Introduction:
Introduction:
Among the noninfectious and noninflammatory mechanical disorders, there is a group of pathologies leading to a table of pain of sacroiliac origin, including osteoarthritis, ankylosing hyperostosis, pain before and after delivery, condensing osteosis iliac, stress fractures of the athlete, which result in a mechanical disorder that can cause pain in the sacroiliac region.
These pathological entities, whose diagnosis is based mainly on radiological criteria, do not make it possible to explain on their own all the pain of sacroiliac origin encountered in current practice, especially in certain circumstances such as the practice of sport , the painful consequences of disc surgery, lumbosacral arthrodesis (32 to 61% of cases) or in the event of failure of zygapophysial and / or epidural infiltrations.
The concept of dysfunction, then evoked, poses various problems such as diagnostic identification, essentially clinical in the absence of a decisive contribution from radiology and the absence of a standardized protocol of care.
In view of the multiple origin of anatomical sites and potentially responsible processes, some authors have proposed the name “ sacro-iliac syndrome “ for the dysfunctional array.
Functional anatomy:
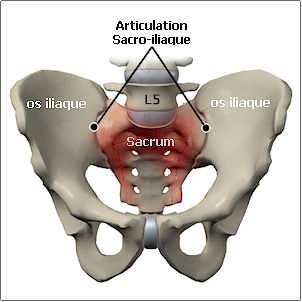
The anatomy of the sacroiliac joint is complex.
It is both an amphiarthrosis characterized by an interosseous ligament and a restricted mobility (2 ◦ in rotation, 2 mm in translation) and a diarthrosis, characterized by a capsule, a ligamentary apparatus and a synovial.
The joint is in the form of a boomerang with an average angle of 93 ◦ .
The ligament plane is composed of a ventral plane and a dorsal plane. The dorsal sacroiliac ligament comprises a superficial plane composed of four ilio-transverse-conjugate bundles, and a deep plane (interosseous ligament). The dorsal plane is completed by the iliolombar, sacrotuberous and sacro-epine ligaments.
Static stability depends on the strength of the ligaments (especially the interosseous ligament), the arrangement of the articular surfaces, the restricted mobility and the corner shape of the sacrum.
The section of the sacrotuberous and sacrospinous ligaments does not increase the articular mobility and thus plays no role in the dynamic stability during walking or jumping.
The joint capsule, which merges with the ligaments, may have defect and three free passages.
Innervation:
The innervation of sacro-iliacs is partly unknown.
The ventral surface of the sacroiliac joint depends, for some, on the ventral branches of the roots L4 and L5 (with other complementary branches: upper gluteal nerve and dorsal branches) and exclusively dorsal branches for others.
The dorsal side depends on the dorsal branches of the roots S1 to S2 for some, and roots L4 to S3 for others, which could explain the similarity of the painful arrays resulting from the sacroiliac joint and the lumbosacral hinge.
There is, moreover, a rich system of anastomosic arches between the primary dorsal branches.
Biomechanics:
The pathological mechanisms involved are numerous.
Hypermobility:
This is the mechanism most often mentioned. Instability can be increased by muscular factors such as decreased stabilizing activity of the thoracolumbar fascia (especially the oblique system). The hypermobility found can reach 8 ◦ in rotation (nutation and counter-nutation) on fresh corpses. This mechanism is evoked as a secondary phenomenon encountered during the practice of certain asymmetric sports activities (rowing, tennis), especially in women, during pregnancy (correlatively to the age of pregnancy), postpartum, motor neuron disease or as a result of lumbar arthrodesis.
However, hypermobility, as a pathological factor, is difficult to demonstrate in clinical studies.
Hypomobility:
Joint mobility decreases with age. Ligament structures contribute 10% to the restriction of this mobility.
The anteriorization of the load line:
This mechanism is found, in standing position during the wearing of load and sitting station in activities like rowing.
Muscle imbalance of the lower limbs:
This mechanism seems to be found in an inconstant way (rowers in sweep rowers), the asymmetry resulting in functional shortening of the lower limbs and an oblique pelvis.
Hip rotation asymmetry:
An imbalance of rotations in favor of external rotation on the side of the dysfunction can be found.
The anterior iliac rotation:
It is a mechanism often mentioned in osteopathy.
The alteration of muscular recruitment:
The activation delay of the stabilizing muscles of the sacroiliac (gluteus maximus, internal oblique) during the phase of support to walking has also been advanced. The alteration of the function of the gluteus maximus would be compensated by the activity of the femoral biceps.
