Six thousand ankle sprains occur every day in France, 1200 of which are severe sprains (rupture of one or more bundles of the lateral collateral ligament). These numerical estimates point to the importance of the problem on the personal level, but also on the economic level.In 2003, a US study put forward the $ 3.65 billion needed to cover the costs of these sprains.
Six thousand ankle sprains occur every day in France, 1200 of which are severe sprains (rupture of one or more bundles of the lateral collateral ligament). These numerical estimates point to the importance of the problem on the personal level, but also on the economic level.In 2003, a US study put forward the $ 3.65 billion needed to cover the costs of these sprains.
But the overwhelming majority, even if serious, if properly analyzed and dealt with in a coherent and appropriate way, will be cured.However, 20-40% of these first sprains will leave the sequelae, for lack of a precise diagnosis and a therapeutic without fault. This is not the place to revisit these shortcomings, but it was important to emphasize this fact at the outset: there should be practically no sequelae of any order whatsoever.
For a very long time, chronic laxities, due to ligament insufficiency, were considered the most frequent and disabling.Over the last few decades, evidence has been provided that this is not the case: the painful sequelae appear in the foreground by their number and variety.
But it is not appropriate to attribute too quickly any chronic pathology of the ankle to the after-effects of a sprain of which any sportsman has been the victim during his career, in the same way that often any acute trauma to baptize it “sprains “ indiscriminately. For this reason, a complete, “ programmed “ examination is needed for this “ chronic “ ankle.In all cases, it will be followed by the additional examinations necessary for the establishment of a precise diagnosis.
Clinical examination:
It must be practiced methodically, on a patient without socks or pants, standing upright, in dorsal and ventral decubitus, in order to explore all the anatomical structures.
The interrogation involves two essential periods:
• the exact description of the initial trauma: mechanism, immediate follow-up, symptomatology, complementary examinations, treatment and follow-up are the main elements;
• the precise description of the current disorders: is it a recurrent sprain or pain? This is an opportunity to emphasize that we must not confuse:
◦ instability: functional symptom related to multiple etiologies. Sensation of insecurity which can be due just as much to brutal pains that give the patient the impression that his “ loose “ ankle, than a true ligamentary insufficiency,
◦ laxity: physical sign found on examination. As a source of repeated sprains, it signs the ligament insufficiency due to non-healed initial lesions.
If it is pain, it is necessary to specify whether they are acute or chronic, their evolution in time, their location.
The inspection examines:
• the axis of the hindfoot, normally in slight valgus, well emphasized by the relief of the calcaneal tendon. Local swelling or swelling is also sought;
• the overall axis of the lower limb, knowing that a genu varum or genu valgum necessarily sounds on the static of the talocrural articulation.
The palpation indicates the presence or not:
• Painful points. All the osseous structures (malleoli, tibial margin, talian dome) and tendinous structures, all around the ankle should be palpated carefully;
• an articular effusion, clearly visible especially on the anterior surface;
• localized swelling, especially on tendon pathways.
The joint amplitudes are analyzed:
• for talocurural articulation in flexion and extension, often showing a limitation of flexion when sufficient attention is paid to it;
• for the subtalar articulation by strongly empalating the calcaneal block and immobilizing the talus under the malleoli.This search for pronosupination can be done in supine position but better, on the patient in ventral decubitus, knee flexed at 90 ◦ .
It should be noted whether these mobilizations cause pain or cracking.
Abnormal movements are tested:
• anterior drawer, looking for either the retreat of the leg segment on the patient in the supine position, the foot resting on the table and the knee flexed (Landeros maneuver), or the advance of the foot under the tibial segment in the ventral decubitus, of the table ;
• forced varus by picking up the entire hindfoot and mobilizing it in relation to the leg segment, again in dorsal or ventral decubitus.
The search for these abnormal movements has all its value in the framework of a chronic ankle, at a distance from any recent trauma. Needless to say, this research must be bilateral so as not to be overtaken by constitutional hyperlaxity.
