INTRODUCTION:
INTRODUCTION:
Dysglobulinemias are characterized by the secretion in the blood of a monoclonal immunoglobulin or monoclonal immunoglobulin fragment. They may complicate a malignant hemopathy, whether it is myeloma, Waldenström disease or another condition involving the uncontrolled proliferation of a B lymphocyte clone, or occur as part of a benign B lymphocyte proliferation.
Monoclonal immunoglobulin or a fragment thereof is sometimes deposited in certain organs, and in particular in the kidneys, and modifies the structure and function of these organs. These deposits can be in various forms and the clinical consequences are very different depending on the type of deposit. The occurrence of this or that type of deposit depends primarily on the characteristics of the monoclonal immunoglobulin. Thus, the injection into the mouse of immunoglobulin light chains from patients with monoclonal dysglobulinemia may, depending on the light chain injected, not induce lesions, induce the formation of myelomaous cylinders, induce the formation of intratubular crystals, induce the appearance of fibril deposits having the histological characteristic of amyloid fibrils, or induce the deposition of light chains along the basement membranes. The type of renal damage also depends, to some extent, on the underlying hematologic disease and the various complications of dysglobulinemias do not occur with the same frequency in the course of various haemopathies.
We will describe successively: myelomatous tubulopathy; Fanconi syndrome associated with myeloma; amyloidosis;the disease of monoclonal immunoglobulin chain deposits; glomerulonephritis with intracapillary IgM thrombi.
Dysglobulinaemia can also be complicated by glomerulopathies related to cryoglobulinemia (type I or II) or glomerulonephritis with non-amyloid monotypic organized deposits (fibrillar glomerulonephritis and immunotactoid glomerulonephritis). These glomerulopathies being treated in detail in other chapters, we will not detail them.
MYELOMATUS TUBULOPATHY:
It is by far the most common renal complication of myeloma and, in two autopsy series of myelomatous tubulopathy lesions, it was present in 32 and 62% of patients, respectively. It is histologically characterized by the presence of “myelomatous cylinders” in tubular lumens, associated with lesions of the tubular cells.
Clinical and biological signs:
The diagnosis of myelomatous tubulopathy can be made either during the exploration of acute renal failure or in the event of progressive deterioration of renal function. In the first case, which is now the most common, renal failure usually reveals myeloma or shortly follows its discovery. Indeed, in the absence of renal insufficiency at the time of diagnosis, the likelihood of later developing acute renal failure has become relatively low. In the second case, renal failure occurs as a rule in a patient who is known to have myeloma.
The nephrological picture of myelomatous tubulopathy is poor: there is neither arterial hypertension nor edema; kidney failure is often severe, and in several recent series the mean creatinine at the time of diagnosis was greater than or equal to 800 μmol / L; there is no hematuria;
On the other hand, there is proteinuria, usually of high flow (greater than 2 g / day in half to two-thirds of cases), consisting essentially (almost always more than 70%) of light chains of immunoglobulins. The presence of albuminuria greater than 1 g / day must call into question the diagnosis and look for associated glomerular damage.
The presence of immunoglobulin light chains in the urine is not detected by the test strips and proteinuria must therefore be systematically sought in the laboratory. In contrast, the dissociation between proteinuria detected by the weight assay of urinary proteins and negative test strips should evoke the diagnosis of monoclonal gammopathy. The 24 hour proteinuria weighting should be supplemented by electrophoresis of the urinary proteins which shows a narrow peak in the globulin zone and by immunoelectrophoresis or immunofixation of the urinary proteins which confirms the presence in the urine of light chains. monoclonal and allows to specify the isotype. The Bence-Jones phenomenon (high temperature redissolution of light chains of immunoglobulins precipitated by heat) is only found in one out of every two cases and should no longer be used in clinical practice.
In addition to this nephrological chart are classic signs of myeloma, which is almost always a high-tumor myeloma (Salmon and Durie stage III in 70 to 80% of cases). Myeloma tubulopathy is a more common complication of light-chain myeloma and IgD myeloma.