The relaxation of the long posterior sacro-iliac ligament:
The relaxation of the long posterior sacroiliac ligament by the tensioning of the gluteus maximus or the anterior iliac rotation in counter-nutation.
Structural asymmetry:
Various risk factors relate to structural asymmetry such as scoliosis, inferior length of limbs, psoas stiffness. . .
Anatomoclinic relationships:
They are a source of controversy.
The intra-articular lesions of arthritic origin, the best described, are most often asymptomatic.
Extra-articular lesions are cited as potentially responsible: the zone exposed to the strongest stresses from a mechanical point of view seems to be the part adjacent to the median part of the joint. This area includes the interosseous axial ligament and the superficial and middle plane of the posterior sacroiliac ligament. The long posterior sacroiliac ligament which is contiguous to the second and third medial nerve clusters emerging from the posterior sacral orifices is implicated in the origin of the pain by some authors, especially in peripartum.
Functional Symptomatology:
The beginning may be insidious as brutal.
The triggering factors can be traumatic (fall on the buttocks, car accident: ipsilateral foot blocked on the pedal, reception of a jump, side impact on the pelvis) but most often microtraumatic (58%). One can emphasize the spontaneous character frequently found (35%).
The pain caused in the healthy subject or felt in the affected subject is located between L4 and the buttock. The picture thus associates low back pain and sacralgia. Irradiation is possible; among them, inguinalgia, trochanteralgia, pains in the ischium, pain in the posterior aspect of the thigh, most often sparing the popliteal cavity, and in a disputed manner of the pseudosciatalgia with irradiation under the knee. However, some may be frequent (22.5%). If we consider the causes of sciatica other than the discoradicular conflict, sacroiliac pathology is found in less than 1% of cases.
At the interrogation, it is usually illusory to distinguish the sacral region from the low back pain, whether in the context of initial pain or during evolution.
Van der Wurff et al., By comparing responding and non-responding subjects before and after intra-articular test block, do not find any difference in the painful territories. The only localization correlated with the test block is inguinal pain.
It is more informative to have the finger pointed at the region responsible for the acme of pain, situated slightly below and within the posterior iliac spine.
Lumbalgia secondary to sacral pain can appear in a variable time between a few days and a few weeks.
The actions of everyday life responsible for the triggering or exacerbation of pain of sacroiliac origin are non-specific in relation to other causes of low back pain (seated / standing transfer, walking), except perhaps the seating. In summary, nothing in the symptomatology of lumbosacralgia distinguishes patients with sacroiliac syndrome from those suffering from the lumbosacral hinge.
The comparison between two groups of subjects according to the response to the anesthetic test block or to the combination of the anesthetic test block and the infiltration of corticoids does not make it possible to demonstrate an activity that specifically triggers sacroiliac pain.
The resulting functional impotence is variable. Most of the time, walking is intermittently interfered with without limitation of the walking perimeter. A lameness is rarely encountered.
Bilateral forms are not uncommon (30%), which is consistent with the figures found in the osteopathic literature (20%).
In an obstetric context, the onset is often abrupt with pain in the seated position, in the immediate postpartum period gradually exacerbating over several days.
Epidemiology:
Low back pain is an extremely common symptom in the general population. Seven to 10% of the low back pain population persist for more than six months.
The prevalence of pain of sacroiliac origin among the general population is not known.
The selective criteria used to diagnose pain of sacroiliac origin show positive signs such as the higher level and the centralization of the low back pain associated with the sacralgia, the sacralgia area compatible with the typology known from the cartographies carried out by the provocation tests in healthy subjects, age, intensity and sometimes negative criteria: lumbar MRI or CT, zygapophysial blocks, epidural infiltration, facet infiltration, discography, fibromyalgia. There is no consensus on the choice of these criteria.
The majority validation procedure is the intra-articular anesthetic test block sometimes combined with the arthrographic distension pain reproduction test, which does not seem to give any associated value. In order to improve the diagnostic value of this test block, some authors propose a second block of confirmation in the case of a positive one because there is a high rate of false positives (20 to 22%).
The prevalence studied varies from 10 to 30.
Maigne et al. note that the maximum rate of 30% joins the figures encountered in the osteopathic literature.
The figures vary according to the population, the selection criteria of the patients eligible for the test block.
The observed prevalence can be increased (32%) in certain pathological circumstances such as lumbosacral arthrodesis.
There is no a priori predominant side, neither in the distribution of the painful localizations nor in that of the radiological lesions.
The sports most often cited as responsible for pain are: rowing (prevalence in the elite: 54.1%), cross-country skiing (especially in asymmetric technique) and ice hockey. This list differs from the one grouping sports where fatigue fractures are observed: dance, gymnastics, tennis, sprint, throwing.
