Introduction:
Introduction:
Anatomical reconstructions of the anterior cruciate ligament (LCA) using autografts have been used for more than 15 years to restore pivotal sports while preserving meniscal capital.Despite the reliability of the procedures performed and the precautions usually observed, a sprain recurrence is always possible. The number of LCA ligamentoplasties performed annually in France is estimated at 34,000 per year.
Reconstruction failures and incomplete results increase with hindsight and concern, according to the series, 5 to 25% of the cases. Salmon et al., In which 67 patients, 85% of whom were seen at 13 years of follow-up, had 13% rupture and 21% low-grade jump with the bone-tendon-bone transplant. The diagnosis of rupture of the LCA is easily posed when the traumatized knee has not already been operated. How should laxity be analyzed on a knee whose LCA has already been reconstructed? A moderate residual anterior laxity is frequently observed after the central pivot has been repaired. Insulated intra-articular plastisas control the anterior drawer well, but may occasionally leave a low jump that is compatible with a good functional result. Is the transplant really broken or distended? What was the ligament state of the knee just before the new trauma? Is it a traumatic sprain or an early anatomical failure?
How to assess the laxity of an already operated knee?
The measurement of the anterior laxity of the injured knee and of the healthy knee makes it possible to express a differential value in millimeters.
Arthrometers (Medmetric ® KT 1000 TM ):
The values obtained in the maximum manual traction mode are the most discriminative. The value chosen corresponds to the average resulting from three successive measurements obtained by the same examiner.
Dynamic radiographs:
Dynamic X-ray photographs of the profile make it possible to evaluate the translation by measuring the translatory differential advance of the internal plate.
Positional Drawer:
Positional dynamic radiographs such as the monopodal profile support use elemental body weight constraints coupled with muscle contractions.
The results are random and influenced by the constitutional tibial slope, weight and degree of contraction of the ischiojambic muscles.
Lachman active radiology:
Active contraction of the quadriceps against a weight of 7 kg applied to the distal end of the tibial skeleton results in anterior subluxation of the tibia.
Lachman radiological passive:
The measurements of the passive radiological drawer according to the method of Lerat et al. use a weight of 9 kg which is applied on the thigh above the kneecap on a knee bent at 20 </s>.
This measurement technique has the advantage of leaving the knee free to rotate. Unlike Telos ® , the knee is not constrained by the translatory thrust whose point of application is located at a distance from the tibial plates.
The static measurement of the differential advance of the medial and lateral compartments at 30 ◦ of flexion makes it possible to demonstrate the rotation of the knee coupled to the anterior drawer under the effect of a simple translatory stress.
The camera with snapshots (Telos ®):
Is it necessary to use a thrust of 150, 200 or 250 N, which is much higher than that recommended by the IKDC plug (137 N)? Staubli and Jakob established a cut-off value of the ACL at 3 mm with a translational force of only 89 N. Bach et al. had obtained with the KT 1000 TM the same threshold value in maximum traction mode. The statistical analysis of Bercovy and Weber has shown imprecise measurements below a threshold value of 180 N. For the latter author, a differential greater than or equal to 4 mm made it possible, using a thrust at 250 N, to assert the rupture of the LCA with an accuracy of 98.5%. Although causing some discomfort, a translational force of 250 N would minimize the risk of false negative by neutralizing parasitic muscle contractions. The values obtained with 250 N of thrust would be somewhat higher than those acquired at 150 N. In the case of an already operated knee, account should also be taken of the laximetric data obtained from the last examination performed.
Only a ligament examination recorded and dated by the same examiner can then truly serve as a comparison.
It is preferable that the same experienced examiner evaluates the ligament laxity each time to avoid interobserver errors. The rubric of the ligament examination from IKDC should be used to compare the scores. For a knee whose ACL has already been reconstructed, the breaking threshold value is 5 mm.
Is the graft broken or distended?