Factors favoring the precipitation of light chains:
In more than half of patients with myeloma and acute renal failure, one or more factors can be found to promote intratubular precipitation of light chains. Their knowledge is crucial because it allows the implementation of extremely effective preventive measures. These are: hypercalcemia; extracellular dehydration whatever the cause (fever, diarrhea, vomiting, diuretic treatment, …); infections; nephrotoxic drugs, such as aminoglycosides and nonsteroidal anti-inflammatory drugs; iodinated contrast media.
Most of these factors favor the onset of dehydration with decreased renal perfusion and increased tubular reabsorption. Nonsteroidal anti-inflammatory drugs inhibit prostaglandin synthesis, which leads to a decrease in glomerular filtration in dehydrated patients and an increase in the corticomedullary osmotic gradient, thus promoting the precipitation of light chains. Iodinated contrast agents would bind to urinary proteins (Tamm-Horsfall protein and immunoglobulin light chains) and promote their precipitation.
Renal histology:
Renal biopsy should not be performed routinely in a patient with acute renal failure, whereas electrophoresis of serum or urinary proteins reveals a narrow peak. Except in very specific cases (absence of a narrow peak at electrophoresis of the proteins or need to estimate the renal prognosis as accurately as possible), it is only indicated if there is an albuminuria greater than 1 g / day and the other biopsies did not show amyloid deposition. The existence of an albuminuria greater than 1 g / day must indeed make search for the existence of a glomerulopathy.
If done, the renal biopsy shows characteristic cylinders and alterations of the tubular epithelium. In addition, there are often more or less important interstitial lesions.
The cylinders predominate in the deep cortex and the medulla, where they obstruct the lumen of the distal and collecting tubes. They are particular in their polychromatophilic character after Masson trichrome staining, by the presence of fracture lines in the cylinder body due to the presence of crystals and by their association with a gigantocellular contact reaction. The study of renal biopsy in immunofluorescence usually shows a staining of the cylinders exclusively by an antibody recognizing the monoclonal light chain (that is to say antikappa or antilambda).
The lesions of the tubular epithelium are constant. They usually interest not only the distal tubes but also the proximal tubes.
Interstitial lesions are common, whether it is an inflammatory cell reaction, a fibro-edema or fibrous lesions. When there are rupture zones of the tubular basement membranes, an intense macrophage cell reaction is observed around the broken tubes.
Treatment:
The treatment of myelomatous tubulopathies has two main components: on the one hand it is advisable to limit as much as possible the precipitation of light chains in the urine, and on the other hand, it is necessary to reduce the production of the light chains, thanks to a chemotherapy.
To limit the precipitation of light chains in the urine, it is necessary on the one hand to suppress all the favoring factors, and on the other hand to ensure the maintenance of a diuresis abundant (at least 3 L / d) and alkaline (with a ph urinary greater than 7 on all the nycthemeron). The maintenance of abundant diuresis dilutes the free light chains present in the urine. The alkalinization of the urine makes it possible to increase the solubility of the Tamm-Horsfall protein.
Chemotherapy should be started as early as possible. No chemotherapy has demonstrated superiority in renal or vital prognosis.
The classic melphalan-prednisone combination requires that melphalan doses be adjusted to renal function. Multidrug chemotherapy, type VAD (vincristineadriamycin-dexamethasone) induces earlier remissions and does not require that doses of drugs to the kidney function. The experience of heavy, so-called myeloablative treatments is still limited in patients with renal insufficiency.
The interest of plasmapheresis remains very controversial. Their theoretical justification is to rapidly decrease the level of circulating monoclonal immunoglobulin and therefore the elimination of light chains in the urine, but its clinical efficacy remains unstated. Two randomized studies suggest a benefit of plasma exchange in the most serious patients but do not establish it definitively.
In addition to the treatment of myeloma tubulopathy, there is of course the symptomatic treatment of renal failure. If necessary, the use of dialysis (hemodialysis or peritoneal dialysis) is clearly indicated in these patients, except probably in those whose myeloma is refractory to chemotherapy and therefore have a very short life expectancy.
