Introduction :
Introduction :
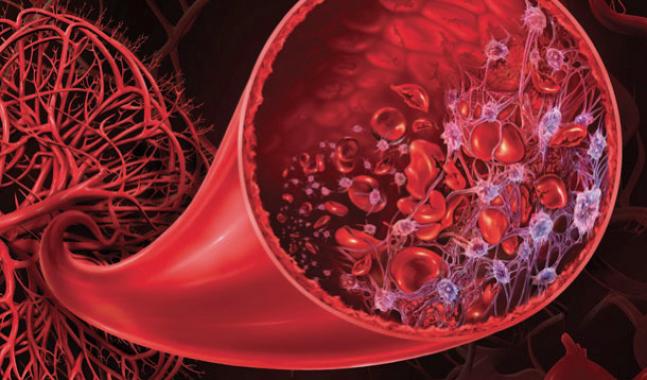
Here we detail the characteristics and recent data concerning the adult hemolytic uremic syndrome (HUS), thus completing the chapter on recently updated thrombotic microangiopathy, and the chapter on child HUS that is developed elsewhere.Thrombotic microangiopathy is an anatomoclinical syndrome consisting of a combination of microangiopathic haemolytic anemia, peripheral thrombocytopenia and thrombotic microvessel lesions. These diffuse microthromboses, which explain thrombocytopenia, create resistance to the passage of red blood cells that fragment into schizocytes.Thromboses can affect the brain and the kidney, but also the heart and almost all other vital organs.
Thrombotic microangiopathy include thrombotic thrombocytopenic purpura (TTP) on the one hand, and HUS on the other hand. PTT has an often abrupt onset and is characterized by the development of arteriolar or capillary thromboses in the brain, heart and other organs. Hypertension and severe renal failure are rare. This disease is due to congenital or acquired deficiency of ADAMTS13, von Willebrand factor protease.
HUS is a different entity in which renal involvement is predominant and in typical postinfectious forms is preceded by haemorrhagic diarrhea. The pathogenesis of HUS involves an endothelial lesion of infectious, toxic or immunological origin. Other pathology such as systemic lupus erythematosus, bone marrow transplantation or solid organ transplantation, chemotherapeutic treatments, consumption coagulopathy and metastasized cancers can also be complicated by thrombotic microangiopathy with variable neurological and renal impairment.
Pathophysiology:
Two phenomena seem to play an important role: intravascular platelet aggregation and the alteration of the property of the endothelial cell from antiplatelet platelet, antithrombotic and profibrinolytic activity to pro-aggregating, prothrombotic and antifibrinolytic activity. Different agents responsible for thrombotic microangiopathy, toxic, infectious or immunological can actually cause endothelial damage. Deficiency of local fibrinolytic activity in affected microvessels has been demonstrated, probably related to an excess of plasminogen activator inhibitor (PAI-1). In indirect immunofluorescence, we found evidence of PAI-1 within fibrin in thrombotic microangiopathy lesions in children and adults. However, the cascade of events between endothelial injury and microthrombosis is not always clear and seems different in HUS and PTT. In all cases, endothelial cell damage induces platelet aggregates, resulting in microthromboses.
Endothelial lesions and SHU related to shigatoxins:
Epidemic HUS associated with diarrhea are due to certain strains of pathogenic Enterobacteriaceae (Escherichia coli, Shigella dysenteriae, mainly Salmonella typhi) secreting bacterial enterotoxins. In 1977, Konowalchuk et al. isolated a toxin secreted by a strain of E. coli responsible for hemorrhagic diarrhea and HUS in children. This toxin has a cytotoxic effect on Vero cells, cells of the African green monkey kidney, and is called verotoxin or shigatoxin.
Most postdiarrheal HUS are due to infection with shiga toxin-producing E. coli 0157: H7 or serotype 1 S. dysenteriae. It has been shown that shigatoxins 1 and shigatoxins 2 can bind to a cell surface receptor on globotriaosylceramide (Gb3), to be internalized in the endosomes and to inhibit the elongation of the protein chains at the level of the transfer ribonucleic acid (RNA) on the ribosomes. This results in an inhibition of protein synthesis in target cells such as glomerular endothelial cells. The detachment, apoptosis or necrosis of these cells leads to exposure of the underlying, thrombogenic basement membrane, which will cause platelet activation and activation of coagulation.
This sequence of events is confirmed by the observation of endothelial swelling and detachment of endothelial cells, platelet adhesion to the basement membrane, and fibrin deposition in human or animal HUS lesions. More recently, SHU lesions have been induced by shigatoxin injection in ADAMTS-deficient mice13.
Shigatoxins can also be cytotoxic for mesangial cells and tubular kidney cells, thus contributing to the severity of renal failure. Shigatoxins increase the endothelial expression of adhesion molecules such as E selectin, ICAM-1 or VCAM-1 and promote adhesion of leukocytes and platelets. Finally, shigatoxins can increase the expression of interleukin-6 and MCP1 in the kidney as well as the expression of TNF- α and interleukin- 1b in monocyte macrophages. These cytokines increase the expression of Gb3 on the endothelial surface, making the cells more susceptible to the cytotoxic effect of shigatoxins. It has also been shown that shigatoxins can be transported by leukocytes from the colon to the kidney through the blood.