The ligamentous structures possess viscoelastic behavior. The elasticity phase is characterized by a reversible deformation under the effect of a short constraint. A continuous graft may be the seat of an irreversible plastic distension equivalent to a collagenic relaxation. For Rollier et al., The transplant is actually more relaxed than actually broken (54% versus 30%) in the event of failure. The pathological laxity characterizing the distension is defined by a downgrading of one or two levels in the IKDC section of the ligament examination group. Grade I surges are still good results and should be interpreted in comparison with data from the last clinical examination.
After a certain threshold of stress, the rupture becomes inevitable with solution of continuity to the MRI. When a transplant is partially broken, the continuous fibers have undergone a plastic elongation explaining the residual laxity.
Special case of mixed intra- and extra-articular plastis:
An important residual laxity without rotational jump can be observed with intra- and extra-articular plasties.
The lateral tenodesis which limits the advance of the lateral compartment can still fully play its role of anti-splintering despite the distension of the central pivot. The anterior laxity is then recognized as arthrogenous with the appearance of secondary meniscal lesions. Fautil in this case reconstruct the central pivot again to preserve the meniscal capital?In contrast, an isolated intraarticular plasty can satisfactorily control the anterior drawer and inadequately neutralize the jump.
Is it then necessary in these cases to reconstruct the single posterolateral beam or to perform an additional lateral tenode- sis to better lock the internal rotation? Depending on the anatomical level of incompetence, reconstructions with two beams are also likely to modify the clinical examination of an already operated knee.
What are the factors behind the failure?
The sprain can be merely indicative of failure (technical errors, lack of biological integration) and occur within the first six months or constitute the main factor responsible for the rupture of the transplant (traumatic ruptures) and then reveal itself one year, sports activities having been resumed. The occurrence of a sports trauma after LCA ligamentoplasty varies from 24 to 57% according to the authors. This relatively high frequency is explained by the fact that an imperfect surgical technique can also be decompensated during a real trauma. The intricacy of several factors can make it difficult to analyze failure in a traumatic context. We described spontaneous recurrence after LCA ligamentoplasty in a context where macrotrauma played a key role in explaining the lesion (s) observed.
What are the different anatomoclinic entities that characterize sprain recurrences?
Several clinical pictures can be revealed depending on the circumstances of onset, the importance of laxity and imaging.
The transplant is completely distended or broken:
Complete traumatic rupture or distension:
The only trauma is responsible for a complete rupture of the transplant without there being a technical defect linked to the intervention. The new accident usually occurs at least one year after the procedure and after a free interval of several months or years during which all sports activities have been resumed at the same level. A real lesion is found during the second trauma. The functional signs of severe sprain are in the foreground. The knee already operated was stable before the new accident. The IKDC score of the ligament examination section had been side A or B at the very last setback. The sign of Lachman is frankly positive and side ++ or +++ soft stop. The sign of the jump is next grade II or III by an experienced examiner.
The biomechanical incompetence of the intra-articular graft is not discussed. The comparative anterior laxity measured with the Telos ® at 250 N or with the aid of the KT 1000 TM in the maximum manual traction mode is strictly greater than 5 mm. Bone tunnels are generally well positioned on standard X-ray images. A transplant continuity solution is most often observed at MRI. Hypersignal fluid areas completely erase the graft on part of its path. When the graft is completely distended, some of the broken fibers are affected by T2-weighted signaling areas. The knee is sometimes artefacts by the metal fixings which do not prevent a good analysis of the transplant in the notch. Osteochondral lesions and bone hyperinsignal lesions are documented at MRI in more than 80% of cases of ACL rupture. According to Spindler et al., The lateral condyle is reached in 68% of the sprains. Can bone signals persist at a distance from the first trauma and still be observed after a sprained recurrence? The volume of bone hyperintensity decreased for Davies et al. more than 50% for 80% of patients at 12 weeks of follow-up. Bretlau et al. observed only 12% of persistent hypersignals one year after the trauma. Faber et al. followed 35 sprains with LCA reconstructed.