Evolution and prognostic factors:
For reasons still unclear, the survival of myeloma patients is less when there is severe renal failure. In our series, mean survival was approximately 2 years in patients with normal creatinine, and only 5 months in those with renal impairment irreversible. Apart from renal failure, the tumor mass and the response to chemotherapy are the two essential prognostic factors.
With regard to renal prognosis, a significant improvement in renal function is observed in about 50% of cases, knowing that this improvement can be slow, delayed by several months. The usual clinical or biological factors do not reliably predict the reversibility of renal impairment at diagnosis. In our experience, as in that of other authors, the severity of interstitial lesions on renal biopsy has a significant prognostic value.
Pathophysiology:
Myeloma tubulopathy is secondary to the elimination of light chains in the urine, often in large quantities. For reasons still poorly understood, only certain light chains will induce myelomatous tubulopathy. This propensity to induce tubulopathy may involve the ability of light chains to bind Tamm-Horsfall protein and / or to self-regulate, or their resistance to the action of proteases. On the other hand, it is not related to the isotype of the light chains or their isoelectric point.
The renal failure results on the one hand from the formation of myeloma cylinders which will obstruct the tubular lumens and on the other hand from the direct induction of lesions of the tubular cells. The respective share of these two types of lesions in the genesis of renal failure varies from one patient to another. Myeloma cylinders are formed in the distal tubes by intratubular precipitation of light chains associated with Tamm-Horsfall protein. Tamm-Horsfall protein is a highly glycosylated, acidic 80 kDa protein that is synthesized exclusively by the cells of the broad ascending limb of Henle’s loop. It has the ability to form autogrégats and bind to some light chains. Certain factors such as reduced tubular flow, low urinary pH, increased urinary concentration of calcium ions or sodium chloride, furosemide, and iodinated contrast agents modulate Tamm-Horsfall’s light chain-protein interaction. and promote the formation of cylinders. The lesions of the tubular cells are of interest to both the cells of the distal tubes, where the cylinders are formed, and the proximal tubular cells. The light chains are normally reabsorbed by the proximal tubular cells, incorporated into endosomes that fuse with lysosomes, and degraded to amino acids by proteases. For reasons still poorly understood, some light chains can be toxic to tubular cells, as evidenced by the morphological and functional alterations they induce in these cells.
FANCONI SYNDROME ASSOCIATED WITH MYELOMA:
Fanconi syndrome is a condition characterized by the existence of proximal tubular transport abnormalities. Although, during the course of myeloma progression, discrete signs of proximal tube dysfunction can often be detected, the existence of Fanconi syndrome associated with myeloma is exceptional and to date less than 50 cases have been reported. This rarity of Fanconi syndrome suggests that its occurrence is only possible if the monoclonal light chains have very particular properties.
Clinical and biological signs:
Fanconi syndrome associated with myeloma usually occurs in patients over 50 years of age. It most often reveals myeloma and is usually discovered during the exploration of metabolic abnormalities, osteomalacia, or slowly progressive kidney failure.
Osteomalacia is present in about half of patients with Fanconi syndrome. It is responsible for bone pain and characteristic radiological abnormalities (increased skeletal transparency, Looser-Milkman bone fissures and sometimes bone deformities). It is primarily due to hypophosphoremia, but bone lesions are also favored by chronic acidosis and possibly abnormal vitamin D metabolism.
Biological examinations typically show normoglycemic glycosuria, increased clearance of phosphorus and uric acid, generalized aminoaciduria, metabolic acidosis and hypokalemia with inadequate kaliuresis, knowing that some of these metabolic abnormalities may be lacking. In addition, in about one in two cases, there is slowly progressive kidney failure.