Patients with postdiarrheal HUS have a normal or moderately decreased level of ADAMTS13 and no circulating inhibitory antibody. In contrast to TTP lesions, thrombi in renal glomeruli during postdiarrheal HUS contain fibrin and platelets with very little von Willebrand factor. In the presence of ADAMTS13, increased shear forces associated with microvascular thromboses lead to increased cleavage of circulating von Willebrand factor, thus increasing low molecular weight forms.
Atypical endothelial and HUS lesions:
In atypical HUS without an enterotoxigenic secretion of verotoxin, the pathogenesis is different. It can be genetically transmitted and is often repetitive.
Atypical HUS in their familial form have been reported to mutations in one of three proteins involved in the regulation of activation of the alternative complement pathway. Some sporadic atypical HUS are also linked to this type of mutation.Two of these proteins, complement factor H and membrane cofactor CD46, are members of the regulation of the alternative complement pathway whose genes are located on chromosome 1 at the 1q32 position. These two proteins are factor I co-factors which is a circulating serine protease that cleaves and inactivates cell-surface bound C3b as well as C4b in the presence of a cofactor. These HUS are transmitted autosomically dominant with extremely variable penetrance. In addition, the homozygous factor H or factor I deficiency may be associated with the development of membranoproliferative glomerulonephritis without HUS. The reasons for these phenotypic variations in these patients remain unknown. A haplotype analysis suggested that the risk of atypical HUS could also be related to the factor H gene or the membrane protein cofactor protein (MCP), whereas no mutation was found in one or the other. other gene.The role of other regulatory factors of complement activation is not excluded. More rarely, autoantibody to factor H have been reported in patients with atypical HUS. These genetic abnormality sometimes remain asymptomatic, suggesting that they are susceptibility factors and that other factors, acting as a triggering factor, are necessary for the expression of the disease. How the activation of the alternative pathway causes the endothelial lesions is for the moment a question not completely solved. Similarly, why is the kidney the primary, if not exclusive, seat of thrombotic lesions? This could be related to higher expression of Gb3 for endothelial and renal vascular cells in postinfectious forms, or less ability to protect against complement activation and membrane attack complex.
The diagnosis of atypical HUS requires investigations of the alternate pathway of complement with a particular dosage of C3 and C4. Similarly, there may be a decrease in factor H and factor I levels or expression of MCP protein on the surface of leukocytes. However, sometimes complement activation is not always present and some mutations do not alter the expression of mutated proteins. Therefore, functional analyzes as well as detailed genetic study are often necessary to demonstrate the involvement of the regulation of complement activation in the pathogenesis of HUS.
Not all HUS are explained by endothelial lesions related to shigatoxins or a complement abnormality.
The endothelial lesion could also be of toxic origin after mitomycin C for example or autoimmune, since cytotoxic antibody endothelial antibody have been demonstrated in some cases of HUS.
In the PTT, on the other hand, there is no abnormality of the factor H, but a constitutional or acquired deficit of the von Willebrand factor protease activity. The complexes of high molecular weight, so-called ultralarges complex von Willebrand factor contained in the endothelial cells are released into the circulation where they cause platelet aggregation, and especially in the capillary where shear stress is important. In the acute phase of PTT, these ultralarges complexes are found in the blood of patients. It should be noted that in cases of familial PTT, these ultralarges complexes persist after the acute episode, suggesting that another cofactor would be required for PTT expression.
In circulating blood, ADAMTS13 is a zinc metalloprotease capable of cleaving von Willebrand factor provided that one or more of these cleavage sites are exposed by shear forces. An antithrombotic effect of ADAMTS13 has been perfectly demonstrated recently. Deficiency of ADAMTS13 results in the accumulation of high molecular weight multimeric forms of von Willebrand factor. These high molecular weight forms can be lengthened by shear forces and promote platelet adhesion and aggregation and formation of vascular microthromboses.
The high molecular weight forms of von Willebrand factor can be identified in the bloodstream with often in parallel a significant reduction in ADAMTS13 activity, less than 10% of the normal control value.
Large study have confirmed the prevalence of ADAMTS13 deficiency in patients with an acquired form of PTT, with the deficit being demonstrated in more than 80% of cases. The other cases correspond either to a PTT without deficit of the circulating protease whose pathophysiology is still undetermined or to different cases of thrombotic microangiopathy (MAT) such as systemic lupus erythematosus, metastatic cancers, nocturnal paroxysmal hemoglobinuria or syndromes. Atypical hemolytic uremic
Thrombospondin 1 may inhibit cleavage of von Willebrand factor by ADAMTS13 protease and may be implicated in the pathogenesis of some PTTs.
ADAMTS13 deficiency can be inherited or, more frequently, acquired.
In hereditary forms of ADAMTS13 deficiency, more than 55 mutations of the gene have been described. One of them, 4143insA, has been detected in both homozygous and heterozygous patients in several European family, suggesting that they may have a common ancestral precursor. In addition to the mutations, at least 26 polymorphisms have been described in the ADAMTS13 gene. These polymorphisms are sometimes associated with changes in the expression of ADAMTS13.
