatic pressure.
Events which decrease the renal perfusion pressure may be extracellular hypovolemia, linked to loss (by vomiting, diarrhea, haemorrhage, gastric aspiration by nasal catheter, burning, heat stroke, diuresis, etc.) or by sequestration (by rhabdomyolysis, pancreatitis, septic state beginner, intra-abdominal surgery …); decreased cardiac output; or taking antihypertensive drugs.
A constriction of the afferent arterioles may be caused by an increase in vasoconstrictor factors (eg, circulating adrenaline, angiotensin II, endothelin, increased renal adrenergic neurotransmission) or a decrease in vasodilating agents (nitric oxide, bradykinin, eicosanoids) . These changes may be due to drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs), ciclosporin, radiological contrast agents or amphotericin B; they may be encountered during the postoperative period, early infections, hepatocellular insufficiency, edematous diseases or hypovolemic states.
Vasodilatation of efferent arterioles is induced by the use of angiotensin converting enzyme or angiotensin receptor blockers.
An unusual cause of “prerenal” IRA is hyperoncotic state. The glomerular filtration pressure is equal to the glomerular hydrostatic pressure decreased by the oncotic plasma pressure due to the colloids. The injection of osmotically active substances such as mannitol, dextran or proteins can increase the oncotic pressure sufficiently to make the latter higher than the glomerular capillary hydrostatic pressure. This results in an interruption of the glomerular filtration leading to an anuric form of IRA, which eliminates the substance causing the disturbance.
Postrenal (or obstructive) acute renal insufficiency
Postoperative causes (after the formation of the glomerular filtrate) of ARI are less frequent than prerenal causes, but almost always accessible to treatment.
The postrenal forms of IRA are divided into intrarenal (tubular) and extrarenal. Tubular precipitation of insoluble crystals (methotrexate, aciclovir, sulfonamides, indinavir, uric acid, triamterene, oxalic acid) or proteins (as in myeloma or other plasma dyscrasias) may increase the intratubular pressure. When it is high enough, it opposes the glomerular filtration pressure and may decrease GFR. Similarly, an obstruction of the extrarenal collector system at any level (pelvic, ureter, bladder, or urethra) can also lead to a postrenal IRA.
Acute renal failure intrarenal (or parenchymatous):
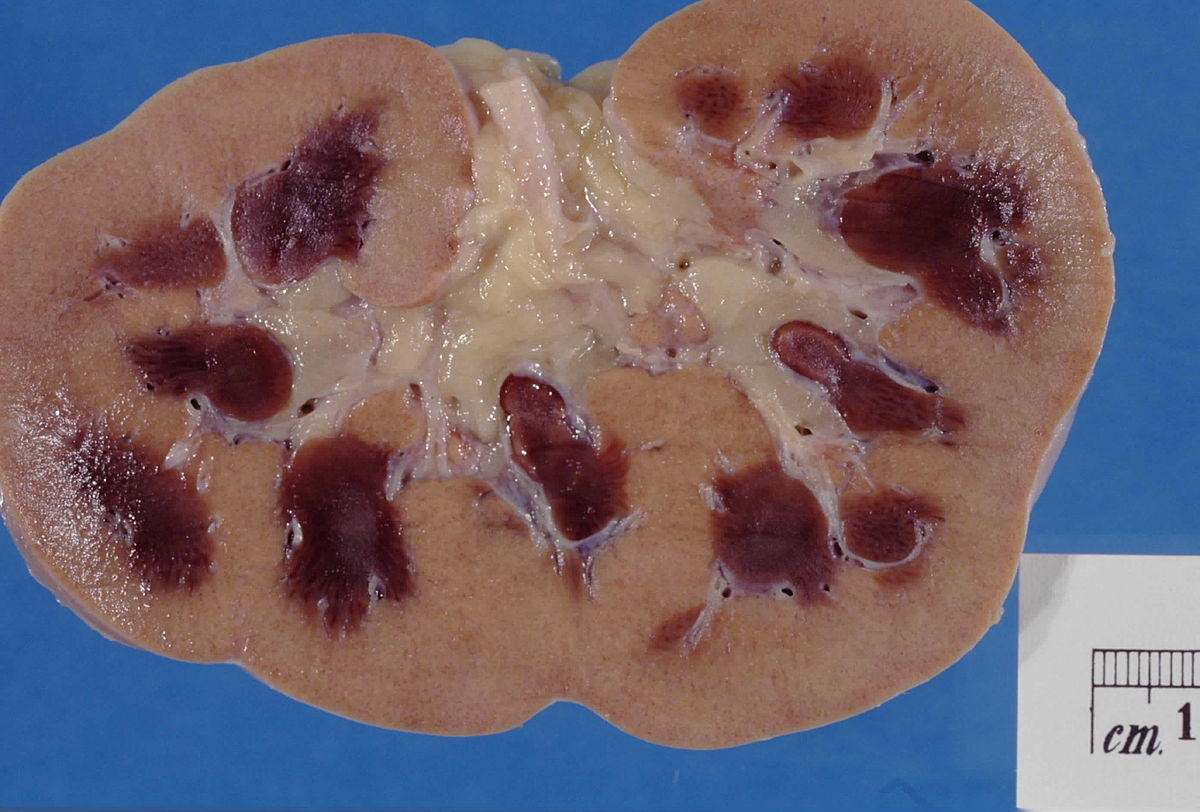