Physical examination:
Positive tests:
There are around 30 tests.
Two types of tests are described: tests for mobility dysfunction (standing and sitting tests) and pain provocation tests.The challenge tests include stress tests and palpation tests. The provocation tests are considered positive only in the event of the onset of lateral pain, thus excluding a central pain that would favor a lumbosacral origin.
Dysfunction test of standing or sitting mobility:
Bending test: the thumbs placed under the posterior iliac spine symmetrically show an asymmetry of level at the end of anterior flexion of the trunk with a super-elevation of the thumb situated on the side of the sacro-iliac hypomobile.
The palpation tests:
In addition to the contribution to the diagnosis of pain of sacroiliac origin, the palpation tests allow the localization of the responsible anatomical site: the long dorsal ligament of the posterior iliac spine to the fourth sacral part, the sacro- tubal, joint space.
However, palpation on an obese or asymmetric subject may prove difficult.
Stress tests:
Stress tests can be classified according to the mechanism involved (distraction ++, compression, torsion), the addition of resistant contractions or the type of lever arm used.
Stress tests on the lower limbs The Patrick (or Fabre) test. The patient is in supine position with the foot resting on the contralateral limb at the knee positioning the hip in flexion, abduction and discrete external rotation. The examiner emphasizes this movement by pressing on the knee to cause tension of the anterior sacroiliac ligaments and the reproduction of lumbosacralgia.
The test of Yeoman (or Mennel). The patient is in procubitus, the examiner drives the hip in extension with rotations of the hip and a flexion of the knee variable according to the authors. The support is varied according to the authors on the posterior superior iliac spine (ipsi or contralateral), sacrum or sacral sulcus.
Thigh thrust test (or Posterior shear test). The patient is supine, with flexed hip around 90 </s>. The examiner, placed on the non-pathological side, presses with the weight of his trunk (force?) The femur of the patient, associating an adduction and causes shear at the level of the sacroiliac and a stress on the sacroiliac ligaments hindquarters.
The Gaenslen test. Sick in supine position at the edge or at the end of the table, the examiner positions the hip on the pathological side in forced extension out of the table while the other hip fixes the pelvis through forced flexion. The test can be meaningful during the reverse maneuver with hip flexion on the pathological side.
The sacroiliac aggravation test. The examiner placed on the suspect side exerts a posterior pressure on the iliac side of the sacroiliac by a vertical force on the hip, with the knee of the patient positioned at 90 </s>.
Active elevation of the tense leg. This test evaluates joint stability. It consists of actively lifting one leg, one after the other, to a height of 20 cm from the position of rest in supine position. Lateral compression of the pelvis decreases the pain syndrome.
The sign of Lasègue. The passive elevation of the lower limb of the pathological side, ankle in the position of plantar flexion, causes the ipsilateral fessalgia from 60 ◦ up to 90 ◦ , without increase of the pain by dorsiflexion of the ankle (Bragard test) which makes it possible to eliminate pain of hard-merian or radicular origin.
The Lasègue maneuver would also cause contralateral pain, depending on the type of dysfunction. The practice of bilateral Lasègue would make it possible to raise the sensitivity of the test and to reduce the angle of appearance of the pain.
The tests of contractions resisted. Adductors, lateral rotators, abductors (Mac-Nab test).
Whatever the muscles involved, the resisted contraction is always performed bilaterally.
With direct constraints on the basin:
Compression tests. Sick in lateral decubitus, the examiner exerts a vertical pressure on the iliac wing on the pathological side.
Compression tests of the sacrum in procubitus.
Sacral thrust test and its variant: the cranial shear test:
• the sacral thrust test: the examiner exercises a vertical thrust with both hands superimposed on the center of the sacrum and then completed by a lateral thrust on the hemisacrum;
• the cranial shear test: the thrust is carried out in the cranial direction. The examiner, located at the end of the table, can also fix the lower limbs of the patient by positioning them between his own lower limbs.
Distracted testing. The patient is in supine position (Gapping test, Squish test): a bilateral thrust downwards and outwards on the anterior superior iliac spines stresses the anterior sacroiliac ligaments and compresses the articular structures.
Negative tests:
Negative tests include two categories:
• tests for sciatica;
• tests for hip disease.
The Contributory Value of Clinical Trials:
Few tests, of all those described, have been validated:
• validated tests for reproducibility: Patrick, Yeoman, thigh thrust test, Gaenslen, cranial shear test, compression test, sacro-iliac aggravation, Distraction;
• Validated tests for diagnostic value: Patrick, Yeoman, thigh thrust test, sacro-iliac aggravation, Gaenslen, sacral thrust test.