The deficits acquired in ADAMTS13 are much more frequent.
The presence of inhibitory antibody of this activity can be demonstrated in 50 to 90% of cases of acquired PTT. In patients whose inhibitory antibody are too low to be detected by inhibition of control plasma activity, enzyme-linked immunosorbent assay (Elisa) assays may be employed. Nevertheless, these tests can give false positives in 10 to 15% of the cases of the general population without PTT.
The causes of the appearance of these anti-ADAMTS13 inhibitory antibody remain poorly known and are sometimes favored by treatment with ticlopidine or clopidogrel or during infection with the human immunodeficiency virus (HIV).The level of ADAMTS13 sometimes remains low when there is clinical remission. These patients are at high risk of relapse. In chronic PTT, inhibitory anti-ADAMTS13 antibody persist at high levels preventing the rise of the circulating ADAMTS13 level. In these patients, rituximab, an anti-CD20 monoclonal antibody has been used successfully.
Clinical and biological signs:
Clinical signs:
This is a rare disease whose annual incidence in adults has been estimated at about 0.1 per 100,000. The most common symptoms include: asthenia, psychic disorders, purpura, hemorrhage, abdominal pain, fever.
Prodromic diarrhea, which is often bloody, is less than a few days old, and is suggestive of infection with pathogenic enterobacteria, but can also be seen in uninfected patients with colonic ischemia in the setting of microangiopathy.More rarely, jaundice, myalgia, arthralgia are noted. Central neurological disorders range from simple headache with confusion to motor deficits, aphasia, visual disturbances, seizures and coma.
Renal involvement, prominent in HUS and very common during PTT, is characterized by microscopic hematuria, more rarely macroscopic and proteinuria. Acute renal failure (ARF), often oligoanuric, is usually associated with severe hypertension (hypertension) and complicates 10 to 20% of adult HUS cases. The examination of the fundus can find papilled edema, retinal hemorrhages and vitreous. Retinal detachment is possible.
More rarely arrhythmia or heart failure, acute respiratory failure related to intra-alveolar haemorrhage, pancreatic diabetes, or rhabdomyolysis by muscular involvement are observed.
Biological signs:
Haemolytic anemia of the microangiopathic type is characteristic. It is an anemia, initially moderate, haemolytic mechanical type due to the fragmentation of red blood cells on microaggregates obstructing the small vessels, resulting in the formation of fragmented red blood cells or schizocytes.
At the same time, reticulocytosis is increased, as is the level of serum lactic dehydrogenase (LDH), hemoglobinemia, hemoglobinuria, unconjugated bilirubin. Serum haptoglobin is decreased. The Coombs test is negative.
The thrombocytopenia is constant, sometimes very deep (less than 10 000 platelets / mm 3 ), linked to a significant peripheral consumption not compensated by the increase of medullary production as evidenced by the increase of the megakaryocytes on the marrow smear.
There is no evidence of disseminated intravascular coagulation (DIC). Quick and activated partial thromboplast times are normal. Fibrinogen and other oagulation factors are normal in more than 90% of cases. There is, however, a slight increase in fibrin degradation products (PDF) in blood and urine, indicating minimal activation of fibrinolysis. A decrease in platelet aggregation in vitro has been shown to be related to preactivation of platelets in vivo.
A decrease in serum complement (CH50, C3 and C4) has been observed in some patients, this is uncommon but has an unfavorable prognosis. An assay of the various complement components including H factor, factor I, and MCP protein must be performed prior to any plasma transfusion. Similarly, a dosage of ADAMTS13, with inhibitor search, should be performed.
Anatomopathology:
Renal biopsy (PBR) during HUS with IRA is of diagnostic and prognostic value. Thrombocytopenia often prevents this procedure from being carried out percutaneously, but the transjugular renal biopsy technique now makes it possible to obtain good kidney fragments in these patients. The lesions can affect glomeruli, pre-glomerular arterioles and intrarenal artery.
Typical glomerular lesions involve swelling of endothelial cells and enlargement of the subendothelial space that reduces the diameter of glomerular capillary. Thrombi obstruct these capillary. They are composed of agglutinated and degranulated platelets and polymerized fibrin. Abundant deposits of PAI1, inhibitor of fibrinolysis, can be observed. The subendothelial clear deposits could correspond to plasma proteins accumulating at this level because of the increased permeability of the endothelial barrier. They could also represent platelet thrombi extensions from the injured capillary lumen. Rarely, mesangial expansion, inflammatory necrosis, or extracapillary proliferation are observed. In immunofluorescence, immunoglobulin G (IgG), IgM and complement deposits are present very inconsistently.
Arteriolar and arterial lesions are irregular and consist of thromboses made of platelet aggregates and fibrin, associated with intimal cell proliferation.
Unlike necrotizing vasculitis, there is no inflammatory reaction in and around the vessel wall. This arteriolar obstruction results in ischemic retraction of the glomeruli downstream. At most cortical necrosis is possible. Similar microcirculatory lesions have been demonstrated in other organs. Arterial lesions have a less favorable prognosis, and more or less severe renal failure may persist after the initial episode.