After considering the prerenal and posterior causes, the clinician must turn to the intrarenal causes of ARI. It is relevant to consider kidney causes in terms of anatomical compartments. Among the possible causes of ARI, microangiopathies (in some vasculitis, thrombotic thrombocytopenic purpura [PTT], hemolytic uremic syndrome [HUS], malignant arterial hypertension, eclampsia, disseminated intravascular coagulation [CIVD scleroderma, postpartum …) and diseases affecting large arteries (thrombosis, embolism …) or renal veins (acute occlusion). All forms of acute glomerulonephritis can be revealed by ARI. Acute inflammation and all processes occupying space in renal tissue (in relation to a drug, infection, autoimmune disease, leukemia, lymphoma, sarcoidosis …) may lead to ARI. Finally, ARI is quite frequent in relation to a tubular lesion or NTA, the usual causes of which are renal ischemia due to prolonged IRA prolonged, the use of nephrotoxic products (iodinated contrast agents, aminoglycosides, pentamidine , foscarnet, cisplatin, amphotericin, NSAIDs, heavy metals, hydrocarbons …) or pigmenturia (intravascular haemolysis, rhabdomyolysis).
Diagnostic approach to acute renal failure:
Background and study of previous documents:
It may be useful to consider the context in which the IRA has developed. For example, an ARI in town medicine can most often be attributed to a single cause (usually prerenal, postrenal or drug-induced) and its prognosis is good.Conversely, an ARI acquired in hospitals develops in a context of comorbidities; it is often multifactorial and associated with higher mortality. The ARI acquired in an intensive care unit is almost always multifactorial and often associated with a severe infectious syndrome with multivisceral failure; mortality is even higher.
The causes of ARI can also be considered taking into account the underlying disease or the process in which it develops. There are specific causes of ARI associated with malignant diseases, human immunodeficiency virus (HIV) infection, pregnancy and post-operative or resuscitation situations.
With age, the renal function reserve decreases and comorbidities become frequent, which increases the risk of ARI.Researchers have shown that the incidence of ARI in community practice increased considerably after age 60 (multiplied by a factor of 3 to 8). Although this population of patients is exposed to all forms of ARI, pre-natal and postrenal causes are particularly common.
The existence of liver disease exposes patients to kidney damage with serious consequences: the process may have a prenenal etiology (aggressive diuretic treatment, aspirate of a large volume of ascites, digestive hemorrhage, infection …) or renal (glomerulopathy , Ischemic or toxic NTA, interstitial nephritis, etc.). In addition, a significant number of patients with advanced hepatopathy develop intense renal vasoconstriction and a form of ARI (hepatorenal syndrome) that responds poorly to treatment and is associated with high mortality.