All had occult lesions of the lateral condyle.
Sixty-five percent of the cases (15 cases) had a persistent bone signal at six years, with only 8.7% (two cases) with thinning of the cartilage. The author evokes a fibrous healing with hyposignal in T1 and T2 of the bone lesion initially perceived in hyposignal in T1 and in hypersignal in T2. In contrast, a low T1 bone marrow in T2 suggests a recent lesion. Prospective studies are needed to verify whether these occult lesions may or may not be according to the importance of the trauma, precursors of degenerative phenomena.
Late progressive rupture or distension:
No responsible trauma has been observed. Only a prolonged follow-up makes it possible to demonstrate the successive degradations of the transplant over time. Rollier et al. have observed on a series of 74 cases of ligamentoplasty, 22 cases of progressive degradation without the notion of trauma. A pre-osteoarthritic condition (sequelae of meniscectomy) can also constitute an unfavorable degenerative and mechanical environment for the graft which may conflict with possible osteophytosis at the notch. An innocuous pivotal movement can end up being revealing of failure.
Early anatomic failure:
The distension occurs during the first year as soon as the sport resumes during a benign accident. At the MRI, the transplant is often continuous and perceived in hyposignal throughout its anatomical path. A defect of biological incorporation of the graft is most often responsible. The laxity may also appear just after the procedure. A minor trauma is sometimes reported.
Failure to fix or excessively aggressive rehabilitation is then called into question.
The transplant is partially broken or distended:
Partial rupture or distension occurs accidentally after a free interval during which pivotal sports activities have been resumed. The residual laxity was less than 2 mm before the new trauma. The IKDC downshift of the laxity takes place at level B. The maximum differential is then between 3 and 5 mm.
The jump is grade 0 or grade I. The continuous MRI transplant is perceived as hyposignal in T1 and T2. Some fibers of the graft may also be ruptured and affected at an early stage by T2 hypersignal fluid ranges. Hypersignal bones are less frequently observed in cases of incomplete lesion of the central pivot. Zeiss et al. observed a bone hyperintense in 12% of the incomplete lesions of the ACL versus 72% in complete ruptures. A clinical reassessment of a relaxed patient and a new imaging after hemorrhagic resorption allows the diagnosis to be made more accurately at a distance from the trauma. The strength of the graft should be confirmed more remotely with the resumption of pivotal sports. In doubtful cases, the clinical examination under narcosis will allow the precise analysis of the laxities and especially the quantification of the jump that remains at the base of the decision tree.
The transplant is intact:
Traumatic meniscal lesions or weak distension of peripheral ligamentous formations are responsible for moderate haemarthrosis. An osteochondral lesion is more rarely involved. The residual laxity and the sign of the jump on the grade 0 or grade I side remained unchanged after the second accident. The LCA transplant appears at continuous MRI and in hyposignal. In case of arthroscopy for secondary meniscal lesion, the transplant appears well vascularized thanks to the synovial sleeve that surrounds it.
Secondary traumatic meniscal lesions:
The rate of occurrence of secondary lesions varies from more than five years to between 5 and 10%, depending on the series. The traumatic meniscal lesions in the vascular zone are most often sutured or spontaneously healed with the repair of the central pivot.
Meniscal lesions treated initially conservatively should be compared to newly observed lesions. For the diagnosis of medial (lateral) meniscal traumatic lesions, MRI was chosen to be 97% (82%) and 97% (96%) with good sensitivity.However, a hypersignal corresponding to an old healed lesion may persist for at least five years in the rupture zone.Arthro-MRI or arthroscanner then make it possible to better differentiate a recent fissure from an old scar formation.The meniscal blockage corresponding to the classic bucket handle constitutes a functional emergency. Grade III marked by a solution of continuity at the level of the meniscal wall testifies to a more or less extensive transfixing rupture. Secondary meniscal lesions, which are often expressed in an iterative sprain, must give rise to suspicion of an anterior or residual laxity which must be demonstrated.