Reproducibility:
Reproducibility depends on the experience of the examiner, although this point is discussed, and the force involved.
For the majority of authors, only pain provocation tests show inter-observer reliability, as opposed to mobility tests. Of these, five have good (moderate to high) reproducibility with a kappa coefficient greater than 0.6: thigh thrust test, Gaenslen test, cranial shear test, compression test, distraction test. The thigh thrust test is, for Laslett and Maynard, the only one with very good reproducibility (kappa> 0.80). The Patrick test and the sacral thrust test have contradictory results.
For Fransoo and Legan, only seven out of 14 tests were retained for their reproducibility: palpation of the posterior sacroiliac ligament, elevation of the stretched leg, thigh thrust test, Patrick’s test, standing flexion, articular clearance test and compression test. It recommends the combination of tests to ensure moderate reliability.
Finally, other authors point out the insufficient reproducibility of each test taken in isolation while advising the practice of three combined tests.
The tests which appear to be insufficiently reproducible and which can be eliminated are: the Gillet test, the sitting flexure test and the sacral thrust test.
For Vleeming and De Vries, the active elevation test of the tense leg is reproducible in women in peripartum.
The diagnostic value of the tests:
It is difficult to distinguish pain of sacroiliac origin from involvement of the lumbosacral hinge in isolated cases. If lumbosacral pain is frequently accompanied by low irradiation, pain of sacroiliac origin is accompanied less frequently by high irradiations, with the possible exception of the parturiante.
Apart from the pain entangled by an irradiation mechanism, the problem arises of a pathology associating pain of mixed origin; their frequency is estimated at 35%.
The distinction between irradiated pain and associated pain is not always made in studies seeking sacroiliac origin.The only element that is constantly retained is the search for predominant pain of sacroiliac origin, characterized by the analgesic response rate after the test block.
The high incidence of false positives in abnormal mobility clinical trials in asymptomatic patients (20%) should be noted.
Various series highlight the inadequacy, or even lack of diagnostic value, of each of the clinical tests used in isolation in the role of the sacroiliac region by comparing the responder and non-responder groups to following an intra-articular anesthetic test block.
In view of the lack of diagnostic value of each of these clinical trials, several authors have recently stressed the value of combining the tests, despite the negative conclusions already expressed in 1996 by Dreyfuss et al. and Slipman et al. in 1998.
Laslett et al. are considered to be the likely sacroiliac origin of pain, with three positive tests at least among the six most contributing tests (distraction test, thigh thrust test, compression test, right and left test, sacral thrust test). The specificity and the sensitivity then obtained are respectively 0.87 and 0.91.
This attitude is found in Broadhurst and Bond which, in a double-blind study, uses the Patrick test, the thigh trust test and the abducted abduction test with a sensitivity ranging from 77 to 87% and a specificity of 100% in retaining as a threshold of positivity the reduction of at least 70% of the pain.
A recent review concludes that it is useful to combine tests with a sensitivity and specificity of more than 60%. There are five tests: distraction test, compression test, thigh thrust test, sacral thrust and aborted abduction test.
In specific pathological situations, certain tests are appropriate such as palpation of the long dorsal ligament (sensitivity of 76%), elevation of the tense leg, and the sacroiliac aggravation test for postpartum preetural pain.
Physical signs retained in the studies for the sacro-iliac origin of pain:
Attitudes are diverse:
• a single test is selected as necessary from a pre-selected list: the thigh bending test, the Gaenslen test, the Patrick test;
• a single positive test on three provocation tests including: Gaenslen, Patrick and Newton;
• three tests must be positive on four achieved: Gaenslen, Yeoman, Patrick, Gillet;
• three positive tests, two of which were pre-selected (Patrick’s test and palpatory test);
• three positive tests out of six performed: Gaenslen, Yeoman, Patrick, compression test, thigh thrust test, contraction resisted abduction.
To summarize, to study the interest of clinical assessment, the following simple notions are used:
• In simple cases where a sacroiliac syndrome is not accompanied by associated lumbosacral pathologies, the pain is located mainly in the sacral region and is accompanied by a normal spinal examination: it is lumbosacralgia without spinal physical examination;
• in the forms with associated spinal syndrome, only the combination of at least three positive tests is contributory.
Paraclinic Review:
Classically the dysfunction has no or few radiological abnormalities.
Standard radiology:
Radio-anatomy is difficult to explore by conventional radiology.