In order to determine the cause of the ARI, it is important to establish a history of the history of the disease, particularly by investigating events associated with loss or sequestration of intravascular volume or cardiac insufficiency. The notion of thirst, orthostatic discomfort or symptoms of congestive heart failure is an element that advocates an IRA of prenenal etiology.
The postrenal causes of ARI are frequent in infants and elderly. The anamnestic or clinical elements evoked are a loss of the flow or force of the urine; bladder, prostate or pelvic cancer; the use of anticholinergic or adrenergic drugs; the existence of anuria, supra-pubic pain or urinary stones; the administration of treatments known to cause hyperuricemia or crystalluria. The existence of a single kidney or a preexisting large decrease in kidney function should make the clinician particularly vigilant with regard to postrenal ARI because a single lesion may be sufficient to clog the kidney alone functional.
The concept of cardiovascular risk factors (smoking, hypertension, diabetes, hyperlipidemia, intermittent claudication, stroke, myocardial infarction, peripheral vascular disease, arterial catheterization involving the aorta, aortic aneurysm, atrial fibrillation) is suggestive of a vascular embolism that could cause the IRA.
The history of systemic infection or the presence of systemic symptoms may be in favor of an ARI of glomerular cause.Exposure to certain medications, symptoms of systemic infection or a history of acute pyelonephritis may lead to acute interstitial nephritis as a cause of ARI. Pathological situations associated with rhabdomyolysis or intravascular haemolysis suggest the possibility of pigmenturia that has contributed to ARI.
In all cases of ARI, a careful review of medications and possible exposures to toxicants is essential.
Various studies have shown that up to 25% of all ARI cases can be attributed to exposure to nephrotoxic agents.
Physical examination:
Clinical examination remains an important diagnostic tool to determine the cause of ARI. The determination of blood volume is essential in these patients but sometimes difficult. A meta-analysis of physical signs indicated that after 1 minute of orthostatism, an increase in heart rate (> 30 pulses / min) or a decrease in systolic blood pressure (> 20 mmHg) dryness of the axillary and buccal mucosa and a cracked tongue have good diagnostic value in favor of hypovolemia. The persistence of the skin fold or the slowness of capillary cutaneous recoloration present a limited sensitivity and specificity.
Ophthalmologic examination may reveal retinal arterial occlusion by cholesterol crystals (Hollenhorst plaques) suggestive of atheromatous embolisms or signs suggestive of bacterial endocarditis, vasculitis or malignant arterial hypertension. The examination of the neck allows the search for turgor of the jugular veins, palpation of the carotid pulse and auscultation of the carotids, which can provide useful elements for the diagnosis of heart failure, aortic valvulopathy or vascular disease.
Auscultation of the heart determines heart rate and rhythm, and looks for breathing, galloping or friction, which may contribute to the diagnosis of heart failure or the discovery of possible sources of embolism (fibrillation atrial, endocarditis …). Examination of the lungs may help to determine the presence of heart failure or a Good Pasture pneumorenal syndrome associated with an ARI. Abdominal examination may provide evidence for vascular disease (eg, perception of a breath or palpation of a mass related to an abdominal aortic aneurysm) or may lead to the discovery of an abnormal mass potentially malignant, bladder distention suggestive of downstream obstruction or a possible portal for bacteraemia, signs of liver disease (eg ascites, collateral venous circulation, hepatosplenomegaly).Examination of extremities in search of symmetry and pulse strength (vascular disease) or edema may be contributory.Examination of the skin may reveal palpable purpura (vasculitis), fine maculopapular eruption (interstitial nephritis induced by a drug) or livedo reticularis and emboli stigma (atheromatous embolism). In the presence of signs of neurological disease, systemic diseases such as vasculitis, PTT, subacute bacterial endocarditis or malignant hypertension should be considered. In combination with an ARI, peripheral neuropathy raises the hypotheses of nerve compression caused by rhabdomyolysis, ischemia, heavy metal poisoning or plasma cell dyscrasia. Pelvic touch in women and rectal examination can detect an obstructive cause of ARI.