Particular case of the associated involvement of medial peripheral formations:
The lesional mechanisms in valgus-flexion-external rotation are responsible for a first attack of the medial peripheral formations. The clinical examination easily shows, with a knee flexed at 20 ◦ , an internal yawn more or less important and spontaneously reducible. The sign of Lachman is often positive after reconstruction of the LCA. The anterior drawer may be further aggravated by the superposed distension of the postero-internal corner point which constitutes a secondary brake to the advance of the internal compartment. The jump also requires the integrity of the internal ligament strut to express itself fully under the effect of valgis- ting stresses.
The LCA plasty can then be better evaluated after healing of the medial collateral ligament and the postero-internal angle.
Risk factors:
Meniscectomy associated with LCA reconstruction:
Meniscal preservation protects against osteoarthritis and ensures better anatomical results in the long term. Salmon et al. studied risk factors on a limited series of nine failures (13.4%) from a retrospective and continuous series of 67 bone-tendon-bone transplants, 85% of which were reviewed at 13 years of follow-up. The meniscectomy associated with LCA reconstruction increased the risk of secondary transplant rupture by a factor of 6.
The medial meniscus which is a secondary brake of the anterior tibial translation protects the graft of the LCA with decreased residual laxity.
Gender-related factors:
Women are four to six times more likely to have an LCA sprain than men for equivalent sports activities. Twenty-two percent of young Alpine skiers break their transplant again.
Genetic factors, hormonal and anatomical entangled with associated neuromuscular factors explain the increased risk of ACL rupture in women.
Hormonal Factors:
Can the menstrual cycle, in particular the ovulatory peak, have an influence on the mechanical properties of the LCA?
A recent meta-analysis of the literature on nine prospective cohort studies showed an increase in ACL laxity during the ovulatory and postovulatory phase. Only three of these studies showed that the influence of the menstrual cycle on LCA laxity was significant. In vitro, sudden increases in estrogen prematurely inhibit fibroblast proliferation and procollagen synthesis of type I. This effect is attenuated with the addition of progesterone which would have a protective effect. In vivo in the spleen, the breaking strength and stiffness of the LCA did not vary significantly during the different phases of the menstrual cycle.
Can hormone receptors influence the remodeling of the graft? The laxity of LCA was not for Blecher and Richmond affected by pregnancy.
Eiling et al. did not observe during the menstrual cycle of variation of the anterior laxity contrary to the musculotendinous stiffness significantly lower during the ovulatory phase. The less contractile muscles would react less quickly to ensure proprioceptive control. Certain periods of the hormonal cycle also make them more vulnerable to sports accidents.
Wojtys et al. showed an increase in trauma during the ovulatory phase.
On the other hand, in the basketball players, LCA sprains occurred preferentially during the two days following menstruation. The discordant results according to the authors do not allow to really decide and to impose, in the operated patients of a rupture of the LCA, a preventive behavior according to the hormonal cycle. In women, the evolution of bone mass, in particular the mineralization of trabecular bone, is closely related to estrogens. The hardness of the spongy bone situated at the level of the tibial metaphysis remains in the female overall less than that of the man to ensure a solid bone-tendon fixation.
Corry et al. have obtained better laximetric results with the bone-tendon-bone transplant in the woman at two years than with the four-strand internal and semitendinous tendons. Bone mineral density is markedly decreased in young women with primary ovarian failure unsubstituted by estrogens.
Hill et al. recommend in reconstructions using the ischiojambic tendons in women the systematic addition of a ligament staple with the tibial interference screw to avoid the phenomenon of slip and thus ensure better results laximetric.
A lack of tibial fixation may lead to early failure in the first trimester.
Genetic factors:
The expression of the matrix metallopeptidase 3 (MMP3) protease coding gene that reshaped the ligaments would be decreased in women, which would have adverse consequences on the histological structure of the ACL.