In addition, immunofixation or immunoelectrophoresis of urinary proteins detect the presence of monoclonal free light chains which are most often of kappa type, whereas the monoclonal component is often not found in serum. The associated myeloma is usually a slow-growing myeloma (smoldering myeloma), revealed by Fanconi syndrome. In some cases, myeloma criteria may even be lacking and patients may initially be considered to have mild monoclonal gammopathy. More rarely, Fanconi syndrome can complicate the progression of lymphocytic lymphoma.
Histological lesions:
The histological lesions observed during Fanconi syndrome associated with myeloma mainly affect proximal tubular cells, site of reabsorption of light chains and their degradation by lysosomes.
In optical microscopy, the proximal tubular cells are typically enlarged in volume and filled with crystals. In some cases, however, the lesions are more discrete and it is a vacuolation of the proximal tubular cells, responsible for a “frosted glass” appearance, which attracts attention. These lesions are associated with nonspecific alterations of the proximal tubular cells (loss of height, loss of the brush border, desquamation) and sometimes fibrous and / or inflammatory interstitial lesions.
In immunofluorescence, there is usually a labeling of certain proximal tubular cells by the antibody corresponding to the light chain eliminated in the urine (that is to say antikappa or more rarely antilambda).
In electron microscopy, the proximal tubular cells present in their cytoplasm either rhomboid crystals located in the phagolysosomes, or vesicular bodies containing fibrillar, tubular, or rod structures.
It should be noted that crystalline inclusions are not limited to proximal tubular cells and that identical crystalline structures can also be demonstrated in tumor plasmocytes and sometimes in certain macrophages.
Treatment:
Due to its rarity, the treatment of Fanconi syndrome is poorly codified. Some studies, however, suggest that chemotherapy, which reduces the tumor mass secreting monoclonal immunoglobulin, may be effective on Fanconi syndrome.
Pathophysiology:
The rarity of Fanconi syndrome suggests that the light chains involved in the genesis of this syndrome have quite unique properties. The light chain study of five patients with Fanconi syndrome showed that variable fragments of these light chains were characterized by both their resistance to proteolytic enzymes and their ability to react with other light chains. In addition, in one patient, the proteolysis-resistant light chain fragment was able to form crystals in vitro. Proteolysis-resistant light chain fragments can be expected to accumulate within the lysosomal compartment of proximal tubular cells and form crystals.
The link between the accumulation of protein fragments in lysosomes and tubular transport abnormalities, on the other hand, remains poorly understood.
AMYLOSE AL:
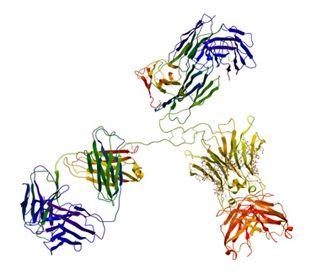
The term amyloidosis is used to characterize histologically defined lesions by the extracellular deposition of a protein material that has specific dye and ultrastructural characteristics. In optical microscopy, these deposits have an amorphous structure and are birefringent (yellow-green) in polarized light after staining with Congo red. In electron microscopy, they have a felted appearance and consist of aggregates of fibrils 7.5 to 10 nm in diameter, linear, rigid, unbranched, arranged in disordered clusters. Many proteins can give rise to such deposits and so there are multiple varieties of amyloidosis, including AL amyloidosis, which is amyloidosis associated with monoclonal dysglobulinemias.
AL amyloidosis is one of the most serious complications of dysglobulinemias since the average survival of patients with AL amyloidosis is of the order of 1 year. This complication is not exceptional and, in two autopsy series, amyloid deposits were present respectively in 5 and 11% of patients.
Structure of amyloid fibrils in AL amyloidosis:
Each amyloid fibril consists of two filaments 3 nm in diameter which have a β-pleated structure and are wound around each other, the β sheets being perpendicular to the axis of the filament. The variable domain of the monoclonal light chain is still the main constituent of the amyloid fibrils of AL amyloidosis, whereas the constant domain of the light chain is most often totally or partially absent. Amyloid fibrils also contain glycosaminoglycans and component P, in addition to monoclonal light chain fragments. The glycosaminoglycans are primarily heparan sulphates and could stabilize the structure of amyloid fibrils and allow the binding of component P. Component P is a homodimeric glycoprotein of β-pleated structure that could protect amyloid fibrils from the action of proteases.