Laboratory data:
A study of the hemogram may be useful in determining the cause of an ARI. Anemia may be related to recent haemorrhage or intravascular haemolysis that may have contributed to ARI. A microangiopathic syndrome (thrombocytopenia, reticulocytosis, increased lactate dehydrogenases, red cell fragmentation) associated with an ARI is directed to PTT, HUS, eclampsia, vasculitis, malignant hypertension, HIV infection or certain drugs. Anemia with roll formation and IRA suggests the diagnosis of multiple myeloma.
Eosinophilia is compatible with atheromatous embolism, acute interstitial nephritis or periarteritis nodosa.
Leukopenia is common in patients with systemic lupus erythematosus (SLE) with ARI. Thrombocytopenia in the context of ARI is consistent with etiologies such as thrombotic microangiopathy, SLE, CIVD, rhabdomyolysis, hepatocellular insufficiency with hypersplenism, or heparin-induced thrombocytopenia. An abnormality of haemostasis tests such as lengthening of the Quick time or activated partial thromboplastin time (ACT) suggests an underlying hepatopathy (prolonged Quick Time), a CIVD (elongated Quick Time and TCA) antiphospholipids (elongated TCA), all of which can lead to an ARI.
Moderate hyperkalaemia (not exceeding 5.5 mEq / l) is the usual finding during ARI. A more pronounced hyperkalaemia suggests the possible involvement in RAI of rhabdomyolysis, tumor lysis syndrome, intravascular haemolysis, or the use of NSAIDs or ACE inhibitors of angiotensin.
Increases in creatine kinase, aminotransferase and lactic dehydrogenase levels are usually associated with rhabdomyolysis and tumor lysis syndromes. ARI is usually accompanied by moderate hyperuricemia (<100 mg / l), while much higher levels of uric acid are observed in tumor lysis syndrome, rhabdomyolysis and heat stroke. Discrete metabolic acidosis is a common consequence of ARI and is generally associated with a moderate increase (5-10 mEq / l) in the anionic hole. Deeper acidosis with a larger anionic hole may suggest ethylene glycol intoxication, rhabdomyolysis, or lactic acidosis associated with severe infectious syndrome.
Diuresis and Urinalysis:
Analysis of the quality and volume of urine is of crucial importance in the assessment of an ARI. Anuria signs the termination of glomerular filtration (by rapidly progressive glomerulonephritis, acute cortical necrosis or renal arterial occlusion) or complete obstruction of the urinary tract. Short episodes (<24-48 h) of deep oliguria (<100 ml / d) occur in some cases of NTA, particularly in the context of heat stroke. Prenary forms of ARI almost constantly contain oliguria (<400 ml / d), although non-oliguric forms have been described. The postrenal and renal forms of ARI may occur under various diuresis profiles, ranging from anuria to polyuria. As pointed out earlier, most ARI cases related to an NTA encountered in current medical practice are not oliguric.
The urinary band and urinary sediment study provide guidance on the etiology of an ARI. According to an earlier study, in almost 75% of these cases, simple tests provided useful information for diagnosis. As a general rule, an irradiation without urinary sediment abnormalities is a priori prerenal or postrenal cause. The presence of abnormalities, on the contrary, leads to a renal cause. Two studies, unconfirmed by the third, suggest a direct correlation between the presence and degree of simple urinary test abnormalities and the prognosis of ARI on the other. In the series of patients with ARI analyzed by Hou et al, the mortality was 15% if the urine tests were normal (probable prenenal cause) versus 35% otherwise (probable renal cause). However, more recent studies indicate that the presence in the urinary sediment of a significant number of cylinders and figurative elements is not incompatible with a typical clinical course of functional renal insufficiency.
The sensitivity of the urine strip, which is based on the reaction to orthotoluidin for the detection of hematuria, is about three red cells / field at high magnification. In the absence of microscopic hematuria, the reaction is also positive in cases of myoglobinuria or hemoglobinuria, both of which can lead to NTA.
