1- Introduction / clinic:
– Immunological diseases related receptor blockade by the endplate acetylcholine receptors anti-Ac, resulted in excessive fatig reliability of striated muscles, improved by rest.
– Myasthenic phenomenon is a deficit in muscle strength whose essential character is to increase the opportunity of an effort. The fatigue increases during the day. This fatigue is corrected at rest.
 – An essential feature of this is its correction under the effect of anti-cholinesterase drugs. The cold improves.
– An essential feature of this is its correction under the effect of anti-cholinesterase drugs. The cold improves.
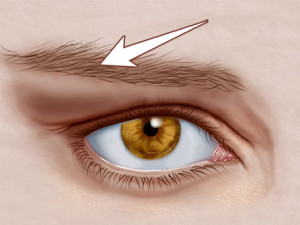
– Involvement of the eye-lid musculature is evocative. Ptosis (+ or diplopia) is one-sided to the top and can bilateralize thereafter remaining asymmetric habi-rently. It tends to increase later in the day.
– Achieving the bulbar muscle innervation sounds on phonation, mastication (with food) and swallowing (liquid discharge through the nose). The voice becomes intelligible nasonnée then.
– Achievement of limb muscles predominates on the proximal muscles (shoulder girdle). Myalgias are misleading.
– Involvement of respiratory muscles can lead to a rapid ventilatory decompensation sometimes inaugural.
– Negative signs: normal ROT; no sensory disorders; lack of muscle atrophy; lack of sphincter disorders.
– Signs of overdose in cholinesterase drugs (cholinergic crisis): abundant fasciculations, increased muscle weakness, nausea, vomiting, diarrhea, colic, tearing sweating, paleness, miosis, bradycardia.
– Transient neonatal myasthenia occurs in 10 to 25% of myasthenic mother of children. Early events for 2 to 3 weeks and then spontaneously regress. Hypotonia associated with the suction disorders, swallowing and breathing.
2- Associations:
– Thymus and gravis: thymic hyperplasia exists in 65% of cases and thymoma in 15% of cases. The thymectomies have a beneficial effect especially in cases of mere hyperplasia. Thymoma can be benign or malignant.
– Myasthenia and autoimmune diseases: associations are common. thyroid disease is found in 13% of cases.
An association with cancer is not exceptional.
3- Additional tests:
– EMG: presence of neuromuscular blockade after a repetitive low frequency stimulation (3Hz) with decrease in the amplitude of the muscular response (reduction potential of more than 10%).
NB: The most sensitive test is the single fiber EMG.
– Pharmacological test: test edrophonium (Tensilon) and prostigmine (cholinesterase inhibitors). This test temporarily regress symptoms. If it is negative does not exclude the diagnosis.
– Anti-receptor Ac acetylcholine: positive in more than 85% in case of generalized MG. Positive in 50% of ocular myasthenia. Free rate correlated with the clinical severity.
– Chest Scanner: search for thymoma or thymic hyperplasia.
– Testing the ice (less reliable) is transiently disappear ptosis
4- Classification:
– Group I: isolated eye shape
– Group II: little intense generalized form without respiratory muscle
– IIA: without reaching pharyngeal
– IIB: with involvement pharyngeal
– Group III: acute myasthenia gravis, severe, generalized with respiratory illness
– Group IV: myasthenia gravis, late
5- Respiratory Impairment two mechanisms:
– Acute myasthenic crisis: with acute motor deficit requiring emergency resuscitation. 4 signs: dyspnea, false-roads, ineffective cough, bronchial congestion.
– Cholinergic crisis: due to overload of cholinesterase inhibitors with respiratory paralysis and cholinergic signs of overdose include nausea, sweating, hy-persalivation, abdominal pain, diarrhea, miosis, bradycardia.
– The factors triggering acute myasthenic crisis: infections, stress, pregnancy, postpartum anesthesia.
6- Treatment:
A- Anticholinesterases:
prostigmine; Tensilon. Side effects are nicotinic (cramps, twitching); muscarinic (sweat, saliva and bronchial hypersecretion, abdominal pain and diarrhea, miosis, bradycardia). If overdose risk cholinergic respiratory crisis.
B- Etiological treatment:
– Thymectomy: risk of postoperative myasthenic thrust. Offered in the young and in generalized myasthenia.
– Corticosteroids: May initial transient worsening
– Immunosuppressive: offered in case of failure of thymectomy and corticosteroid therapy (azathioprine)
– Plasmapheresis: in acute forms (myasthenic crisis) before thymectomy
– Injectable polyvalent immunoglobulins: alternative to plasmapheresis
C- against Drugs suitable:
* Neuromuscular Blocking Agents
* Benzodiazepines (Hypnovel)
* General anesthetics (halothane)
* Muscle relaxants and antospasmodiques (dantrolene, baclofen)
* Antibiotics: aminoglycosides +++; colistin; polymyxin B; injectable tetracycline
* Drugs containing the salt of Mg 2+
* Quinine, quinidine, $ hydroquinidine
* D-penicillamine
7- Other causes of myasthenic syndrome:
– Drugs: especially, D-penicillamine can induce autoimmune myasthenia gravis. drugs that blocks the NMJ (curare …)
– Lambert-Eaton syndrome: paraneoplastic syndrome myasthiniforme; path is essentially with the lung small cell carcinoma. It is due to presynaptic blockage of neuromuscular transmission (insufficient release of acetylcholine). Ac positive anti-calcium channels in 50% of cases. Muscle deficit improves in the day or after an effort unlike myasthenia gravis. Respect oculomotor and facial motor. The ROT are often abolished.
vegetative disorders.
– Botulism: blocking the neuromuscular junction and cholinergic synapse cholinergic parasympathetic system.