Other lesions, glomerular or vascular chronic, preexisting, can be discovered at the time of the HUS and are specific to each etiology. The existence, on the other hand, of an acute tubular necrosis on the biopsy is of favorable prognosis.
Treatment:
Management of renal failure:
The development of renal failure in patients with HUS requires very precise and regular monitoring of the state of hydration to avoid water-overload and episodes of hypertension and pulmonary edema. The use of dialysis may be necessary. In case of obvious overload, high-dose diuretics such as furosemide 125 to 500 mg by the venous route may be used to increase diuresis. Overdose can lead to episodes of dehydration that increase the risk of intrarenal microthrombosis. Subtractive dialysis or isolated ultrafiltration is generally more effective. Arterial hypertension should be treated with vasodilators and in particular angiotensin II receptor antagonists (ACE inhibitors) and / or angiotensin II receptor antagonists (ACE inhibitors), with or without calcium channel blockers or beta-blockers ; they most often allow the control of hypertension and decrease renal ischemia and the mechanical component of hemolysis. It is an essential component of symptomatic treatment with a strict blood pressure goal not exceeding 120 mmHg systolic. It is also necessary to avoid any nephrotoxic drug and opioid agents that can accumulate in case of kidney failure.Systematic treatment with folic acid can be given to help with the correction of anemia. Extrarenal complications of HUS must also be systematically detected.
Central neurological complications are sometimes severe and are important factors in morbidity and mortality. A brain scan or magnetic resonance imaging (MRI) is required for neurological manifestations.
In case of acute bloody diarrhea, patients must be admitted to the hospital and isolated. Intravenous rehydration and the maintenance of sufficient fluid intake can limit the severity of renal damage, especially if hydration is started before the onset of renal failure.
Antibiotics should not be given to these patients at the risk of increasing the frequency of HUS through a mechanism that remains poorly understood but probably involves massive bacterial lysis in the digestive lumen. Similarly, it is not recommended to administer digestive motility inhibitors or opiate derivatives as they also appear to increase the risk of HUS or neurological complications.
Patients who develop HUS can become fairly quickly severely anemic and transfusions may be necessary. However, they must be careful because they can promote high blood pressure. It is best to avoid platelet transfusions unless there is significant clinical bleeding or an invasive procedure.
Indeed, platelet infusions appear to aggravate microthromboses.
Kidney failure sometimes recovers completely after HUS but depending on the severity of the initial episode and the need for dialysis, sequelae remain possible in 10 to 30% of cases. In chronic renal failure, the disease usually goes away when the dialysis stage is reached.
Plasma exchanges:
The presentation of adult PTTs and HUS is often complex, and can not accurately predict whether it is an ADAMTS13 deficiency or other mechanism. It is therefore recommended in these forms to rapidly initiate plasma infusions or plasma exchanges and to monitor the clinical course. Of course, fresh plasma is the surrogate fluid that must be used during plasma exchange for these patients.
In adults, plasma exchange is the only treatment for which there is evidence of efficacy for the treatment of PTT. A prospective randomized trial compared plasma exchange with plasma perfusion. This trial demonstrated a significant improvement in survival at 6 months in patients receiving plasma exchange compared to those receiving plasma infusions. Some patients initially treated with plasma infusion have secondarily received plasma exchange with efficiency.
The initial response was also better in the plasma exchange arm. Plasma infusion remains useful in patients with TTP when plasma exchange can not be administered immediately.
It sometimes seems difficult to distinguish PTT from other diseases with thrombotic microangiopathy. Plasma exchanges are recommended in those for whom the diagnostic criteria for PTT are found. Their effectiveness in other cases remains uncertain or unlikely, as after bone marrow transplantation. Similarly, their efficacy in postdiarrheal or drug-related HUS remains unclear, although the retrospective study of Dundas suggests this. The optimal duration of treatment is still unknown.
The value of plasma exchange in atypical HUS related to factor H, factor I or CD46 deficiency is likely. However, a recent study does not show any benefit from plasma exchange in a short sery of patients with CD46 protein deficiency.
It appears that daily plasma exchange should be continued until the platelet count is stabilized and normal. The level of LDH that reflects both tissue ischemia and hemolysis is also a good marker of response to treatment. It is important to know the risks associated with the practice of plasma exchanges. In a cohort of 206 consecutive patients observed over a period of 9 years, 5 (or 2%) died from plasma exchange-related complications (3 haemorrhages related to central venous catheterization and 2 haemorrhagic sepsis). starting catheter); Another 53 patients (26%) had plasma exchange-related complications, including systemic infections, venous thrombosis, and hypotension requiring dopamine. However, given the benefit of this treatment in this disease, it is important to practice plasma exchange.
Immunosuppressants:
To prevent a rebound when plasma exchange is stopped or a relapse after a remission phase, corticosteroids should be prescribed in addition to plasma exchange (0.5 to 1 mg / kg / day until remission). Several study have confirmed the interest of glucocorticoids in this disease even if some patients were able to cure in the absence of corticosteroid treatment. Other immunosuppressive treatments are nowadays recommended in case of a resistant form such as monoclonal anti-CD20 antibody (rituximab), cyclophosphamide, vincristine or even cyclosporine. Quality clinical trials are lacking to specify the indications of these treatments.