The search for proteinuria by the strip only detects albumin. Acid precipitation with sulfosalicylic acid (Exton reagent) detects all types of proteins. The contrast between a low positivity of protein search by the strip and the detection of larger amounts by the acid precipitation reaction suggests the presence of light chains and should require electrophoresis of the urinary proteins for further evaluation. When the detection of proteinuria by the test strip is moderately or strongly positive during an ARI, a quantitative result must be obtained (either after collection of all the urine for a given time or by determining, in a sample collected punctually, the albumin / creatinine ratio).
Proteinuria greater than 1-2 g / d is suggestive of glomerular IAR.
Cytological examination of the urine provides valuable information. The presence of macroscopic or microscopic haematuria suggests a parenchymal cause, whether glomerular, vascular, interstitial or other (calculation, tumor, infection, trauma …) and is rare in NTA. Much attention has been paid to the morphology of urinary erythrocytes as a key to the etiological diagnosis of hematuria. The morphological abnormalities observed in phase contrast, scanning or electron microscopy, or with the Coulter counter, were considered as the control of a glomerular process. More recently, it has been shown that optical microscopic observation of red blood cells with contours deformed by protrusions and protrusions of varying shape, sometimes shredded (red blood corpuscles of the Anglo-Saxons), was strongly suggestive of glomerular involvement. However, there are no specific data on the morphology of urinary erythrocytes in the ARI depending on its cause. The presence of significant leukocyturia is suggestive of pyelonephritis or interstitial nephritis. Recently, the quantitative cytological study of urine showed that significantly higher numbers of tubular cells and cylinders are observed in ARI-related NTAs than in ARI resulting from other causes. There was, however, a large overlap between the observed values, which limits sensitivity, specificity and predictive value.
Eosinophiluria is a useful semiotic element in the assessment of an ARI. The coloring of Hansel is superior to that of Wright. The presence of eosinophiluria (> 1% of urinary leukocytes) is not specific.
It occurs in acute interstitial nephritis, in many forms of glomerulonephritis, in atheromatous embolisms, urinary tract infections, prostatitis, acute kidney transplant rejection, or urinary tract obstruction. However, this sign has a diagnostic value when the ARI appears in a setting compatible with allergic interstitial nephritis (exposure to drugs, fever, rash, peripheral eosinophilia) or atheromatous embolism (vascular catheterization, presence of cholesterol embolism on the fundus of eye, livedo-reticularis, purple toes).
Erythrocytic cylinders present in the urinary sediment strongly suggest a glomerular or vascular cause of ARI, but they have also been observed in acute interstitial nephritis. Leukocyte cylinders may indicate the presence of pyelonephritis or other forms of acute interstitial nephritis.
The observation of crystals in the urinary sediment is an element of great diagnostic value during the ARI.
To be optimal, the search for crystals must be carried out by an experienced examiner, on a freshly emitted urine, under a polarizing microscope, taking into account the urinary pH. The presence of a large number of crystals of uric acid suggests acute uratic nephropathy, tumor lysis syndrome or catabolic IRA. Oxalate crystals are suggestive of IRA caused by ethylene glycol, by ileal resection or jejuno-ileal short-circuit, or by massive doses of vitamin C. The presence of drug-induced crystals resulting from the use of sulfonamides, indinavir or triamterene suggests that these may be the triggering cause of ARI.
Urine biochemistry and other urinary markers:
Interest and limitations of urinary biochemical analysis:
Randomized prospective studies have clearly established during the ARI the diagnostic utility of measurements of urinary concentration of electrolytes, uric acid and creatinine. The essential interest of these assays is to differentiate a pre-renal form of IRA from a renal form (especially NTA). Basically, pre-natal conditions are characterized by a retention of tubular functions, with high reabsorption of filtered salts and water as well as certain organic acids, resulting in low urinary concentrations of sodium, chlorine, lithium and uric acid, and relatively high urine / plasma (U / P) ratios for osmolality, urea and creatinine. Conversely, NTA is associated with a decrease in tubular functions resulting in elevated urinary concentrations of sodium, chlorine, lithium and uric acid and low U / P ratios for osmolality, l urea and creatinine. In general, the sodium excretion fraction (FE Na = U Na / P Na ) / (U Cr / P Cr ) Å ~ 100] is more sensitive than the urinary elements mentioned above to differentiate functional IRA of the NTA. However, a recent study showed that a small fraction of urea excretion (<0.35) may be more sensitive and specific than the fraction of sodium excretion to distinguish a pre-ARI from a renal ARI , particularly in the case of diuretics.