The search for tendon pathologies is carried out according to the usual method: besides the palpation, by the tensioning and the contraction resisted. All tendons around the ankle should be examined.
The neurological examination is essential: sensitivity and motor skills, especially in the territory of the common fibular nerve.
Complementary examinations:
They are essential supplements and include: standard radiographs, always indispensable as first-line. Four shots are necessary (ask only “ face and profile “ would be a fault):
• face antler in neutral rotation;
• an ankle with an internal rotation of 15 ◦ to fully clear the talocrural spacing and, in particular, the supersolateral angle of the talus and the tibiofibular space;
• profile anchor;
• unrolled the foot (or oblique external) to analyze bones and joints of the mediopod and base of the fifth metatarsal.
The second-line examinations (ultrasound, CT, arthroscanner, MRI) are only complementary, oriented by the clinic and the standard radiographs according to the diagnosis mentioned and taking into account the specificity of each imaging technique.
Differential diagnoses:
Voluntarily, this paragraph is placed immediately because it is often too easy to attribute this “ chronic “ ankle to sequelae of sprain, while many other pathologies may be involved. Without entering into the details of each of them, it is only necessary to cite them in order not to misunderstand them:
• sequelae of other bone traumas, such as those of unimallerolar, talian, anterior or posterior marginal fractures of the base of the fifth metatarsal, for example;
• sequelae of the lower tibiofibular sprain, too often not initially diagnosed, or sprain of the Chopart joint;
• all non-traumatic pathologies, whether inflammatory (rheumatoid arthritis, pelvispondylitis), infectious or tumoral, tendinous or bone, benign or malignant. It should always be remembered that an athlete can suffer from a pathology that has nothing to do with sport.
Both the clinical examination and the complementary examinations should make it possible to evoke them in order to eliminate them.
Schematically, the sequelae are presented under two tables:
• the “ painful “ ankle;
• the ankle “ unstable “ despite, of course, a certain interpenetration of different pathologies.
The “ painful “ ankle:
This is the most frequent picture and in recent years have allowed for dismemberment thanks to a more precise clinic and high performance imaging.
The characters of these pains must be specified. They can be:
• acute, brutal and intermittent, often giving rise to sensations of instability or insecurity, to be clearly defined by interrogation so as not to be misled and to go too easily to the diagnosis of chronic laxity;
• chronic and quasi-permanent with, again, many shades less decided.
There are many pathological pictures. They can be presented as follows.
Periarticular fibroses:
They are the most frequent cause of the painful sequelae of sprains. This fibrosis is due to the “ pathological “ healing of the initial capsuloligamentar lesions.
Clinical signs of orientation:
• Painful ankle swelling, permanent;
• often limited amplitudes, especially in dorsiflexion, more troublesome;
• Painful points that have a valuable localization value.
A particular form has been described in 1950 by Wollin et al. : the anterolateral conflict. This is a cicatricial fibrosis filling the prefibular gutter where there is swelling and painful point caused clearly localized.
It corresponds to a hypertrophic scar tissue in the anterior beam of the lateral collateral ligament on which local inflammatory reactions are grafted.
Complementary examinations:
• Standard radiographs are usually normal.
Sometimes there is a seedling of small calcifications.
• Ultrasound and CT (or MRI) show perfectly fibrosis, its importance, its location.
The treatment:
• “ medical “ primarily through physiotherapy and infiltration, which is most often enough;
• surgical in case of failure, for debridement and partial synovectomy by arthroscopy.
But the results are sometimes incomplete with, in particular, persistence of a discreet limitation of the amplitudes, especially in dorsal flexion.
The earlier astragalian conflict:
Described by Basset et al. in 1990.
Clinical signs of orientation:
Anterior pain on the tibiotal line.
Apart from the previous painful point, the clinical examination is negative. At the most, it is found that this pain is increased by dorsal flexion and diminished on the contrary in plantar flexion.
