Introduction:
Introduction:
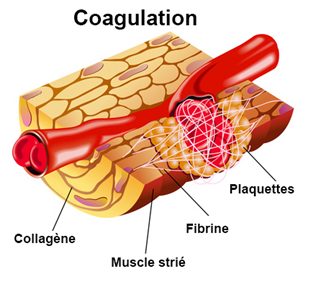
Chronic renal failure (CKD) is characterized by complex hemostasis disorders that coexist a bleeding tendency and a prothrombotic state.
Hemorrhagic manifestations:
Clinical diagnosis:
Hemorrhagic manifestations are often present in patients with CKD. These may be mild manifestations or extremely severe bleeding including haemorrhages of the gastrointestinal tract and subdural and retroperitoneal hematomas. In a study in 25 CKD patients treated conservatively and in 22 hemodialysis (HD) patients, the proportion of subjects with bruising was 32% in CKD patients, 41% in HD patients and 6% in a group. witness.Another study showed a frequency of hemorrhagic events of 24% in a group of 96 CKD patients taking no platelet antiaggregant and followed for 1 year. This bleeding tendency is further aggravated by heparinization performed during hemodialysis sessions.
Therapeutic advances such as reduced doses of heparin used for hemodialysis and the correction of anemia with erythropoietin (EPO) have reduced the frequency of bleeding in patients with CKD. However, the risk of bleeding is always a limitation to surgery and invasive procedures in these patients.
Biological diagnosis:
Bleeding time (SB) is still the test considered to be the most representative of the risk of bleeding.
This test is better correlated with hemorrhagic complications than platelet aggregation tests in vitro. TS is a global test that depends on all factors of primary haemostasis: platelet count and function, fibrinogen concentration, clotting factors, vascular function. The most used method for measuring TS is the technique of Ivy incision. A tension cuff maintains a constant pressure of 40 mm of mercury. An incision is made in a standardized manner on the anterior aspect of the forearm using a commercial device (Simplate ® ). The blood is collected every 30 seconds on a blotter without touching the vascular breach. The TS gives results sometimes not reproducible because it is influenced by the quality or the temperature of the skin, the technique of the operator and the cooperation of the patient. TS remains, however, the only test available and interpretable in practice. A study using this technique showed a mean TS of 10.6 ± 6.1 min in a group of subjects with CKD and 4.7 ± 0.9 min in healthy controls. Nearly half of patients with CKD have prolonged TS compared to controls.
In recent years, the industry has been offering a Platelet Function Analyzer (PFA) -based primary platelet function test that simulates in vitro the process of adherence and platelet aggregation after vascular injury. This test seems very sensitive but less specific than the TS. A study performed in 30 dialysis patients without hemorrhagic syndrome shows abnormal results in 60% of cases while TS is increased in only 20% of cases. It remains to demonstrate that PFA is predictive of hemorrhagic complications.
Etiology:
The pathophysiology of uremic bleeding is multifactorial.
It involves anemia, platelet abnormalities, and vascular abnormalities.
Anemia:
Anemia is one of the major factors in increasing bleeding time during CKD. In fact, the value of the hematocrit influences the platelet-vessel interaction by modifying platelet adhesion to the subendothelium. The correction of anemia by blood transfusions is associated with a decrease in TS.
Platelet abnormalities:
Platelet hypoaggregability:
It is observed in the presence of different agonists such as collagen, ristocetin and mechanical stress.
This hypoaggregability mainly involves abnormalities of platelet prostaglandins and abnormalities of GPIb and GPIIb / IIIa surface glycoprotein (GP) expression. Platelet GP abnormalities involve defects in intraplatelet signaling and GP release from the canalicular system.
Finally, the availability of GPIIb / IIIa can be reduced during IRC because these receptors are occupied by fragments of fibrinogen. Platelet hypoaggregability is probably due to uremic toxins. For normal platelets in the presence of uremic serum hypoaggregability is found while platelets of CKD patients in the presence of normal plasma regain normal functioning. The deleterious role of several toxins has been mentioned: guanidinosuccinic acid, methylguanidine and creatinine.
Thrombocytopenia:
This is not an anomaly classically associated with IRC.
One study, however, reported thrombocytopenia (<150 Å ~ 10 9 / l) in 31% of patients treated with HD and 9% of patients treated with peritoneal dialysis. Thrombocytopenia appears to be primarily associated with infection with the hepatitis C virus (HCV). In this case it is due to a mechanism of destruction-sequestration of platelets. Platelet-associated immunoglobulin (Ig) G was observed in 81% of HD HCV-infected patients and 42% of non-infected patients. A decrease in the medullary production of megakaryocytes is also involved, as evidenced by the decrease in reticulate platelets, which are the young platelets. This decrease in cross-linked platelets may also participate in platelet function disorders of CKD. EPO treatment appears to increase the percentage of crosslinked platelets. The data on cross-linked platelets during the CKD are, however, discordant because other studies show an increase in values, suggesting an acceleration of platelet turnover. Finally, heparin-induced thrombocytopenia may be evoked in patients treated with hemodialysis and having extremely prolonged exposure to heparin. However, heparin-induced thrombocytopenia is exceptional in these patients.