The use of urinary parameters to aid in the differential diagnosis of ARI requires certain precautions:
• there is no “gold standard” for the diagnosis of NTA, making definitive conclusions about the sensitivity and specificity of these indices difficult;
• despite their widespread use, no studies have shown that these parameters influence the management or progression of ARI;
• recent administration of diuretics may mislead urinary sodium;
• Nearly all studies have relied on parameters obtained on an ad hoc basis at a relatively late stage in the evolution of ARI. The IRA is undoubtedly a dynamic process by nature. For example, the tubular function is intact at the early phase of functional ARI.
If the cause (s) of the prenenal disease can not be rapidly controlled, an ischemic NTA can develop, altering the tubular functions. This sequence of events has been clearly documented in experimental ARI cases and may account for the low-EF NA reported in the early stages of ARI accompanying rhabdomyolysis, severe infectious syndromes, administration of contrast agents, non-oliguric ERI and exposure to NSAIDs;
• ultimately, the specificity of urinary biochemical indices is limited. Thus, at the beginning of the evolution of an obstruction of the urinary tract, of a glomerulonephritis or of a thrombotic microangiopathy, the FE Na may have values similar to those observed in the functional IRA.
Acute interstitial nephritis or acute occlusion of the renal arteries may give rise to indices that can not be distinguished from those of NTA. Similarly, indices identical to those observed in NTA are produced in the case of functional ARI associated with decreased tubular sodium reabsorption in relation to diuretic use or with bicarbonatura, glycosuria, mineralocorticoids or salt-lost nephropathy. Finally, although the excretion fraction of lithium appears to be a reliable index for identifying pre-ARI forms, it requires the application of specialized analytical techniques that limit its use.
Specialty Markers:
Two other categories of urinary markers were used as diagnostic elements of ARI. The first is the urinary excretion of enzymes present in the brush borders of nephron segments (for example the intestinal form of alkaline phosphatase, N-acetyl- b- glucosaminidase, alanine aminopeptidase). The second is the urinary excretion of low molecular weight proteins (eg, b 2 -microglobulin, amylase, lysozyme, retinol binding protein, $ 1 -macroglobulin) which are readily filtered and usually reabsorbed in the proximal tubule. In the case of a tubular lesion, the reabsorption capacity is decreased and an increase in the excretion of these enzymes and of these filtered low molecular weight proteins can be expected.
Although this is usually true, the measurement of urinary excretion of enzymes and small proteins has been shown to be insufficiently sensitive or insufficiently specific for its routine use in the diagnosis of the ARI mechanism.
Urine examination may also be useful when monoclonal gammopathy is suspected. Urine electrophoresis in search of light chains may be contributory. The use of antisera directed against light chains is more sensitive and more specific for the diagnosis of light chain nephropathy.
Recent research has identified another marker that may have an interest in distinguishing NTA from other causes of ARI. The kidney injury molecule (KIM-1) is a transmembrane protein synthesized by proximal tube cells. An increase in urinary levels of KIM-1 was observed during NTA. Further work is needed to confirm the clinical utility of this biomarker.
Obstruction of the urinary tract:
Postrenal ARI is particularly common in elderly patients and patients with ARI in the extra-hospital setting. The bladder and kidney ultrasound are the means usually used to detect obstruction. However, hydronephrosis may be minimal or absent in renal imaging, if the obstruction is very acute or in case of extensive retroperitoneal fibrosis.
A CT scan of the kidneys may be useful in identifying urinary tract obstruction and identifying its cause and extension.
Other tests:
It is sometimes difficult to assess blood volume and cardiac output even after careful observation, clinical examination and laboratory results. Other tests, such as chest x-ray and echocardiography, may therefore be indicated. The usefulness of pulmonary artery catheterization in the management of critically ill patients has been questioned.However, in carefully selected patients, this procedure can provide important information by allowing measurement of blood volume and filling pressures.