Anatomical Factors:
A narrower notch in the woman houses a smaller LCA with a smaller cross-sectional area, minimizing the conflict theory and corroborating the idea of a more fragile central pivot. The cross-sectional area of the LCA at the cross-over with the LCP is smaller in women than in men of equivalent weight. This relative thinness of LCA in women results in an increase in intraligamentary stresses for an equivalent tension force. The connective tissue used for transplantation must, regardless of sex, have sufficient immediate biomechanical qualities at least equal to the native LCA. Salmon et al. did not observe more secondary ruptures in women in a cohort study using ischiojambular tendons at seven years of follow-up. However, laxity and leapfrogs were statistically less important for humans.
Neuromuscular control:
The knee is potentially more unstable in indirect lesional mechanisms because of three neuromuscular dominances explaining the proprioceptive imbalances in women.
Ligament dominance:
Ligament stresses occur before protective muscle activation during torsional movements.
The quadricipit dominance:
The recruitment of quadricipital fibers is superior to that of the ischiojambic muscles in sports gestures.
LCA ruptures usually occur on a knee near the extension. The harmful role of the quadriceps is then linked to the anterior tibial translation force, which is the component of the traction force of the patellar tendon. Young athletes also use a quadricipital muscle activation sequence that contributes to the dynamic valgus.
The dominant member:
Coordination, flexibility and muscle strength are much better in the dominant member. The opposite member then remains more vulnerable to sporting constraints.
The plyometric training exercises working the power and explosiveness of striated agonist muscles against weightlessness have shown efficacy in the prevention of LCA sprains in young women.
These reprogramming techniques involve neuromuscular facilitation and provide better control of knee movements while enhancing athletic performance.
Constitutional Factors:
Narrowness of the indentation:
Morphometric studies of the distal femur were able to establish a relationship between the narrowness of the intercondylar notch and the risk of rupture of the non-contact LCA. Nevertheless, there is the problem of the variability of the groups of populations studied and the uncertainty of the radiographic measurements. The anterior indentation, the anatomical zone of potential conflict with the transplant, remains in man and woman narrower than the posterior indentation:
• patients with bilateral LCA rupture have a narrower indentation than those with unilateral involvement;
• femoral bicondylial width is proportional to the width of the indentation for both sexes;
• the indentations of patients who had unilateral or bilateral LCA disruption independently of sex are narrower than those measured at a control population.
The distribution of these measures on the basis of sex showed an increased narrowness in women.
Anderson et al. have not found a gender disparity. The notion of threshold value is in fact difficult to establish. The probability of having a LCA sprain in relation to a narrow notch should be further defined by prospective cohort studies.
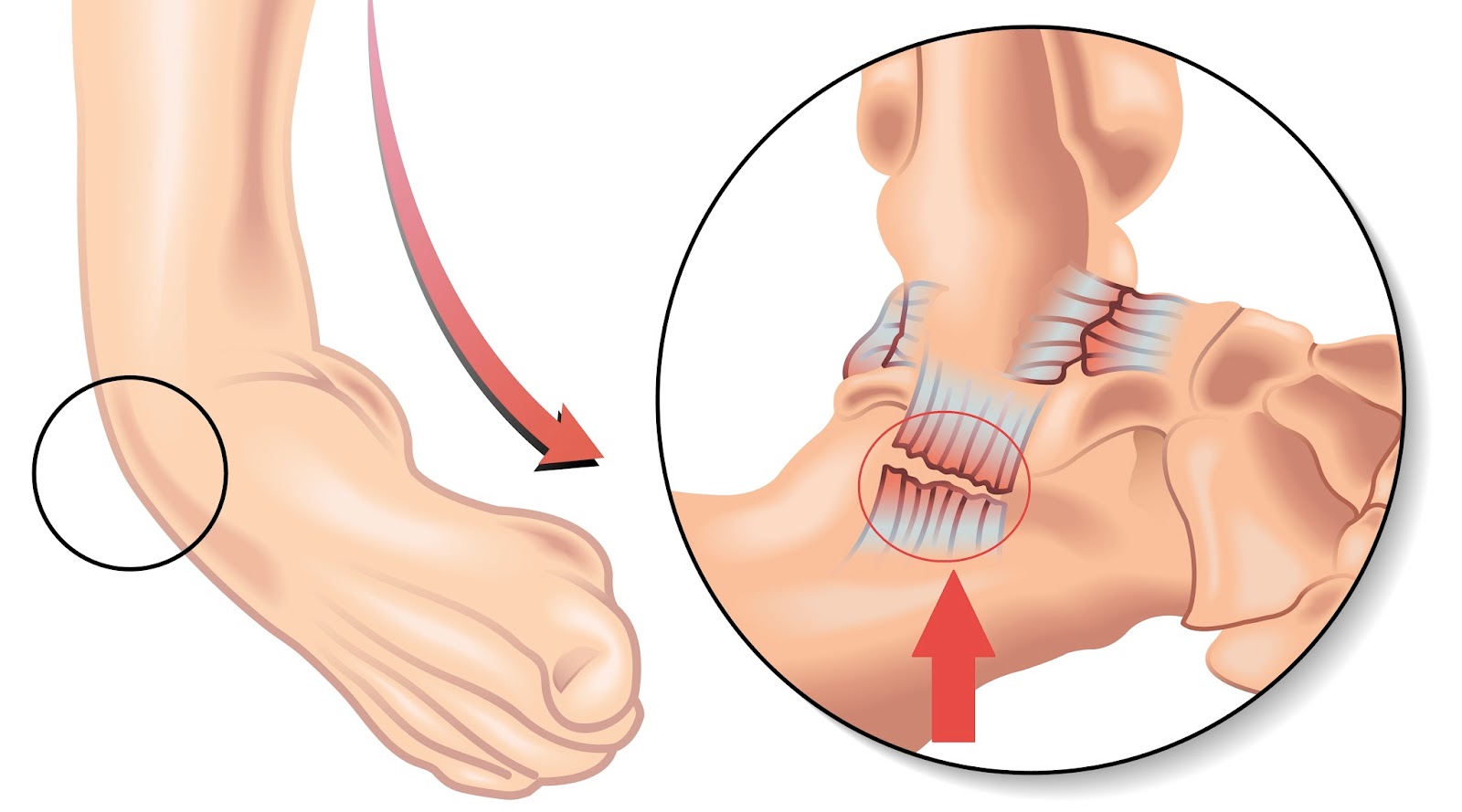
Tibial slope:
Brandon et al. have linked the increase in the tibial slope with LCA ruptures. The tibial slope generates at full load shear forces at the level of the two tibial plates causing an excess of stresses at the level of the ACL. An increase in the tibial slope of 10 ◦ majore for Dejour and Bonnin the anterior tibial translation of 6mm in monopodal support.
Tibial osteotomies of anterior subtraction decrease the tibial slope by increasing the recurvatum.
Genu recurvatum:
The recurvatum may be of bone and / or capsuloligament origin. Hyperextension results in physiological contact between the transplant and the roof of the notch.
The positioning of the graft is then decisive to avoid a conflict with the top of the anterior notch which forms a gothic ogive more or less narrow which constitutes in hyperextension a true guillotine to LCA.
The anisometry of the transplant generated by hyperextension is also an indisputable factor of distension. Anterior addition tibial osteotomies increase the tibial slope. The indication can only be reasonably posed in the case of instability related to the genu recurvatum or, in the case of recurrence of a sprain associated with a sagittal deformation greater than 20 </s>.