Splenectomy or rituximab may decrease the frequency of relapses.
Other treatments (anticoagulants, aspirin, vitamin E, etc.) have not shown efficacy and are therefore not recommended.
Evolution and prognosis:
Adult HUS has a variable prognosis depending on the cause.
In the Tenon Hospital sery, we observed an immediate low mortality of 12.5% in patients with de novo HUS, and an excellent recovery of renal function in more than 70% of cases. Postinfectious HUS do not re-offend. On the other hand, those related to a deficiency of regulating factors of the alternate pathway of complement recidivate frequently and can lead to chronic renal failure (CKD) terminal. Life-threatening is very dark in HIV-positive patients with HUS, and the renal prognosis is poor in patients with underlying nephropathy. Independent mortality factors were positive HIV serology and the need for dialysis. Chronic hemodialysis is necessary in the absence of recovery of renal function, and renal transplantation should only be considered after a thorough assessment (see below).
Particular etiological circumstances:
They are numerous and varied in the adult.
In our sery of 55 cases of adult HUS, all confirmed by renal biopsy, the etiology found can be classified into two major groups: the so-called de novo HUS, that is to say on previously healthy kidney (72,7 %) and secondary HUS complicating underlying nephropathy (27.2%). This distinction is essential because the renal prognosis is radically different, recovery being the rule for de novo HUS, while chronic renal failure sometimes terminal may follow a HUS on anterior nephropathy.
Postinfectious or idiopathic forms:
The incidence of post-EHS HUS coli O157: H7 is particularly important in children. This postinfectious form exists nevertheless in the adult and even in the elderly and justify the systematic search for the toxin in the stool of all the patients presenting a HUS. The interval between ingestion of the contaminated food and the occurrence of diarrhea vary from 2 to 12 days. Typically, E. coli O157: H7 infections induce non-bloody diarrhea for 1 to 3 days, after which the diarrhea becomes bloody. Colic involvement can be relatively severe. However, there are also minor E. coli O157: H7 infections that have been found in patients without diarrhea. Most patients are not feverish during diarrhea, although they sometimes report the presence of fever in the initial phase.
The predominant cause of HUS in the world is E. coli O157: H7 infection, which can be detected by culturing faeces on agar medium containing sorbitol (MacConkey Agar). Commercial tests are also available for the direct detection of shigatoxin, possibly for different strains of O157: H7.
Thrombocytopenia is the first to appear in most patients, followed by hemolysis and renal failure.
Some risk factors have been well characterized such as leukocytosis, early symptom reporting, antibiotic administration or the use of antispasmodic agents.
Acute renal failure is often severe, oligoanuric, associated with hypertension, sometimes pulmonary edema.Proteinuria is usually between 1 and 2 g / 24 h but can be nephrotic. The ACB allows to recognize the forms with predominant arteriolar involvement, of worse prognosis than the forms with exclusive or predominant glomerular damage. Symptomatic treatment with hemodialysis and antihypertensives and aetiopathic treatment with fresh plasma in adults have upset the prognosis of these once catastrophic forms.
In addition to pathogenic enteric bacterial infections secreting shigatoxin, other bacterial infections can be complicated by HUS by a different mechanism. Thus, the pathophysiology of pneumococcal HUS is related to the production of an enzyme, neuraminidase, which exposes the Thomsen-Friedenreich antigen (AgTF) on the surface of erythrocytes, platelets and glomerular cells. The circulating anti-AgTF natural antibody recognize this antigen and this reaction is at the origin of the clinical and biological signs of HUS.
Many viruses (enteroviruses, HIV) and especially cytomegalovirus (CMV) in the transplanted patient are involved in triggering thrombotic microangiopathy. HIV infection and AIDS are risk factors for developing kidney disease, particularly hemolytic uremic syndrome. HUS in HIV patients is more common and more severe than in the general population and has high mortality. In a sery reported in our center, HIV accounted for one-third of HUS cases.Exceptionally, HIV-positive patients may develop an ADAMTS13 autoantibody deficit, but in most cases there is no obvious explanation for the development of thrombotic microangiopathy.
HIV or other associated viral infections, including CMV, are thought to promote the development of endothelial lesions.
Atypical hemolytic and uremic syndromes:
In addition to these postdiarrheal HUS, atypical HUS have been described without obvious prodrome, which accounts for about 20% of the child’s HUS. A fairly clear link has been established between these atypical HUS and mutations of the genes encoding regulatory proteins of the alternative complement pathway.
These mutations have been found in both familial and sporadic cases. These regulatory abnormality of the alternate pathway may be associated with hypocomplementemia with a decrease in C3. This is however inconsistent and is not necessary for diagnosis.
HUS linked to a mutation of the factor H gene:
There does not appear to be clinical heterogeneity linked to a specific type of mutation of the factor H gene. On the other hand, globally these atypical HUS have an extremely variable evolution, some having only one relapse without relapse with restitution ad integrum. renal function while others have successive episodes evolving towards end-stage renal failure.
The disease usually begins in childhood, but late-onset forms in adults have been reported. Forms found after end-stage renal failure have also been described in recurrence of HUS on a renal transplant.