When glomerular or systemic diseases are suspected of being the cause of ARI, additional tests may be indicated: blood cultures, echocardiography and CT scan to detect the presence and origin of infection; assay of cytoplasmic antineutrophil antibodies, deoxyribonucleic acid (DNA), basal antimembrane, antistreptolysin O in an evocative context; viral hepatitis serology, assay of complement fractions, detection of circulating immune complexes (cryoglobulins, rheumatoid factor, C1q binding) as appropriate. In case of suspected vascular disease, doppler ultrasound or magnetic resonance angiography (MRI) may be useful for diagnosis.
Therapeutic Tests:
The response to a therapeutic intervention may represent a diagnostic test. Improvement of renal function after blood volume or cardiac output (through positive inotropic treatment or reduction of pre- or postload) is in favor of functional ARI; after catheterization of the bladder, placement of a ureteral probe or percutaneous nephrostomy, it suggests a postrenal cause; after interruption of NSAIDs or ACE inhibitors, it argues for an etiological role of these agents in the development of ARI.
When renal function improves in response to treatment with corticosteroids or other immunosuppressants, the diagnosis of allergic interstitial nephritis or allergic glomerulonephritis is preferred.
Anatomical examination:
Despite careful assessment, it is not always possible to determine the cause of an ARI with a reasonable degree of certainty. Clinical and paraclinical evaluation as described in this study provides a diagnosis in 75-80% of cases.Where this is not the case, a renal biopsy should be considered. Although there was no consensus on its indications, nephrologists turned to a biopsy when prerenal or postrenal causes were excluded and clinical and biological evaluation did not allow the diagnosis of NTA. The presence of functional or physical signs suggestive of systemic disease, significant proteinuria or erythrocyte cylinders is a potential indication for renal biopsy in patients with ARI.Anuria in the absence of obstruction, prolonged oliguria (2-3 weeks) and significant hypertension are also possible indications.
Several studies have examined the utility of renal biopsy in the assessment and management of ARI. In an earlier series, 84 patients for whom the diagnosis was NTA had a renal biopsy. The histological examination concluded in 52% of the cases with a glomerular pathology, 30% a tubulo-interstitial attack and 18% a vascular affection. The sensitivity of the clinical diagnosis of acute tubulo-interstitial disease was 77% and its specificity was 86%, compared with 56% and 66%, respectively, for the clinical diagnosis of acute glomerulopathy. In another series, renal biopsy was performed in 91 cases of ARI considered to be of renal origin. The cause of ARI was glomerular in about 20% of patients. The sensitivity of the etiologic diagnosis of ARI was 86% for acute tubulointerstitial diseases and 67% for glomerulonephritis.
Of 21 renal biopsies performed as a result of an ARI, Cohen et al. showed that prebiopsy clinical diagnosis was only corrected in one-third of the cases, but that biopsy results resulted in a significant change in treatment more than once.
Using the results of 259 consecutive renal biopsies performed as a result of ARI in patients 60 years of age or older, Haas et al. found that the most frequent diagnoses were pauci-immune glomerulonephritis (31%) or acute interstitial nephritis (18%), and that more than 90% of the biopsied samples had identified the cause of ARI.
The timing of renal biopsy in the ARI remains a critical issue. The classic indications have long been the lack of functional renal recovery and the persistence of anuria for several days. Currently, due to the problems raised by the irreversibility of many forms of glomerulonephritis or acute untreated interstitial nephropathies, there is a tendency to biopsy earlier in evolution as soon as the cause of ARI is not clear at the end of a careful clinical evaluation.
Synthesis:
Early detection and rapid and thorough evaluation of even minimal increases in S Cr are vitally important, as early intervention can help to alleviate renal insufficiency. The first elements of the evaluation are the history, the study of the medical record and the assessment of the clinical context. Completed by clinical examination, urinary tests and routine laboratory tests, these factors determine the cause of ARI in 40-60% of cases. Further investigations and possibly a therapeutic test provide the diagnosis in 20 to 30% of additional cases.
In other cases, a renal biopsy may be necessary.