The explanation of the syndrome is due to the presence of an accessory bundle of the anterior and inferior tibiofibular ligament, situated beneath the principal ligament from which it is separated by a small fat lobule. Since the ankle is the seat of a residual laxity, even if it is minimal and subclinical, the anterolateral part of the talian dome conflicts with the accessory bundle, which may be the cause of localized chondral lesions.
Complementary examinations:
The problem is that this accessory bundle is present in 80% of the individuals and that nothing comes to prove its responsibility in the symptomatology presented by the patient, especially since the chondral lesions of which it could be the cause are always very discreet:
• standard radiographs are normal;
• ultrasound, CT and MRI are usually normal.
The diagnosis is based on clinical and arthroscopy, both diagnostic and therapeutic.
The treatment:
Arthroscopic resection of the accessory beam.
The para-articular ossifications
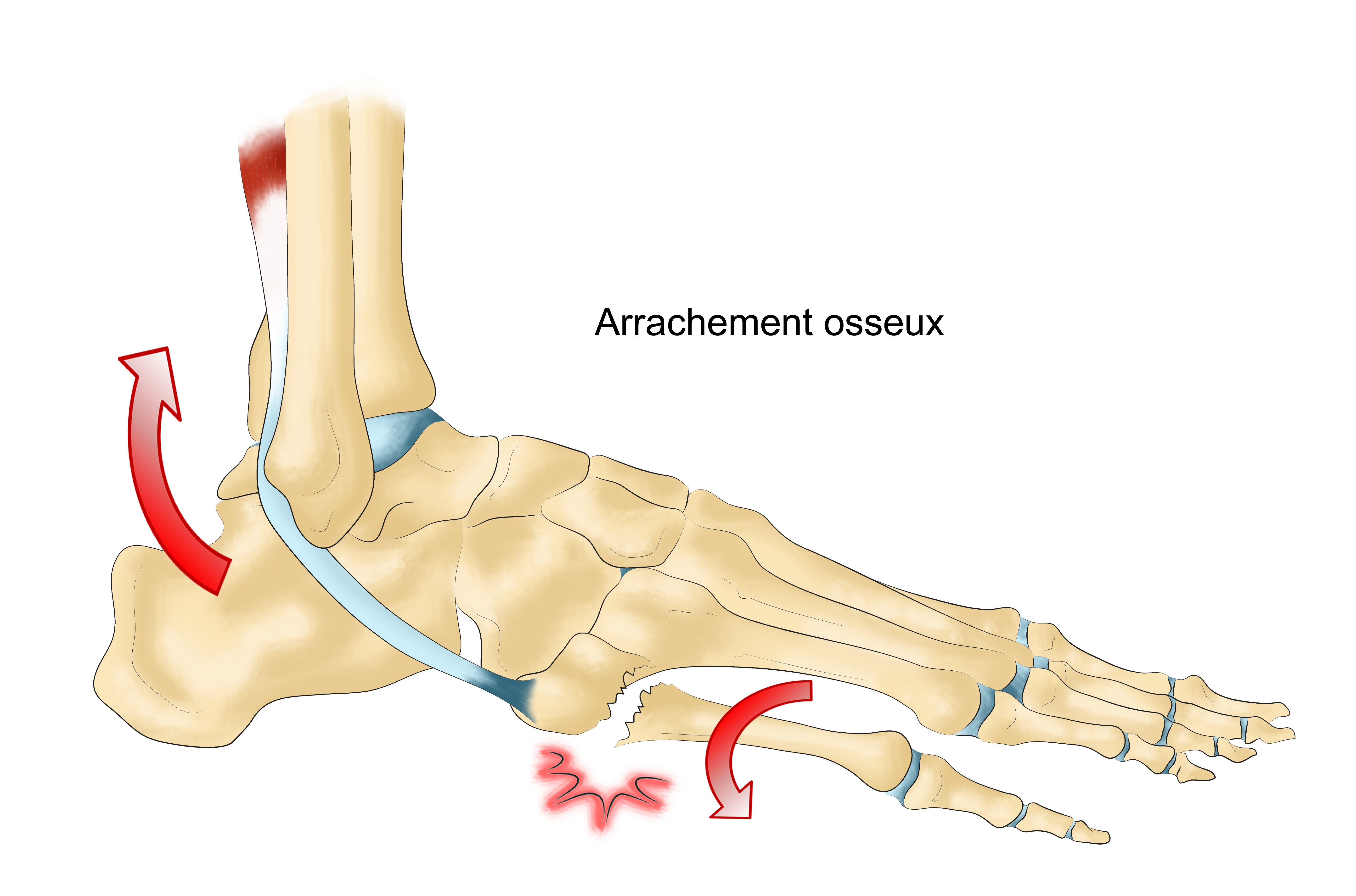
They are the consequence of direct microtraumatism or the sequelae of small capsular or ligamentous pulls consolidated in vicious position.