Autoimmune forms of HF-related HF deficiency have been described with the characterization of anti-H antibody in children with atypical HUS. The circulating factor H activity was decreased in these patients and correlated for two of them with circulating anti-Factor H antibody. Antigen factor H and factor H were normal in all patients. Other autoantibody such as antinuclear factors were also quite common, even though there was no other autoimmune disease characterized. These forms may involve immunosuppressive therapy and plasma exchange.
SHU and CD46 protein or membrane cofactor protein:
Mutations in the MCP protein were initially described in familial forms of HUS with autosomal recessive inheritance.
The age of onset of the disease is variable, after a few months of life, in adolescence or in young adults. The first flare can progress immediately to end-stage renal failure.
In all cases, there is a decrease in membrane expression of the MCP protein.
SHU and factor I:
In patients with C3 levels without evidence of factor H mutation, it has been investigated and demonstrated factor I mutations in atypical HUS. Complete factor I deficiency has been described as a recessive disease usually associated with repeated pyogenic infections.
More recently, atypical HUS have been described in connection with Factor I mutations in the heterozygous state with sometimes late revelation, possibly in the postpartum period.
After relapse, end-stage renal failure usually leads to hemodialysis. Recurrence of HUS on a renal transplant has also been described.
Thus, more and more, atypical HUS can be related to often heterozygous mutations of regulatory proteins of the alternative complement pathway. There are, however, unexplained forms that may be mutations of other regulatory molecules, although no mutations have been found in patients with familial or sporadic HUS with respect to the CR1 gene or DAF protein (CD55).
SHU and ADAMTS13:
It is quite exceptional that a deficit in ADAMTS13, which characterizes PTT, leads to hemodialysis and no epidemiological data is currently available.
Renal impairment, limited to proteinuria and moderate renal failure can be observed in 20 to 30% of cases.
The clinical signs are extremely varied related to the presence of microthrombi in several organs. Approximately half of the patients with PTT have central neurological disorders quite severe from the outset or during the evolution of the disease such as seizures or focal motor deficits, possibly rapidly regressive. It is important to exclude at this stage other diseases such as severe sepsis, metastatic cancer or malignant hypertension.
There is no DIC. PTT predominates in women as adults. The risk appears to be increased in black and obese patients.
In the neonatal form of PTT, patients usually present with periodic episodes of thrombocytopenia and microangiopathic haemolytic anemia which improve quite rapidly with plasma infusion sometimes over several years. In less severe forms, PTT may appear later in life and relapse periodically. In a sery of 25 hereditary PTT cases, 30% of patients had chronic neurological deficits due to ischemic events. An ARI occurred at least once in five cases. In each case, however, this IRA was reversible in patients treated rapidly with plasma. CKD has also been described in patients with hereditary PTT who had not received a plasma infusion. A case of inherited PTT that has developed CKD has also been reported, possibly related to concomitant H factor deficiency.
SHU and pregnancy:
The SHU of pregnancy usually occurs during the third trimester of pregnancy and poses diagnostic problems with some forms of preeclampsia and haemolysis syndrome, elevated liver low platelet count enzymes (HELLP) where hypertension, proteinuria, microangiopathic haemolytic anemia, thrombocytopenia and insufficiency renal can be observed. CIVD signs absent in HUS are usually present in preeclampsia. In the absence of treatment, a fetal mortality of about 80% has been reported. Conversely, the infusion of fresh plasma has made it possible to control HUS, prolong pregnancy and considerably improve the fetal and maternal prognosis.
HUS can also appear in the postpartum after normal delivery and a symptom free interval of a few weeks to a few months. This postpartum HUS is often more severe than that during pregnancy, with frequent progression to end-stage renal failure. It seems that these severe forms correspond to the late revelation of a heterozygous factor H deficiency or, more rarely, factor I deficiency. PTT may also appear or recur during pregnancy. Maternal and fetal risk is low but needs to be known.
SHU and PTT cancers and after chemotherapy:
Signs suggestive of HUS or PTT have been observed in acute promyelocytic leukemias, prostate cancers, gastric or pancreatic carcinomas. Signs of CIVD are often associated and lesions may be related to tumor emboli. A recent study showed that 10 out of 351 patients who had been initially labeled as SHU or PTT and treated with plasma exchange had subsequently been shown to have diffuse metastatic cancer. These patients are distinguished from those with idiopathic PTT with a longer duration of evolution, more frequent respiratory signs, higher lactic dehydrogenases (LDH) and a poorer therapeutic response to plasma exchange. The diagnosis of cancer was made by bone marrow biopsy in six cases. In the literature, 19 other similar cases of HUS or PTT have been reported since 1965. Although rare, this table deserves to be known and justify bone marrow biopsy in case of doubt. HUS may be related to the disease itself or its treatment. HUS after chemotherapy were observed mainly in patients treated with mitomycin C and more recently gemcitabine. Other drug substances (cisplatin, bleomycin, vinblastine or vindesine) have also been implicated. The cessation of chemotherapy and plasma exchanges most often make it possible to effectively treat these HUS. The evolution is especially that of the cancerous disease.