Vascular abnormalities:
Vascular abnormalities include von Willebrand factor abnormalities, prostaglandins, nitric oxide (NO), and fibrinolysis.
Von Willebrand factor (vWF) anomalies:
VWF is a multimeric glycoprotein of variable molecular weight resulting from the assembly of a 250 kDa subunit. It is synthesized by endothelial cells and megakaryocytes. In plasma, vWF forms a complex with factor VIII. Upon exposure of the subendothelium that follows an endothelial lesion, vWF binds to the subendothelial collagen and allows platelet adhesion by binding to GPIb. Circulating vWF intervenes in platelet aggregation by forming a bridge between platelets by its binding with GPIIb / IIIa. During the course of IRC, vWF is impaired by a loss of its high molecular weight multimers and a decrease in its platelet concentrations.
In contrast, plasma vWF levels are increased, as well as cofactor activity of ristocetin. Therapeutically, vWF is the target of two treatments capable of correcting hemostatic disorders during CKD: vasopressin leads to an increase in high molecular weight multimers of vWF and plasma vWF levels and decreases temporarily TS. It is also possible that the corrective effect of estrogen on hemostasis disorders involves an action on vWF.
Anomalies of Prostaglandins and Nitric Oxide (NO):
An increase in vascular prostacyclin production (PGI2) at the level of vascular lesions was described during the CKD.An increase in NO has also been reported. NO increases TS; it inhibits platelet adhesion to vascular endothelium as well as platelet aggregation. Data on NO levels in uremic patients are discordant. Most studies show decreased rates.Only Remuzzi and Noris report high rates. These authors point out that the administration to uremic rats of monomethyl-L-arginine (L-NMMA), which is an inhibitor of NO synthase, normalizes their TS and platelet dysfunction.Estrogen-induced reduction of TS in uremic rats would also be achieved by reducing the excessive synthesis of NO.Conjugated estrogens have long shown their ability to reduce bleeding in uremic patients.
Anomalies of fibrinolysis:
Chronic renal failure seems to be marked by hypofibrinolysis: a global test of fibrinolysis, the lysis time of euglobulins, is prolonged. Tissue plasminogen activator (tPA), produced mainly by the endothelium, is decreased, as well as plasminogen. The type 1 plasminogen activator inhibitor (PAI-1) which is the main inhibitor of fibrinolysis is increased.This increase is also observed on stimulated endothelial cells placed in the presence of uremic serum.
It seems, however, that some patients show an increase in fibrinolysis with an increase in tPA. Tranexamic acid (Exacyl ® ), an inhibitor of fibrinolysis, is able to reduce the lengthened TS of CKD patients. In a study in 37 CKD patients with TS prolongation, tranexamic acid decreased TS in more than 60% of patients. This drug decreases fibrin degradation products and plasmin / antiplasmin complexes.
Treatment:
Transfusions:
The first therapeutic measure for uremic bleeding is to correct anemia. TS is significantly improved by transfusions.
EPO:
EPO improves platelet adhesion and aggregation and phospholipid content of platelets. Malyszko reports an increase in blood and platelet serotonin levels. EPO decreases platelet content of cyclic AMP and enhances ATP release during platelet aggregation. EPO has been shown to normalize the increase of intraplatelet calcium in response to stimulation and thereby improve intraplatelet signaling. The treatment with EPO is able to improve the disorder of platelet adhesion and aggregation regardless of its effect on the red blood cell count. This effect could be due to the neutralization of certain toxins by red blood cells or a decrease in the production of toxins by better oxygenated tissues.
Desmopressin:
Desmopressin (Minirin ® ) is indicated for the correction of TS elongation during chronic renal failure. It is injected at a dose of 0.3 to 0.4 μg / kg (0.2 μg / kg in the elderly or with cardiovascular disorders).
It allows to temporarily decrease the TS. This effect is due to an increase in the high molecular weight multimers of vWF and plasma vWF levels. Successive injections are accompanied by an exhaustion of the effect. Desmopressin can be used before a kidney biopsy or surgery.
Tranexamic acid (Exacyl ® ):
Tranexamic acid reduces the lengthening of TS in CKD patients. Several observations have shown the value of tranexamic acid in CKD patients in the control of digestive bleeding or intracranial bleeding.