Deforming the malleolar points or the tibial margins, they are the cause of conflicts with the dome or the talian cheeks.
Clinical signs of orientation:
They are usually referred to as chronic pain, but also sometimes acute as joint seizures in the aftermath of forced movement.
The examination finds localized pain points, medial or lateral, especially during the mobilization of the foot.
Complementary examinations:
• Standard x-rays easily prove this;
• an arthroscanner can reveal chondral lesions on the corresponding dome or tal cheek.
The treatment:
• “ Medical “ by physiotherapy or infiltration: may be effective, but too often provisionally;
• surgical, rather arthroscopic by resection of the ossification, thus bringing a definitive result.
Foreign bodies:
The forced varus movement, responsible for the sprain, is the cause of impacts of the talus against the tibiofibular mortise which can generate small osteochondral fractures. Unbound, they will cause foreign bodies.
They can be :
• intra-articular, located in the lateral spaces between malleoli and cheeks;
• Periarticular and embedded in the ligament, medial or lateral planes.
Clinical signs of orientation:
• Acute, joint pain, but sometimes chronic pain. If they are intra-articular, there may be incidents of true blockages;
• In all cases, there may be feelings of insecurity or even instability.
The clinical examination is poor. At most, an ossification is sometimes perceived if it is superficial and sub- or pre-premolar. May cause pain and cracking during mobilization.
Complementary examinations:
They must not only show foreign bodies but also locate them: intra- or periarticular. From this location will depend the type of treatment to be proposed:
• standard X-rays, provided that the lateral spaces are well separated;
• CT and arthroscanner.
It is necessary to know that it is always necessary to start with a simple CT, the contrast product can mask calcified foreign bodies. On the other hand, the arthroscanner alone is capable of showing purely cartilaginous foreign bodies and possible chondral lesions.
The treatment:
• Intra-articular foreign bodies must be removed by arthroscopy;
• periarticular foreign bodies:
◦ one can first try the “ medical “ treatment by physiotherapy and infiltrations,
◦ in case of insufficient results, and without waiting, ablation by arthroscopy. But it is sometimes ineffective in removing foreign bodies embedded in the lateral ligaments or adjoining the malleoli. An arthrotomy must then be used.
The ankle known as “ the sportsman “
It is an entity distinct from osteoarthritis, of which it is differentiated by the absence of articular pinching, but of which it represents perhaps an initial state.
It is, in fact, the summation of the previously described arrays with articular and periarticular ossifications, anterior, medial, lateral and posterior and fibrous thickenings, sequels of multiple microtraumatic lesions of the ankle.
The clinical signs of orientation and the means of imaging are identical to what has already been mentioned.
The treatment is primarily conservative and often allows the pursuit of the sport. The surgical treatment is justified, as before, only in case of failure and repeats the same techniques.