Sometimes severe HUS or PTT has also been reported after marrow allograft, but the diagnostic criteria are sometimes unclear, so the actual incidence and consequences of these TADs are difficult to establish. A recent international consensus has been reached to define this syndrome and allow prospective study to evaluate risk factors and treatments. There does not seem to be a different variation of ADAMTS13 after marrow transplantation in the presence or absence of MAT. MAT post-marrow transplantation appears to be more frequent after intensive myeloablative dose (etoposide or busulfan, and cyclophosphamide, associated with total body irradiation, or even thiotepa, melphalan or carboplatin, and antilymphocyte serum), unrelated donor and induced T-cell depletion. by high doses of corticosteroids. Cyclosporin A given after transplantation can also be complicated by MAT.
Other medical causes:
Numerous drugs have also been implicated in cases of HUS on healthy kidneys: tacrolimus (1 to 5% of patients), ciclosporin A, interferon a , clopidogrel and quinine. All tables can be observed from simple histological findings to multi-organ failure. The mechanism is often not explained, but one can sometimes, as after taking a quinine, find in the patient’s serum different autoantibody, in particular against the glycoproteins of the platelet membrane GpIIbIIIa, but also against the erythrocytes, the leucocytes and endothelial cells. Renal MAT forms are currently reported with the new anti-vascular endothelial growth factor (VEGF) (bevacizumab) or VEGF tyrosine kinase inhibitors (sunitinib).
SHU and scleroderma:
The IRA of scleroderma is rare, but classic. It can occur, depending on the sery, in 10 to 40% of scleroderma patients. It is manifested by a HUS, most often with malignant HTA. Scleroderma, of the acrosclerosis type, is usually known at the onset of renal failure, but this can be revealing in 5 to 10% of cases. An increase in visceral signs, an alteration of the general state, an inflammatory syndrome can precede the “vasculorenal crisis”. Nonsteroidal anti-inflammatory drugs or corticosteroids have been implicated as a triggering factor. HTA, when present, may exceed 200/120 mmHg. However, despite severe kidney damage and an authentic HUS, some patients are not hypertensive.The fundus lesions are constant with dysoric nodules and / or retinal detachment, uncorrelated with the level of arterial pressure. Renal biopsy shows predominantly vascular lesions, mainly involving the interlobular artery, which are the site of circumferential proliferative or fibrotic endarteritis that reduces vascular lumen. The endarter is infiltrated by a mucoid material, rather characteristic of scleroderma or by fibrinoid material. Cortical and corticomedullary segmental necrosis is possible, also detectable by renal angiography. Later, nephroangiosclerosis lesions due to malignant hypertension can be superadded, mainly affecting pre- and post-glomerular arterioles with proliferative endarteritis and fibrinoid necrosis.
The prognosis of ARI in scleroderma, once catastrophic, remains pejorative, with up to 50% mortality in the first year due to stroke, heart failure or cachexia. It is improving since the use of IEC / ARAII. Hemodialysis and transplantation can be performed. Late recovery of renal function is observed after several weeks or months of hemodialysis, correction of blood pressure allowing slow regression of endarteritis and fibrinoid necrosis lesions.
Malignant nephroangiosclerosis:
It manifests as malignant hypertension with diastolic blood pressure greater than 130 mmHg, and major visceral repercussions. It can occur spontaneously, but most often follows an old HTA not or poorly controlled, regardless of the etiology. Sometimes it complicates the development of chronic glomerulonephritis and often marks the ultimate stage of nephropathy and renal failure.
Renal involvement is marked by an ARI or rapidly progressive, which can become oligoanuric. Most often, however, patients report a polyuropolydipsic phase receding their hospitalization, associated with asthenia and weight loss.Cachexia states can be installed quickly. Proteinuria is minimal. There is no hematuria.
Visual disturbances and fundal lesions are usual: haemorrhages, exudates, papilledema. Hypertensive encephalopathy is sometimes in the foreground with headache, confusion, somnolence, coma, general convulsions or cerebromeningeal hemorrhage. Left ventricular failure, related to the significant increase in peripheral vascular resistance, can lead to pulmonary edema.
Biologically, a haemolytic anemia of microangiopathic type is frequent; thrombocytopenia is absent or poorly marked.An increase in muscle enzymes (creatine phosphokinase [CPK], aldolase) may indicate muscle ischemia due to extreme peripheral vasoconstriction. Plasma renin is constantly extremely high. Plasma volume, which can be measured by isotopic dilution of iodine-labeled albumin or dilution of Evans blue, is often decreased due to HTA-induced polyuria.
After control of hypertension and haemostasis disorders, an ACB can be performed. It shows lesions characteristic of major proliferative endarteritis affecting the interlobular artery and especially the pre- and post-glomerular arterioles.The exuberant proliferation of smooth muscle cells in the intimal position results in the formation of the classic “onion bulb” lesions that can be found also in the HUS of scleroderma. More typically, necrosis of smooth muscle cells and fibrin infiltrates in the vascular wall can be observed, constituting fibrinoid necrosis lesions. Fibrinoid necrosis of the afferent arteriole, possibly extended to the glomerulus, is very characteristic of malignant nephroangiosclerosis and is not observed in other vascular nephropathy. Hyperplasia of the juxtaglomerular apparatus and an increase in the number of cells containing renin were observed.