Clinical and biological signs:
AL amyloidosis is almost always found in a subject over 40 years old, with a mean age of diagnosis of 65 years. The telltale signs are variable, but it is most often an alteration of the general state.
When the renal involvement is symptomatic, the nephrology table associates: a proteinuria, constant, with in about a third of the cases a nephrotic syndrome. This proteinuria consists of either albumin or both albumin and globulins.Unlike the proteinuria seen in most glomerulopathies, its flow rate does not usually decrease when kidney failure worsens; sometimes renal failure, which is present at the time of diagnosis in just under half of cases; an increase in size of the kidneys, visible on the kidney tomograms.
On the other hand, there is no hematuria (except in cases of associated urologic involvement) and there is usually no arterial hypertension.
These renal signs can be associated on the one hand an alteration of the general state and, on the other hand, extra-renal signs testifying to the systemic spread of the disease.
Monoclonal immunoglobulin or free light chains are found in serum or urine in 90% of patients with AL amyloidosis.The monoclonal light chain is twice as often a lambda light chain as a kappa light chain.
Despite the almost constant presence of a detectable monoclonal immunoglobulin in the blood or urine, only a minority of patients with AL amyloidosis have a known immunoproliferative disease. This is much more often a myeloma than another lymphocytic hemopathy B. Thus, in a study of 474 cases of AL amyloidosis, 15% had a proven myeloma, 56% had an abnormally high number of plasma cells in the bone marrow and 29% had amyloidosis considered primitive.
Renal histology:
In patients with amyloidosis, there may be impaired haemostasis by acquired factor X deficiency or increased fibrinolysis, which may render renal biopsy dangerous. Histological diagnosis should be made, if possible, by biopsy of accessory salivary glands, rectal submucosa, or subcutaneous fat.
Whatever the tissue considered, the existence of a yellow-green birefringence in polarized light after staining with Congo red makes it possible to diagnose amyloidosis. Only in case of doubt, and particularly when amyloid deposits are very discrete, should one resort to electron microscopy. The amyloid deposits then appear as fibrils 7.5 to 10 nm in diameter, entangled with each other but unbranched. The identification of the nature of the amyloid protein is based primarily on immunohistochemistry. In the case of AL amyloidosis, amyloid deposits are not recognized by AA antiprotein antibodies. They are sometimes stained by the antibodies directed against the monoclonal light chain, but this coloration is inconstant because of the frequent absence of all or part of the constant domain of the light chain in the fibrils. Moreover, in the case of AL amyloidosis, the birefringence observed after staining with Congo red does not disappear when the slides have been pretreated with potassium permanganate, unlike in AA amyloidosis.
In the kidney, amyloid deposits may be of interest to all structures, but they usually predominate in glomeruli where they first appear in the mesangium and then along the glomerular basement membrane (extramembranous or subendothelial). These deposits are associated neither with a proliferation of mesangial cells nor with an influx of inflammatory cells. They will gradually obliterate the floculus, transforming the glomerulus into an “amyloid sealing bread”. It should be noted that there is no correlation between the rate of proteinuria and the abundance of deposits.
Prognosis and evolution:
The prognosis of AL amyloidosis is extremely pejorative with an average survival of about 12 months, and less than a quarter of patients alive at 3 years. This survival would be even shorter in patients with myeloma, or in those with heart failure, orthostatic hypotension or digestive malabsorption. On the other hand, it does not appear that the existence of a renal impairment decreases survival.
Cardiac involvement is the leading cause of death, as it is responsible for at least 40% of them whether through rhythm disorders, conduction disorders or refractory heart failure.
For patients with end-stage renal disease, dialysis survival is poor but does not appear to be significantly different from the survival of patients with renal autonomy. The course of renal damage is sometimes precipitated by surgery, which may, for unknown reasons, lead to a sudden worsening of amyloid nephropathies.