The osteochondral lesions of the slope dome:
It is a vast chapter because, for the same location on the slope dome, four types of fundamentally different pathologies can be observed:
• Pseudarthrosed parenchyma fractures of the talian dome, usually super-lateral, contemporaneous with the initial severe ankle sprain;
• adolescent osteochondritis, which is almost always medial and can become painful as a result of trauma; it is sometimes bilateral;
• dystrophic or partial necrosis lesions, medial or lateral, of pathogenesis discussed but almost always secondary to an old trauma;
• intraosseous mucosal cysts, probably secondary to traumatic chondral lesions.
If the clinical expression is rather unambiguous, the radiological images and the treatment are different.
Clinical signs of orientation:
They are made of chronic pain with sometimes acute episodes. There may also be feelings of insecurity, fugitive blockages and joint cracking.
Clinical examination is almost always remarkably poor.
Complementary examinations:
Given the paucity of signs of examination, they must be done in the slightest doubt in front of any chronic painful ankle.
The aim is not only to authenticate the lesion, but also to specify its type and, above all, to study the state of the cartilaginous coating:
• well-oriented and well-penetrated standard radiographs are indispensable but often insufficient for accurate analysis;
• CT and arthroscanner are the key examinations, far superior in this context, to MRI in the current state of the art, especially for the study of cartilage.
Thus, it is possible to precisely define the type of the lesion and to deduce the therapeutics to propose:
• the pseudarthrosis of an osteochondral fracture occurs in the form of a thin osteochondral scale of supraprolateral seat);
• osteochondritis is seen in an adolescent with the image of “ egg to nest “ in its typical form and supra-medial seat);
• dystrophic lesion or partial necrosis, medial or lateral seat, with chondral lesion and changes in the underlying bone with irregular multi-periodic images);
• the intraosseous mucosal cyst in the form of an optically empty subchondral cavity. If one takes the time to resume the examination after mobilization of the ankle and, better still, after having asked the patient to take a few steps, one can observe the partial opacification of the cavity, authenticating the chondral lesion).
The treatment:
• Pseudarthrosed particle fracture should be removed by arthroscopy rather than by arthrotomy. Its volume does not usually allow attempts at repositioning and osteosynthesis. But the diminution of the articular amplitudes which its presence has engendered for several months, even several years, often persists. This confirms that it is at the initial stage that these fractures must be treated;
• First, osteochondritis must prove absolute responsibility for painful symptoms.
It is only then that the surgery is justified for ablation of the nucleus and perforation of the bottom of the niche, by arthroscopy;
• the dystrophic and necrotic lesion responds, if the lesion is shallow, to simple curettage under arthroscopy.
On the other hand, if it is deep, it must be filled in conventional surgery, which can be done by different means: spongy grafts taken at the level of the lower tibial epiphysis or osteocartilaginous mosaic grafts taken from the medial cheek of the femoral trochlea;
• the intraosseous mucosal cyst responds to the same techniques.
The posterior crossroads syndrome:
It is due to the phenomena of posterior “ wedging “ between the posterior margin of the tibia, the tail of the slope and the posterior part of the subtalian articulation, consequence of the initial trauma in forced equine varus and aggravated by repeated microtraumatisms in forced plantar flexion . They are responsible more or less for posterior fibrosis, osseous changes in the tail of the talus (bone trigon), cystic dilatations developed from the posterior synovial cul-sac or osteochondral lesions located in the talocrural and / or subtalian posterior joints.
Clinical signs of orientation:
• Acute posterior pains in trauma in forced plantar flexion (tackle, shoot counter) which “ nail “ the player on the spot;
• Reproduction of the pains by the brutal plantar flexion, augmented by the percussion of the heel, and by the resisted contraction of the flexor of the I, the tendon of which passes between the posterior tubercles of the talus.
Complementary examinations:
• Standard radiographs of the profile, supplemented by plates in forced plantar flexion, objectify the local modifications, knowing the difficulties of interpretation of the bone images of the tail of the slope, the great individual variabilities of which are known;
• CT and arthroscanner are always very useful for studying posterior osseous changes and the possible existence of posterior cystic dilatation, which is a source of “ jamming “ and which may even contain foreign bodies. MRI can find its place here.