The value of the standard radiograph (face, profile, oblique) is classically little or not informative within the framework of the dysfunction table. It does not, in the case of negative exploration, eliminate a diagnosis of dysfunction.
Conventional radiology has a very low sensitivity and detects little change in the suspicions of dysfunction, including in the sportsman.
Conversely, 24.5% of asymptomatic patients over the age of 50 have degenerative signs.
Arthrography:
The profile view and the oblique allow the visualization of a ventral recess. The anteroposterior view visualizes a small lower recess. The line spacing is indicated by a line viewed on the ipsilateral oblique.
The anomaly statistically associated with a positive anesthetic block is the ventral capsular tear (20%). No other anomaly appears to have any significance (diverticulum). Only 15% of patients with normal arthrograms respond favorably to the anesthetic test block.
In total, the arthrography seems really contributory only to ensure the quality of the test block used at the same time.
Computed tomography (CT):
Its positive or negative diagnostic value for sacroiliac dysfunction is low. The sensitivity varies from 12.9 to 57.5%.
Thus, for Elgafy and Semaan, CT showed positive signs only in 57.5% of patients suspected of sacroiliac pain with negative lumbar MRI, palpatory examination and intra-articular test block ( 31% in the control group). The specificity is 69%.
Anomalies are rare among patients under 30 years of age.
The most frequent signs in the symptomatic group are osteophytes (31%) and subchondral sclerosis (greater than 5 mm on the iliac side [37%] and greater than 3 mm on the sacral side [12,6%]) .
Rare signs are articular pinching of less than 2 mm, preferentially located on the iliac side (normal thickness of iliac cartilage: 1 to 2 mm and sacral: 4 mm) in 6% of cases and geodes in 3.4%.
The signs that are always absent are localized erosions and ankylosis.
However, CT allows to determine the angulation of the line spacing in the axial plane in order to guide possible injection under fluoroscopy and the possible existence (13 to 16% of the examinations) of an accessory joint between the medial slope of the axial plane posterior superior iliac spine and a rudimentary articular surface located just laterally to the second sacral hole.
The MRI:
The contribution of MRI in the study of dysfunction is not known. MRI can be used for guiding the infiltration or block.
in inflammatory pathologies. The interpretation of the physiopathological origin of pain can not rule out the hypothesis of the presence of moderate inflammation without an increase in osteoblastic activity.
Conversely, scintigraphy provides a good diagnostic contribution for osteoporotic fractures after minor trauma and fatigue fractures.
Injection challenge tests:
No method of intra-articular injection can be performed with an exclusively clinical guide, under penalty of a considerable failure rate.
The tests are carried out by triggering the pain during the intra-articular injection of 1 ml of contrast agent, sometimes associated with hypertonic saline serum (0.5 ml to 10%). The response is ranked on a scale of four grades: “ unusual pain “ , “ no pain “ , “ similar pain “ and “ identical pain “ .
The test is considered positive when the pain is the same as the spontaneous pain. The challenge test is used by some authors as a screening test to then propose the anesthetic test block.
There seems to be a negative correlation between the challenge test and the favorable response to the anesthetic block.
Thus, the absence of exact reproduction of the pain is a prognostic criterion of the absence of response to the test block. Conversely, the patient’s perceived pain-free reproduction does not appear to be a favorable prognostic factor for the test block.
Murakami and Tanaka found a positive test in 92% of the intraarticular injection group and a positive test in 100% of the periarticular injection group, suggesting a large number of false positives .
The anesthetic test blocks:
The sites :
Several authors insist on two notions:
• the risk of neglecting extra-articular sources of pain, a notion already mentioned in 1996 by Maigne et al. during the intra-articular injection, highlighted in 2002 and confirmed recently in 2008;
• the risk of underestimating or overestimating the intra-articular origin of pain, especially because of the importance of extra-articular leakage, which can reach 61%.
Products:
The products are:
• bupivacaine 0.5% which allows a prolonged effect for a minimum of two hours;
• 2% lignocaine for five to ten minutes (0.5 to 2 ml) used as a selective test prior to the bupivacaine confirmatory test.
The rate of false positives (17%) is lower than that of facet test blocks.
Laslett et al. recommend to limit the total volume injected to 1.5 ml (0.5 ml of contrast agent and 1 ml of anesthetic) to limit the risk of leakage.
The techniques:
Two techniques are possible:
• Intra-articular: the technique by lower route, described by Fortin et al., Is well standardized. The isolated block of each of the dorsal branches does not allow the intra-articular block to be replaced;
• periarticular: the procedure comprises different variants which have been described.