Treatment:
The treatment of AL amyloidosis remains poorly codified, especially since there is no parallelism between the evolution of the clinical or biological manifestations of the disease and the evolution of amyloid deposits.
Chemotherapy to reduce the production of monoclonal light chains is logical in patients with myeloma but more questionable in those with so-called primitive amyloidosis. Three clinical trials prospectively and randomized the efficacy of melphalan-prednisone treatment in patients with primary amyloidosis without showing a clear benefit from such treatment. However, the most recent study suggests that some patients, who are probably those without severe visceral involvement, may be able to benefit from melphalanprednisone and colchicine combination therapy. The place of myeloablative heavy treatments remains to be clarified. Colchicine is used by some, by analogy with the treatment of familial Mediterranean fever, but its effectiveness has not really been established. Dimethylsulfoxide has been proposed to dissolve amyloid deposits, but has been found to be of little or no efficacy and poorly tolerated. Other treatments such as vitamin E or interferon alpha have also not been proven effective. A recent study suggests that a new anthracycline may be effective on the resorption of amyloid deposits.
Pathophysiology:
The possibility of inducing typical fibrillar deposits in mice by injection of light chains from patients with amyloidosis but not light chains from patients without amyloidosis shows that only certain light chains can induce AL amyloidosis. The characteristics of light chains that make them capable of inducing the formation of amyloid deposits are still poorly understood. A recent study suggests that the variable segment of light chains capable of forming amyloid fibrils could have a particular three-dimensional structure. Other authors have suggested that the affinity of light chains for some components of the extracellular matrix may play an important role.
DISEASE OF MONOCLONAL IMMUNOGLOBULIN CHAINS DISEASES:
The term Monoclonal Immunoglobulin Deposition Disease (or monoclonal immunoglobulin deposition disease) is used to refer to conditions involving unorganized deposits of monoclonal immunoglobulin fragments, whether they are isolated light chains. isolated heavy chains, or a combination of light chains and heavy chains. In fact, these deposits almost always consist of fragments of light chains either isolated, or more rarely (three cases out of 25 in a recent study) associated with heavy chain fragments and, to our knowledge, only six cases involving Heavy chains without light chain deposits have been reported to date.
Clinical and biological signs:
The average age of onset is about 50 years, but may affect younger patients.
Renal damage is constant and often revealing. Above all, it results in kidney failure, which is often in the foreground and worsens rapidly, often leading to dialysis in a few months; by a proteinuria variable flow, greater than 1 g / d in more than 70% of cases and 3 g / d in about 40% of cases.
To these signs may be added: microscopic hematuria, detected in about 30 to 50% of cases; and / or arterial hypertension, present in about one out of every two cases.
MIDD is a systemic disease and deposits can be found in multiple tissues. The most common extrarenal attacks appear to be hepatic, cardiac and neurological. Hepatic deposits may be responsible for hepatomegaly and liver function abnormalities that are usually moderate, but some patients develop sometimes severe hepatocellular insufficiency and / or portal hypertension. Cardiac deposits can result in simple cardiomegaly or cause heart failure.
Immunoelectrophoresis or immunofixation detect monoclonal immunoglobulin in blood or urine in only 70-85% of patients. The monoclonal light chain is then much more often of isotype kappa (80% of the cases approximately) than lambda. In other cases, the absence of detectable monoclonal immunoglobulin is probably due to the fact that the monoclonal component is rapidly deposited in the tissues.
The MIDD can complicate the evolution of a patent hematology and in this case it readily reveals the hematological disease. This is much more often a myeloma than a Waldenström disease. As in the case of AL amyloidosis, there may also be no detectable hematological malignancy and the MIDD may appear primitive.
Renal histology:
The diagnosis of MIDD is based on the demonstration, in immunofluorescence, of monotypic deposits of immunoglobulin chains on the basement membranes and in the mesangium.