These examinations are all the more demonstrative because they are completed by images in flexion and, above all, extension.
The treatment:
• First and foremost “ medical “ by local infiltrations.
They must be very precise in their location and, as such, it is preferable to carry them under television control;
• only in case of failure, surgical excision of the lesions: soft parts and tail of the slope by arthroscopy or arthrotomy.
The tarsal sinus syndrome:
It should be remembered that the middle beam of the lateral (or fibulocalcanéen) collateral ligament is the true lateral ligament of the subtalian articulation, of which the hem ligament is the central element. As such, any severe lateral sprain of the ankle may result in lesions of the subtalar joint, more often painful than unstable syndrome.
Clinical signs of orientation:
They are deep back pain, especially when walking in irregular terrain and are particularly troublesome for changes of direction, reception of jumps, etc.
The examination finds pain in the lateral orifice of the sinus and in the mobilization of the articulation in pronosupination, moreover very often limited in its amplitudes.
Complementary examinations:
• Standard x-rays and even tomographies are totally powerless to explore this area properly;
• CT or MRI, on the other hand, made it possible to authenticate this syndrome by showing the local fibrosis embedding the whole sinus with sometimes ossifications;
• it must be added that a test infiltration has a determining value provided that it is carried out under a brightness amplifier because the diffusion to the two articular surfaces, anterior and posterior, is always random.
The treatment:
• It must first and foremost, if not exclusively, be “ medical “ by local infiltrations of corticoids in the sinus, under televised control, with very often very good results. The manipulations in axial decoaptation are particularly effective here, aided by the need for a stabilizing heel orthosis;
• surgery has very rare indications unless it is necessary to perform the removal of an ossification. . .
Some have proposed the curettage of the sinus but the indication can only be exceptional.
The pathologies of the fibular tendons:
They are far from being rare in the aftermath of an ankle sprain, whether it be recurrent dislocations or fissure syndromes.
Recurrent dislocations:
Too often the initial accident has passed unnoticed, interpreted as a mundane sprain, while knowing that fibular tendons can be associated with dislocation and dislocation.
Clinical signs of orientation:
The symptomatology consists of accidents which the patient recognizes as instabilities when the tendons come suddenly to place on the lateral face of the fibular malleolus during very brutal contractions during movements of forced inversion or explosive eversion, especially as pains accompany them.
But the examination reveals that all this symptomatology is retro-luminal and the clinical examination is revealing since it is known to search for the specific signs: reproduction of the dislocation during the upset eversion movements, especially if one exercises a backward pressure on the tendons.
Complementary examinations:
They are necessary only if one does not clinically reproduce dislocation:
• the contrastless frontal radiography sometimes shows a lateral-skeletal osseous scale, a sequela of a small osteoperiosis of the retinaculum which normally fixes the tendons. It is a pathognomonic sign of tendinous dislocation;
• ultrasound is the most effective examination because it allows a dynamic study and can specify the condition of the tendons;
• MRI shows dislocation only if it is permanent, but, like ultrasound, it has the advantage of specifying the anatomical state of the tendons, and in particular a possible fissure syndrome (see below).
The treatment :
It can only be surgical by retinaculum retension and reinsertion via transosseous points or better, now, by small bone anchors. If the retinaculum is dehiscent, it may be reconstructed by a small periosteal flap, which is rotated from the lateral malleolus. The excavation of the retro-lumbar gutter has very little interest and indication. Numerous artifices have been proposed in the literature but they have no place in practice (calcaneal tendon plasty or bone stops, for example).
Arthroscopic techniques have recently been proposed but require confirmation.
Fissure syndromes:
They are longitudinal lesions, more or less complete, cracking the tendons in one or several strips because of the repeated contacts between the tendons and the posterior margin of the lateral malleolus. The tendon of the fibular short, nearer to the posterior border, is most often reached.