The radius is cranially oriented to clear the line spacing. The localization of the injection is the deep posterior ligamentous plane (interosseous ligament). The place of injection is on the projection of the line spacing at different height levels in four different zones. The injected product remains localized in each of the selected zones. For Borowski et al., The test block is completed by injection of the lateral portions of the dorsal branches from S1 to S3.
The interpretation:
Some authors recommend, after an intraarticular block, to exclude patients with extra-articular extravasion on the arthrogram.
Interpretation is done in two ways:
• by pre- and post-test comparison of the painful nature of activities of everyday life or triggering movements or postures. The threshold usually considered significant is a 75% or greater reduction in pain on an analog visual scale for 15 to 45 minutes with lidocaine injection and more than two hours with bupivacaine injection. A lower threshold entails a risk of overestimating the diagnosis, especially if a base threshold is chosen: 62%, 50%. This 75% rate makes it possible to improve patient selection and improve therapeutic studies. Exceptionally, a higher threshold is chosen: 80% or even 90%;
• by pre- and post-test comparison of a catalog of activities of daily living containing six items from the following seven: getting up from a chair, stopping in a semi-upright position and then rising, lifting a load heavy, walking, turning from one side to the other in the lying position. Each item is scored on a five-grade scale. Pain assessment is done by establishing a cumulative score.
The results:
Intra-articular injection:
Different studies have demonstrated the possibility of temporarily reducing suspected sacroiliac pains in 18 to 57% of cases. For Schwarzer et al., The only painful localization specifically responding to the test block is inguinal pain.
The diagnostic value of the intraarticular anesthetic block is controversial:
• for some, the test block is a gold procedure whose value allows diagnostic assertion provided optimization of the conditions of use (arthrography and provocation test);
• for others, more recently, if the test is considered to be the golden procedure, it may lead to an over-use of the procedure and an overstatement of the diagnosis of sacroiliac joint syndrome.
Criticism from detractors concerns the lack of reproducibility (60%) and specificity due to diffusion of the product out of the joint in 61% of the intraarticular tests.
In the event of leakage, the product may concern the roots L5 and S1 and the lumbosacral plexus.
This explains some of the discrepancies between the provocation tests (during arthrography) and the anesthetic block.
Peri-articular injection:
Murakami and Tanaka, in an uncontrolled study, noted a 100% positive response rate. In 56% of cases, the site considered to be responsible for the pain was in the middle of the joint, 24% in the upper third, 18% in the lower zone and 3% in the other , in the area overlying the joint.
For the author, these results emphasize the role of peri-articular structures as a generator of pain and mainly in the interosseous ligament.
Combined injection (intra- and periarticular) Combined injection (intra- and periarticular): the response rate is 62.5%.The anesthetic test block can be coupled at the same time by a therapeutic glucocorticoid test for some authors. The block is then considered positive if the improvement is observed for more than one week. It would increase sensitivity (60%). The products used are methylprednisolone (40 to 80 mg) or methylprednisolone-acetate (60 mg).
Differential diagnosis of dysfunction:
Sacroiliac arthrosis:
The overall radiological prevalence is 78% in a population of 20 to 75 years.
Natural history reveals that degenerative alterations begin in their thirties and progress with the years.
The risk factors mentioned are inferior length of the lower limbs, postural abnormalities (hyperlordosis) and obesity.Arguments favor the existence of sacrococcygeal malformations with extension to the sacro-iliac.
The lesions found are in order of frequency: fibrillation, surface irregularities, cracks, cartilage necrosis, osteophyte formation and fibro-osteocartilaginous replacement of the cartilaginous space.
Ankyloses are rare. Erosions are infrequent and superficial.
Radiological findings predominate on the iliac side at the level of the fibrocartilaginous area. The elective seat of the overload lesions is in the area of maximum stresses on the anterior portion of the middle segment. Lesions are symmetrical except in hinge anomalies or post-traumatic forms.
In the athletes are associated lesions of the sacro-iliac and the pubis. The lower third of the joint is almost always preserved in mechanical affections.
The typology of the lesions varies according to sex: osteophytosis, more common in humans, is located in the anterior superior part whereas in women the osteophytes are rather anterior inferior. Osteophytes are early in sports. The incidence of lesions is higher among black subjects.
Radioclinic correlations are poorly understood.
Inflammatory iliac osteosis:
The condensation, of triangular form, is located at the level of the iliac bone of the middle third of the joint, without alteration of the interline or the subchondral bone.
It is found almost exclusively in women (95%) and mainly after one or more pregnancies.