Overweight :
The stresses borne by the graft are proportional to the template and the physical activity of the patient. Is the available connective tissue still sufficient to make a strong autograft? The diameter of a four-strand ischiojagier graft usually ranges between 6.5 and 8.5 mm. The size of the tendons does not always vary in a proportional way to the body mass. Thus, in patients with heavy ischiojam tendons that are relatively slender, there is the problem of using additional lateral tenodesis or using the patellar tendon. The modularity of the fascicular grafts makes it possible to increase their diameter by making transplants with five or six strands tendinous. A four-beam plasty using only the half-tendinous tendon makes it possible to obtain a thicker graft at the cost of a shortening of the tendon which requires the graft to be suspended in line with cortical fixations.
The bone-tendon-bone transplant should not exceed 10mm in width to avoid a harmful weakening of the stent.Shelbourne and Johnson showed that the total width of the patellar tendon removed could also have an influence on the recovery of muscle strength. The weight, height and body mass index were for Bowers et al. of the predictive factors of chondral and meniscal lesions observed during the reconstruction of the LCA. A high body mass index in women is also considered a predisposing factor for non-contact lesional trauma. Weight reduction is desirable prior to surgical recovery to achieve a body mass index of at least 30 kg / m 2 or less.
Factors related to rehabilitation and sports recovery:
Can intensive rehabilitation programs result in distension of the transplant? A prospective and continuous series of 25 active patients operated on a bone-tendon-bone plasty were randomized into two groups comparing the results obtained after a classical and accelerated rehabilitation. The increase in laxity at two years of recoil (90 N tensile at KT 1000 TM ) showed no significant difference between the two groups with 1.8 mm for the non-accelerated group and 2.2 mm for the accelerated group . The phenomenon of sliding at the level of the anchoring by interference screw associated with a relaxation of the transplant explains for the latter author the increase of the laxity during the first months.
Barber-Westin et al. have adapted their rehabilitation program with the bone-tendon-bone transplant as a function of the follow-up of the repeated measurements of the laxity which makes it possible to detect at an early stage any distension of the graft. Five percent of failures in the first year were reported with a slight upturn in sporting activities at six months and competition at eight months. The accelerated rehabilitation initiated with the patellar tendon by Shelbourne and Nitz must be tempered in order to protect the donor site and avoid the awakening of anterior pains which can on the contrary hinder the sporting recovery.
With the ischiojambic tendons, bone integration takes place later at 12 weeks; intensive rehabilitation should be avoided to reduce the enlargement of bone tunnels.
Salmon et al. studied the incidence and risk factors of sprain recurrences in a continuous series of 675 plasties (316 bone-tendon-bone transplants and 427 transplants using the four-stranded ischiojack tendons) five years later. The rupture of the transplant occurred preferentially in the first 12 months with a risk multiplied by three in the case of an initial indirect injury mechanism and by two in the event of a revival of a sport with pivots. An age of less than 21 years was also retained as a derogatory factor by multiplying the probability of a new break in the central pivot by ten. Young athletes must therefore be closely supervised during the first year, strictly adhering to a set of specifications before the resumption of the sport. Proprioceptive disorders more or less associated with muscular insufficiency may, depending on the sports discipline, lead to an iterative sprain during indirect lesional mechanisms.
Skiing and football are the biggest breeders of the LCA. Indirect lesional mechanisms with foot-to-foot blockage are particularly frequent during football activity that excessively biases the knee in internal rotation, posing the problem of stabilizing the external compartment to reduce the risk of failure long term.
Ligament Factors:
Distinction associated with important points of angles:
The posteromedial angle is a secondary brake to the anterior tibial translation. The weakening of the latter after medial meniscectomy thus leads to an increase in stresses at the level of the transplant.
Dejour et al. had proposed using the bone-tendon-bone transplant to tighten the postero-internal capsule in case of differential anterior laxity greater than 10mm. The evolution of arthroscopic techniques has minimized the importance of associated peripheral ligament gestures. Early intervention also allows for better preservation of the medial meniscus, which can thus play its role as a protective wedge. The posterolateral angle is more rarely reached in chronic anterior laxities and the diagnosis is often occluded; the tibial epiphysis turns spontaneously in external rotation. In the case of lateral tenodesis associated with the repair of the central pivot, the position of the tibia should be observed before attaching the transplant. The popliteal tendon plasties well described by Jaeger et al. are
in fact most often used for combined posterior laxities.