The pathogenesis of malignant hypertension during malignant nephroangiosclerosis involves, above all, significant secretion of renin and intrarenal and systemic angiotensin II generation. Proliferative endarteritis and fibrinoid necrosis reduce vascular lumen and result in glomerular ischemia that causes renin secretion. This secretion of renin increases vasoconstriction and hypertension, increasing proliferative endarteritis, and therefore renal ischemia, which in turn stimulates renin secretion. A vicious circle of autoaggravation sets in, resulting in the malignant HTA with IRA. The lesions of proliferative endarteritis may be secondary to poorly controlled old hypertension, but they may also appear in young subjects with no particular history. This primary nephroangiosclerosis is similar to the vascular lesions observed in the spontaneously hypertensive rat (SHR), whose arterial and glomerular lesions appear and progress despite the control of hypertension. It could be a primary disease of the endothelial cell or smooth arterial muscle cell.
In addition to hemodialysis, which is used to correct hydroelectrolytic disorders, the treatment of ARF during malignant hypertension is mainly based on antihypertensive therapy.
The patient must be hospitalized in intensive care unit.
ACE inhibitors alone or in combination with other vasodilators, particularly AIIRAs, are also remarkably effective here and have completely replaced the previously necessary biphrectomy. Abrupt hypotension at the introduction of ACE inhibitors / ARA2, related to hypovolemia, may result in renal or cerebral retinal ischemia, so volume expansion must be associated. It is of course necessary to avoid diuretics and ultrafiltration at the beginning of treatment. The normalization of blood pressure is initially accompanied by a worsening of renal insufficiency, or even a reduction in diuresis. It is however essential to prevent the installation of new arteriolar lesions. This short-term worsening does not prevent a long-term improvement in renal function in a few weeks or months, sometimes interrupting dialysis treatment. This delay could correspond to the time required for the regression of proliferative endarteritis. During this period, iterative hemodialysis and antihypertensive therapy should be strictly maintained. The other etiopathogenic treatments (corticosteroids, fresh frozen plasma) have not been evaluated in this circumstance and do not seem justified to us.
SHU and lupus:
HUS or PTT may occur in systemic lupus erythematosus or antiphospholipid syndrome.
It has been reported for 2 to 8% of patients with lupus. It can occur at any age and sometimes precede the discovery of lupus. There are sometimes autoantibody to the von Willebrand factor protease. Immunosuppressive therapy and plasma exchange are effective in achieving remission of thrombotic microangiopathy.
HUS is a rare complication of antiphospholipid syndrome. There is usually severe hypertension, variable proteinuria, kidney failure. Glomerular capillary thromboses may be associated with arterial or arteriolar microthromboses. They progress to glomerular sclerosis and renal failure.
Immunosuppressive therapy and plasma exchange are usually used successfully.
SHU and renal transplant:
The frequency of HUS recurrence after kidney transplantation vary with the underlying cause. In all cases, whether it is de novo MAT or recurrence, this complication on the graft increases the risk of graft loss and mortality.
In a recent United States Renal Data System (USRDS) registry study, 29.2% of patients with chronic kidney disease were shown to develop thrombotic microangiopathy on their graft versus 0, 8% of patients with chronic renal disease of other origin. The incidence of thrombotic microangiopathy in renal transplant patients was 5.6 episodes per 1,000 people / year, with a higher incidence of recurrence than de novo MAT.
The risk of thrombotic microangiopathy is higher in the first 3 months after transplantation. Survival of the patient with thrombotic microangiopathy is approximately 50% at 3 years. In a collaborative study of the Ile-de-France Transplantation Cooperative Group (GCIF), recurrence of HUS after renal transplantation was studied in 16 patients with a primitive HUS, responsible for end-stage renal failure. This study showed an extremely high recurrence rate since 56% of the patients had a certain recurrence and 25% a possible recurrence. Recurrence was associated with a very poor prognosis of the transplant since renal transplant survival was less than 20% at 5 years. On the other hand, in the absence of recurrence, survival was comparable to other transplants. In children, there is no recurrence or quite exceptionally in patients who presented a typical postdiarrheal HUS (1 out of 137 grafts). On the other hand, this recurrence is much more frequent in case of atypical HUS (18 out of 77 grafts or 23%). It therefore seems possible to recommend a transplant in patients who have had a typical HUS associated with diarrhea. On the other hand, caution should be exercised in patients with atypical HUS, particularly in adults with hypocomplementemia and especially if a mutation of factor H or factor I has been demonstrated. In these cases, recidivism occurs in about 70% of cases.
There is no recurrence in patients with a mutation of the MCP protein, because this protein is expressed by the graft cells. Similarly, the exceptional cases of end-stage renal failure associated with von Willebrand factor protease deficiency are exposed to recurrence. In any case, it is best to avoid family donors who may also carry mutations and are predisposed to developing an HUS. Currently, it is proposed to perform the transplant under the guise of regular plasma infusions every 15 days to 3 weeks. This type of treatment could not be evaluated on large sery.