Frequent (up to 2.5%) in the middle-aged adult population (35 years), it is mostly unilateral.
It is for most authors frequently asymptomatic with however exceptions. The difficulty is, in some cases, to differentiate it from a sacroiliitis.
The condensation may disappear, in whole or in part, depending on the duration of evolution.
Ankylosing Hyperostosis:
The intra-articular involvement of the sacroiliac in this condition is rare since pure fusion without osteophyte is estimated between 0 and 4%. In case of ankylosis by osteophyte, the fusion is found in 24% of the cases and the difficult distinction with the rheumatic pelvispondy. Ankylosis is then peripheral, resulting from bone bridges secondary to chronic enthesopathies that predominate on the anterior plane. Ossifications are the predominant elemental lesions with rare associated lesions, such as erosions or hyperostosis. These bone proliferations are well defined by CT scans.
The anatomoclinic relationship is difficult to define. It seems that the asymptomatic forms are very frequent since in 28 radiological observations no painful syndrome was found.
Sacroiliac Pain and Pregnancy:
The radiological signs present are localized to the pubic symphysis in the first half of pregnancy and precede the appearance of hypermobility of the sacroiliac observed at the end of pregnancy, reaching one and a half times the initial mobility. Pelvic involvement affects 50% of the parturiantes. Morbidity, in addition to the age of pregnancy, depends on the age of the parturiante. Hyperlaxity is found in 77% of pelvic pain cases. Ligament relaxation regresses in three to five months after childbirth.
Lumbosacralgia is frequent during pregnancy (50% of women) and is multifactorial in origin.
Their characteristics are specific because of their brevity and regressiveness in most cases after childbirth, except in 9.1%, where the pain persists between 0.5 and 12 months after a difficult delivery.
The importance of the place of pain of sacroiliac origin in the origin of these lumbosacralgias is not well known.
Sacro-iliac and piriformis:
A pathology of the sacro-iliac may result, through its anatomical relations, in contracture of piriformis and secondary sciatica. This mechanism is evoked in postpartum sciatica.
Athletic arthropathy:
The microtraumatic pathology of the athlete is due to overuse, secondary to a modification or a resumption of training.
Fracture of sacred fatigue and sport:
Sacral fatigue fractures are rare and the published series each report only a few cases. They are mainly related to the long distance race (more than 80 km / week) but not always (tennis, sprint, throw). There is often an intensification or modification of the conditions of practice (change of shoe or surface).
The clinical presentation, which is not specific, is a lumbosal or lumbosalgic chart, which systematically evokes a disc condition prior to subsequent diagnostic revision.
Standard radiography is most often defeated due to the absence of callus production. CT and MRI can be contributory (50% of cases for each exam). The MRI shows a hyposignal in T1 and a hypersignal in T2.
The trajectory of the fracture in the background runner is stereotyped.
It starts from the upper edge of the wing and proceeds towards the first sacral hole parallel to the sacroiliac line.
Sometimes, only the scintigraphy allows the diagnosis.
The anomalies can be seen on the posterior views but especially on the obliques. The locations of the stress fracture are both anterior and posterior.
The long-term outcome of the fatigue fracture, notably the risk of degenerative arthropathy is not well known.
However, it is difficult to confirm a good radioclinic correlation since the existence of a fissure of sacroiliac fatigue, with scintigraphic evidence, could be identified in the absence of functional and physical sign.
The treatment is the rest, with stopping of the stomach, for four to six weeks.
Treatments for dysfunction:
Manual therapy and self-correction:
The principle of action would be to correct the “ osteopathic lesion “ most often in anterior rotation of the ileum (especially in the peripartum), but also, sometimes, in posterior rotation. The dysfunction can be bilateral.
The Lasègue maneuver would determine the type of dysfunction: the pain of an anterior dysfunction is increased by a sign of a contralateral positive Lasègue and the pain of a posterior dysfunction is aggravated by an ipsilateral maneuver.
Dysfunction may also cause pseudorabrasion of the ipsilateral lower limb to the posterior ilii.
The correction of a prior dysfunction occurs in several ways. In case of bilateral dysfunction, the correction will be made first on the less painful side.
A complementary autocorrelation program may be necessary by mobilizing the hemibasin by flexing the hip in different postures or by hyperextension of the pelvifemoral complex. These exercises should be performed symmetrically on 15 sets of two to three replicates per day, for three or four days, then gradually for one week.
Other measures to improve stability in addition to corrective measures include increased medial rotation amplitude, increased gluteus maximus, pelvic girdle and compensation for lower limb inequality in persistent cases after manual treatment.