Associated chronic frontal laxity:
A medial or lateral decoaptation associated with an unfavorable and significant deviation of the morphotype constitutes an indisputable factor of failure. The central pivot is no longer protected in movements of valgus or varus flexion. A normocorrectary osteotomy realigning the lower limb remains an indispensable prerequisite before the iterative reconstruction of the ACL. The reactions and the plasties of the peripheral formations showed in chronic distensions anatomical results less good than those obtained in the recent repairs.
Constitutional Hyperlaxity:
Scerpella et al. have established using the score of Beighton et al. a link between the genu recurvatum, the anterior tibial drawer, the generalized hyperlaxity and the spontaneous occurrence of the non-contact ACL. These last parameters of analysis are prevalent in the woman and explain in part the recurrences of sprain. Sung-jae et al.observed in hyperlax patients (Beighton et al. score greater than or equal to 4) two-year laximetric results significantly better with the bone-tendon-bone transplant (3.4 ° æ1.5mm) compared to those obtained with the ischiojambic tendons (4.5 ° æ2.0 mm). These two authors used anatomical fixation by interference screw for the two types of reconstruction, the rigidity of the patellar tendon and the bone-os fixation then explain these results.
Rotational laxity:
The importance of rotational laxity must also be taken into account. Giraud et al. (lateral compartment differential greater than 8 mm), the combination of a lateral extra-articular plasty allowing a reduction of stresses at the level of the transplant.
Bad positioning of bone tunnels and technical errors:
The poor positioning of the bone tunnels constitutes for Carson et al. the most common cause of non-traumatic failures. These authors analyzed the causes of failure in 90 iterative reconstructions. Forty-seven technical errors and 22 cases of traumatic ruptures were dismembered with seven cases of biological integration failure. Garofalo et al.observed in a series of 28 cases of failure resumed by an autograft of the quadricipital tendon, a femoral tunnel too anterior in 79% of the cases. A poor placement of the tibial and / or femoral graft may adversely affect the anatomical results with the consequence:
• a more or less favorable anisometry leading to secondary relaxation of the graft;
• a transplant conflict with the anterior edge of the notch and / or the LCP. Navigation would position the earlier anterior tibial tunnel while avoiding this conflict;
• an excessive divergence between the direction of the stresses exerted and the major axis of the graft.
In case of recovery, the choice of the autograft and the realization of the bone tunnels should be planned after analyzing the causes of the failure. A two-stage surgery involving the prior filling of bone defects with a corticospongic autograft may be indicated in cases of significant osteolysis. The results of the iterative reconstructions of LCA showed overall worse results than those obtained in first intention. The 2006 Symposium of the French Arthroscopy Society on LCA iterative surgery revealed 73% of cases of meniscectomy after the second intervention. One third of the patients were only rated IKDC A. The control of the jump was better ensured (p = 0.03) by performing a mixed plasty for the iterative reconstruction of the LCA.
Conclusion:
The etiologic diagnosis of a knee sprain after LCA ligamentoplasty must be conducted rigorously by an experienced examiner. Clinical examination, the instrumental and radiological laximetric balance allow, with reference to the healthy knee and the injured knee examined at the last recoil, the functional evaluation of the graft. The threshold of the differential anterior laxity attesting a rupture is 5 mm. A continuous, hypointense transplant to MRI does not eliminate biomechanical incompetence. A scarred meniscus can simulate a recent lesion on MRI, which requires a prior opacification. The clinical examination under narcosis allows, in some difficult cases, the precise analysis of the laxities and especially the quantification of the jump that remains at the base of the decision tree. The analysis of risk factors for a sprain recurrence after ligamentoplasty does not always allow preventive action. Other prospective studies are needed to better evaluate the distension factors that ideally allow to establish a risk score.