In light microscopy, the MIDD associates tubular, interstitial and glomerular lesions. The tubular involvement is constant, characterized by a thickening of the tubular basement membranes which appear refracting, of ribbon aspect and are chromatophiles. Interstitial involvement is nonspecific, marked by fibrosis of varying intensity. Glomerular lesions are more heterogeneous. Most often, there is simply a thickening of the glomerular basement membranes that appear abnormally refractive and / or hypertrophy of the mesangial matrix.
However, in some cases, MIDD lesions achieve true nodular glomerulosclerosis with the presence of mesangial nodules that push back peripheral cell nuclei and may even stretch the capillary loops. In all cases, these deposits do not take the colorations of amyloidosis.
In immunofluorescence, the deposits along the tubular membranes are always intensely labeled with a single light antihamin antibody and more rarely with a heavy antihamin antibody. The glomerular deposits are less clearly marked and several cases of glomerular immunofluorescence have even been reported. This tubular and glomerular marking is associated with the labeling of vascular walls of arterioles and interlobular arteries.
The study of renal biopsies in electron microscopy reveals the deposits of immunoglobulin chains in the form of an electron-dense material of granular appearance.
Evolution:
The survival of patients with MIDD is highly variable, ranging from 1 month to 10 years, and in a retrospective study involving 19 patients, survival was 89% at 1 year and 70% at 5 years. It depends both on the consequences of visceral deposits of immunoglobulins and on the underlying hematological disease.
The renal prognosis is pejorative with often a rapid progression towards end-stage renal failure.
Treatment:
While the use of chemotherapy is logical in the presence of proven myeloma, it is more questionable in the absence of symptomatic haematological disease given the highly variable evolution of the MIDD. Two retrospective studies of a small number of patients, however, suggest that this chemotherapy may be beneficial. In the absence of a prospective study, it may be proposed to treat patients with either poor renal insufficiency or extrarenal manifestations of their disease. The treatment could then call for chemotherapy combining an alkylating agent and corticosteroids. On the other hand, when there is isolated kidney disease with already advanced renal insufficiency, chemotherapy is probably less useful.
A few patients with MIDD and dialysis were transplanted with usually recurrent MIDD on the graft.
Pathophysiology:
The study of the light chains produced by the plasma cells of patients suffering from MIDD made it possible to detect a certain number of abnormalities of these light chains. They may include structural abnormalities with abnormal size and / or presence of unusual amino acids in certain positions resulting in the formation of hydrophobic groups, be abnormally glycosylated in their N-terminal portion, or have a particular propensity to polymerize in particular. vitro.However, it is not known how these light chain abnormalities promote their deposition within tissues. Moreover, although the positivity of immunofluorescence deposits suggests that the constant domains of immunoglobulins are present in these deposits, the precise structure of immunoglobulin light chain fragments deposited in tissues remains unknown.
The factors responsible for nodular glomerulosclerosis associated with immunoglobulin chain deposits in the kidney are also poorly known. An in vitro study suggests that deposited immunoglobulin chains are able to stimulate extracellular matrix synthesis by mesangial cells, through an increase in TGF-β (transforming growth factor) production. By analogy with the role played by advanced glycation end products (AGEs) in the development of diabetic glomerulosclerosis, it is also possible that the abnormal glycation of certain light chains plays a role in the production of extracellular matrix .
NON-AMYLOID SMONOTYPIC ORGANIZED DEPOSITION GLOMERULOPATHIES:
Glomerulopathies with non-amyloidic organized deposits are the subject of a separate chapter. We will only briefly discuss the main features of these conditions, which in a number of cases complicate dysglobulinaemia.
The most common clinical presentation associates proteinuria, often of high flow, and microscopic hematuria.