Recently a pilot study compared 20 episodes of severe bleeding from the upper digestive tract with tranexamic acid administration and 20 episodes without administration of tranexamic acid. A significant decrease in the rate of bleeding recurrence was observed in the group receiving this drug. Tranexamic acid is administered at a dose of 20 mg iv and then orally 10 mg / kg / 48 h for 4 weeks.
Estrogen:
The interest of injectable conjugated estrogens in reducing TS in patients with CKD has been known for a long time.
These injectable estrogens have not been marketed in France for several years. The active estrogen fraction on TS is represented by 17 beta-estradiol. It is possible that the application of transdermal beta-estradiol 17 is of interest. In a small study in six CKD patients, this drug reduced TS and symptomatic bleeding. Estradiol is administered percutaneously in patches of 50 to 100 μg / 24 h renewed every 3.5 days for 2 months. The mechanism of action of estrogens on hemostasis could be related to an effect on specific receptors on platelets, an inhibitory effect on NO, or an effect on vWF.
Thrombotic manifestations:
Clinical diagnosis:
Venous thromboses:
Deep vein thrombosis and pulmonary embolism are classically considered rare complications in CKD patients. In a study of 2255 autopsies between 1969 and 1981, the total frequency of pulmonary emboli was 32% in the general population (macroscopic in 4% of cases) and 9% in a group of 95 patients with CKD (macroscopic in 0% cases).Another autopsy study conducted between 1987 and 1996 showed a pulmonary embolism rate of 12% in a group of 185 CKD patients and 21% in 8051 subjects in the general population. These emboli were fatal in 6% of CKD patients and in 15% of non-CKD subjects. The annual prevalence of emboli remained stable throughout the study period despite the increasing proportion of patients treated with EPO. Only one recent study reports an increased risk of pulmonary embolism in dialysis patients. This is an analysis of the United States Renal Data System (USRDS) registry of 76,718 patients on dialysis in 1996. The incidence of hospitalizations for pulmonary embolism over a 1-year period was was 149/100 000 in these dialysis patients compared with an incidence of 24/100 000 in the general population.The relative risk of pulmonary embolism for dialysis patients was 2.11 after adjusting for age and excluding patients with known risk factors. This study requires confirmation to the extent that no radiological or autopsy argument has been requested for the diagnosis of pulmonary embolism. There are several publications of pulmonary embolisms in the form of isolated clinical cases. Most of these cases had classical risk factors for venous thromboembolism such as neoplasia, surgical follow-up, or prolonged hospitalization. There is no evidence that renal failure predisposes to venous thrombosis. However, it is possible that changes in the demographic and clinical characteristics of the dialysis population increase the risk of venous thrombosis and make this risk more similar to that of the general population.
Thrombosis of vascular access:
This is the most common thrombotic complication in hemodialysis patients. Vascular access thromboses are due to stenosis in 85-90% of cases. Among the 10-15% of non-stenotic thromboses, a number are due to an episode of hypotension or excessive compression of vascular access. Thrombosis due to hypercoagulability represents a minority of cases. Vascular access thromboses have been associated with a number of hypercoagulability markers which will be discussed below.
Stroke (stroke):
Strokes occurring in CKD patients are predominantly of haemorrhagic origin. The incidence of ischemic stroke is however higher than in the general population. A Japanese retrospective study in a population of 1,064 hemodialysis patients showed ischemic stroke incidence of 3.7 per 1,000 patient-years versus 0.95 per 1,000 patient-years in the general population.
The influence of hypercoagulability on stroke has not been studied during the CKD. One study focused on the frequency of stroke in patients with atrial fibrillation (AF). Curiously, in patients with CKD treated with hemodialysis, the existence of an AF is not accompanied by an increased risk of stroke.
Coronary accidents:
CRI is associated with an increased risk of coronary events. However, it is rather difficult to determine the respective share of hypercoagulability and atherosclerosis in the occurrence of a coronary event. In contrast, renal failure decreases the success rate of coronary angioplasty. Ischemic accidents occurring during the procedure are more frequent.
Etiology :
Activation of coagulation:
A large number of hypercoagulability markers have been described in patients with CKD. This is the increase of thrombin-antithrombin III complexes, fibrinogen, D-dimer, fibrinopeptide A, vWF, 1 + 2 fragments of thrombin and factor VII. This activation of coagulation may be due to the inflammatory state associated with CKD.
Decreased plasma levels of coagulation inhibitors:
A decrease in protein C has been reported, as well as antithrombin III, protein S, and resistance to activated protein C.These inhibitors of coagulation are reduced in 25 to 30% of the patients studied. These are acquired deficits that normalize after renal transplantation. The origin of these deficits is not clear. They could be related to the presence of substances that alter the synthesis or activity of coagulation inhibitors.
It is also possible that the renal parenchyma plays a role in the synthesis of inhibitors, which is reduced because of renal failure.