The beneficial role of rehabilitation with stabilization exercises has helped women reduce post-partum pain in a controlled study.
Infiltrations:
The beneficial role of infiltrations is well known in spondylarthropathies and more discussed in dysfunctions.
Intra-articular:
The cavity is narrow (2-5 ml) with partitions.
The needle must penetrate 1 cm inside the joint so that the product is in intra-articular. Intra-articular injection without arthrographic control should not be used because of its low success rate (22%).
An epidural passage is possible (24%) through the sacral hole. CT may be necessary in case of obesity or in case of special obliquity, or of obstacle in the line spacing in the axial plane.
The insertion point is located midway between the projection of the posterior iliac spine and the median line and slightly below the caudal part of the joint (1-3 cm) because the lower line is the most accessible. The upper track is more difficult to access and is a source of side effects. The angulation in the transverse plane is oriented laterally by 45 </s>.
The needle is 9 cm and 22 or 25 gauges.
Periarticular:
The site is chosen according to the localization of the pain, which is, according to the experiments, 3-4 cm below the posterior iliac spine and 6-7 cm from the midline of the sacrum.
Bone contact should be sought.
The results:
The assessment is made at one month, two months or three months.
Intra-articular:
In the sacroiliitis, the positive result on pyalgia is ten out of 12 positive cases with an efficacy of an average duration of 9.6 months.
In dysfunctions, a positive response rate is reported that varies greatly from one study to another. The results are discordant and vary from 12.5% to three months after rigorous selection (in particular cases of failure of spinal infiltrations), 33% to more than six months after selection by anesthetic test block (but threshold selected at 50 %!) and up to 90% at two months without block selection.
Infiltrations were proposed during pregnancy with a benefit of three points on the visual analog scale from the 14th week.
Slipman and Lipetz found in a retrospective study, without excluding false positives, an improvement in the visual analog score and the Oswestry score from 33.3 to 44.6.
Periarticular:
In the dysfunctions, Luukkainen et al. emphasize the value of peri-articular injections. The short-term assessment (one month) showed an average improvement on the visual analog scale of 40% in a randomized study (13% in the placebo group). The effect does not appear to be related to the systemic passage.
Combined injection:
The three-month response rate was 31.25% following an injection for different sites: intraarticular, periarticular, including the ligament plane and lateral branches of S1 to S3 in an uncontrolled retrospective study. The authors’ conclusions are in favor of the superior effect of this type of injection compared to the isolated intraarticular injection pending a methodologically acceptable confirmation.
The viscosupplementation:
The favorable effect of viscosupplementation was observed in the initial study with three injections (Hylan GF 20) at two weeks intervals with a benefit of 40 to 65% at a 12-16 week follow-up. These results were confirmed with an average pain reduction rate of 72% at one month of confirmed follow-up at six months.
Thermocoagulation of lateral branches of dorsal sacral branches by radiofrequency
A number of authors reported results of limited value over time (36% very good results) at six months. A recent controlled study finds an improvement equal to or greater than 50% in 57% of cases at six months of recoil by cooling the canula and identifying the origin of the sensitive branch innervating the posterior surface of the joint. However, the result was one year loss (14% of favorable cases) in relation to nerve regeneration occurring between six months and one year.
The initial failure rate can be explained by the incomplete innervation of the sacroiliac joint by the dorsal branches.
Prolotherapy:
Prolotherapy is an unusual treatment method.
The rate of responding patients, reported following injection of a phenol solution in the ligament plane, is 61% at one year of follow-up in a single study.
The prolotherapy is then carried out only in case of failure of infiltrations. The average percentage of pain improvement in responders was 82%.
Surgery:
A series reports the interest of surgical debridement by micro-invasive surgery. Sixty-one percent of patients reported a pain intensity reduction of 50-100% on the short-term analog visual scale and 53% maintained a better than 75% improvement after two years.
The reported results of the arthrodesis by Buchowski et al. are in favor of a rate of between 50 and 70% of good and very good results. The most commonly used procedure is the Smith-Pederson technique with a possible instrumentation associated with no postoperative immobilation and a discharge for three months. Other techniques are possible by the anterior route or else percutaneously.
Dysfunction is the leading cause leading to arthrodesis for Buchowski et al. with 65% of total indications. The rate of non-fusion is 15%, all etiology confused.
Conclusion:
Dysfunction is a component of the sacroiliac syndrome.
This clinical entity is still being dismembered thanks to new etiological, clinical and diagnostic concepts.
Conflict of interest:
The authors did not transmit a conflict of interest.