The study of renal biopsy in light microscopy revealed either extramembranous glomerulonephritis, often associated with segmental mesangial proliferation, or lobular membranoproliferative glomerulonephritis. In fact, it is the study in electron microscopy that asserts the diagnosis. It shows deposits organized in fibrils (fibrillar glomerulopathies) or microtubules (immunotactoid glomerulopathies) in the mesangium and the walls of the glomerular capillaries. Fibrillar deposits differ from amyloid deposits both by the negativity of Congo red staining (due to the absence of β-pleated structure) and by the larger fibril diameter (12-20 nm instead of 7, 5 to 10 nm).
In some cases, especially if it is an immunotactoid glomerulopathy, the immunofluorescence examination shows that the organized deposits are monotypic. Glomerulopathy can either appear primitive or complicate a malignant hemopathy (which is in rule a chronic lymphoid leukemia or more rarely a B lymphoma). Most often, there is no evidence of circulating monoclonal immunoglobulin.
CRYOGLOBULINEMICS:
The renal involvement of cryoglobulinemia, which is the subject of a special chapter, will only give a very brief description of its main characteristics.
Cryoglobulins are immunoglobulins which, in vitro, precipitate in the cold. They can be classified in three categories: type I cryoglobulins which consist only of a monoclonal immunoglobulin; type II cryoglobulins which consist of a monoclonal immunoglobulin (most often IgM kappa) with anti-IgG activity and polyclonal IgG; type III cryoglobulins which consist of both polyclonal IgM with anti-IgG activity and polyclonal IgG.
In the case of type I cryoglobulins, the monoclonal immunoglobulin alone precipitates in the cold, whereas in the case of the type II and III cryoglobulins it is the IgMIgG complexes that precipitate in the cold. Cryoglobulin type I is demonstrated during lymphoplasmocytic proliferation, whether Waldenstrom disease, myeloma, or more rarely other lymphoid hemopathy. Mixed cryoglobulinemia can either complicate the progression of lymphoid hemopathy, infection (including hepatitis C virus), autoimmune disease or chronic liver disease, or appear as essential.
Cryoglobulin type II is the most common cause of kidney damage. This can be manifested by a nephritic syndrome, an abundant proteinuria with possibly nephrotic syndrome, or by isolated urinary abnormalities. It evolves willingly by pushes. It can be isolated or associated with other manifestations of the disease such as purpura, arthralgia, sensitivomotive neuropathy. The study of the renal biopsy typically reveals a particular membranoproliferative glomerulonephritis, on the one hand by the existence of an infiltration of the floculus by monocytes and T lymphocytes, and on the other hand by the presence of voluminous endomembranous deposits PAS (para-aminosalicylic acid) positive that can form thrombi in capillary lumens. Moreover, in about one-third of cases there are vasculitis lesions affecting the small and medium-sized arteries. In immunofluorescence, endomembranous deposits react with anti-IgM, anti-IgG, antikappa and / or antilambda antibodies. In electron microscopy, these deposits can be either amorphous deposits resembling immune complexes, or deposits having a microtubular structure.
GLOMERULONEPHRITES WITH IGM INTRACAPILLAR THROMBI:
This glomerulopathy is a rare condition that is seen exclusively in Waldenström disease. It should be emphasized in this regard that in patients with Waldenström disease, disorders of haemostasis are frequent and make it dangerous to perform a renal biopsy puncture.
In the six cases initially described by Morel-Maroger et al, this condition resulted in variable proteinuria, whereas renal function was normal or little altered.
In this same series, the study of renal biopsies showed PAS positive endomembranous deposits in a variable number of capillary loops. Sometimes these deposits could be large enough to occlude the capillary loops and form true thrombi. In the three cases where this was studied, these deposits were recognized by the anti-IgM sera.
The pathophysiology of this condition remains unclear, but it is possible that the deposition of monoclonal immunoglobulins in the capillary loops is favored by hyperviscosity. Along the glomerular capillaries, the formation of primitive urine by ultrafiltration of the plasma gradually increases the blood viscosity.
OTHER GLOMERULOPATHIES:
In dysglobulinemias, isolated observations of extracapillary glomerulonephritis and hypocomplementemic membranoproliferative glomerulonephritis without cryoglobulinemia have been reported.