Increase in the prevalence of antiphospholipid antibodies:
The presence of lupus anticoagulant or anticardiolipin has been reported in 30% of patients in some series.
Platelet hyperaggregability:
It is present in some patients. An increase in the number of aggregated platelets has been reported, as well as an increase in the circulating level of platelet microparticles that possess their own procoagulant activity.
Clinical relevance of hypercoagulability markers:
We do not really know the clinical consequences of the presence of these hypercoagulability markers in CKD patients.No marker was clearly associated with the occurrence of venous or arterial thrombosis in these patients. The only associations between hypercoagulability markers and thrombotic events have been reported for vascular access thromboses, which are the most common events in these patients. Thus combinations have been described with the increase of fibrinogen, with protein C deficiency, or with the presence of lupus anticoagulant, or anticardiolipin.Increased levels of platelet microparticles appear to be associated with thrombotic complications, but these are not accurately described in the only study published to date. Further studies would be needed to establish the clinical consequences of the presence of circulating hypercoagulable markers. It must be emphasized that a large number of patients with these markers never have a thrombotic complication. The search for markers of hypercoagulability should therefore be done only in patients with recurrent thromboses.
Treatment:
The curative treatment of thrombotic complications of CKD patients differs from that of the general population because in these patients the haemorrhagic risk predominates. The treatment of venous thrombosis and arterial thrombotic events is based on heparin and oral anticoagulants.
Heparin therapy requires caution in patients with CKD. Low molecular weight heparins (LMWH) are eliminated renally and their half-life is increased during renal failure. The difficulty of adapting doses of LMWH during renal failure has led health safety authorities in France to prohibit the curative use of LMWH in case of renal insufficiency with a glomerular filtration rate of less than 30 ml. / min / 1.74 m 2 . In this case, unfractionated heparin must be used (French Agency for the Safety of Health Products [AFSSAPS], September 2000).
Preventive treatment of thromboses is debatable in CKD patients. If preventive treatment of venous thrombosis is to be initiated in a patient at risk, the AFSSAPS does not recommend the use of LMWH. The use of calciparin is preferable. The anticoagulant treatment of CKD patients with atrial fibrillation was discussed as one study did not show an increased risk of cerebral thrombotic events in this group of patients. This treatment remains however indicated currently. Preventive therapy is also discussed for vascular access thromboses for hemodialysis. These thrombotic events are the most common, but most of them have mechanical or hemodynamic causes (stenosis, hypotension). In the rare cases where recurrent thrombosis occurs in the absence of any mechanical or hemodynamic cause, some authors suggest that oral anticoagulant therapy be initiated. However, there is no study demonstrating the value of this treatment which is accompanied by an increase in the risk of bleeding. One study analyzed the survival of polytetrafluoroethylene (PTFE) prosthetic fistulas in 107 treated with either low dose warfarin with an international normalized ratio (INR) between 1.4 and 1.9, or placebo. Fistula survival was no better in the warfarin group, but the number of major bleeds was significantly higher. Further prospective studies are needed to demonstrate the value of anticoagulant therapy for the prevention of vascular access thrombosis. The place of antiplatelet agents is not always clear because they would act on the survival of vascular accesses more by preventing stenosis than by preventing thrombosis. A relatively old study has shown the interest of ticlopidine over placebo in reducing vascular access thrombosis. Another study prospectively analyzed the effect of antiaggregants in 107 patients by comparing dipyridamole, dipyridamole-aspirin, aspirin or placebo.
The relative risk of thrombosis was significantly decreased with dipyridamole. This study also suggested that aspirin alone increases the risk of vascular access thrombosis.
This could be due to an effect promoting aspirin on the proliferation of smooth muscle cells and intimal hyperplasia. A study of 200 hemodialysis patients with prosthetic fistulas who received either clopidogrel 75 mg and aspirin 325 mg, or placebo for nearly 1 year, did not show any benefit on fistula survival. In contrast, the number of subjects with hemorrhagic complications was 24% in the placebo group and 42% in the treated group.
Thromboses of hemodialysis catheters pose a specific problem and mechanical factors are in the foreground. A study of 98 tunneled catheters (Permcath ® and Vascath ® ), however, showed the superiority of aspirin 325 mg and warfarin (with an INR between 2 and 3) compared to no treatment to maintain patency. hemodialysis catheters. There is no difference between aspirin and warfarin in this study.
Conclusion:
Disturbances in hemostasis during chronic renal failure are dominated by bleeding complications.
Thrombotic complications occur in the presence of mechanical factors such as stenosis of a vascular access drainage vein for hemodialysis or atheromatous injury.
The risk of bleeding requires extreme caution in prescribing anticoagulants and in particular LMWHs that accumulate in case of renal failure.