These repeated contacts occur only on the occasion of dislocations (or subluxation) of the tendons or on accidents of instability due to chronic laxity.
Clinical signs of orientation:
Pain and lateral retromalleolar swelling dominate the picture, but there are often phenomena of instability when the strips are mobilized or the tendons become luxurious.
The examination finds all the signs behind the lateral malleolus.
Complementary examinations:
The additional examinations are as follows:
• standard radiographs, although still indispensable, are of no help here;
• ultrasound and MRI are the determining examinations (the tenoscanner has no place), showing perfectly the longitudinal divisions of the tendon (s). Depending on the extent of cracking, from simple flattening to complete cracking, Sobel et al. have defined four stages:
◦ stage I: simple flattening,
◦ stage II: non-translocating cracking,
◦ stage III: transfixing cracking,
Stage IV: dislocation of a strip or multiple cracks.
It may also be tenosynovitis reaching the fibular or the posterior tibial tendon.
The treatment :
Surgical treatment is justified, the only way to avoid the aggravation of lesions. It consists in suturing the strips or in excising a single strip and in making the retinaculum by reinsertion as described above.
The results are usually excellent.
Neurological sequelae:
They are too often neglected by ignorance. They may be sensory or motor, depending on the nervous trunk concerned.
The lesional mechanism is variable: either stretching by tensioning during the initial mechanism in inversion of the ankle, or compression at the level of an aponeurotic or canal passage.
The lesion can be juxta-articular or located at a distance (common fibular nerve in the neck of the fibula):
• the sensory sequelae are of interest to the superficial fibular nerve or to the posterior tibial nerve. They are responsible for dysesthesia and, sometimes, for objective disorders of sensibility;
• motor sequelae are rare and affect the territory of the common fibular nerve. The motor deficit they cause may be the sole cause of ankle instability.
This means that a neurological examination is necessary before any painful or unstable ankle.
Imaging here is of no help. The only necessary and necessary examination is the electromyogram.
The treatment depends on the symptomatology: the pure sensory forms can be treated by infiltration at the level of the compression in the aponeurotic procession or the ductal crossing. In the event of failure and whenever it is a motor deficit, surgical release is required as soon as possible. However, the results are often incomplete.
Apart: pain on tarsal synostoses
It is known that the synostoses of the tarsus, complete or incomplete (synchondroses), stiffening the hindfoot, are the cause of sprains since all the constraints are exerted on the lateral collateral ligament. So much so that in the adolescent, any ankle sprain must make them seek, whether it be a talocalcanéan synostosis or calcaneo-avicular synostosis.
However, in the aftermath of a sprain, they can become symptomatic, in the form of chronic pain and / or recurrent sprains.
Clinical signs of orientation:
• The clinical examination easily shows the stiffening of the talocalcanéan and / or talonavicular joints, especially since these synostoses are often bilateral. Attempts to mobilize are sometimes painful.
Complementary examinations:
• The standard radiographs, in the case of a talocalcaneal synostosis, show a pathognomonic sign on the profile: the sign of the wheel, dense and circular, totally erasing the subtalian spacing. In the case of a calcaneo-avicular synostosis, the oblique radiographs of the tarsus show the elongation of the calcaneal spout and its more or less complete sealing with the navicular bone;
• CT is however the indispensable examination to analyze exactly bone coalescence.
The treatment:
• in the adolescent, when it is symptomatic, the synostosis must be resected widely, with good results most often on the pain and the recurrence of the sprains, insofar as one restores mobility to the joints previously fixed;
• in adults, however, this hope is not allowed and surgery should be rejected. Only “ medical “ and orthotic means are recommended.
The “ unstable “ ankle:
We must repeat that instability and laxity are not synonymous: any “ unstable “ ankle is not “ lax “ and, conversely, any “ lax “ ankle is not unstable.
Indeed, it is unstable ankles without laxity, when the proprioceptive control is imperfect; for example, by failure of rehabilitation after a sprain. They relate only to the resumption of rehabilitation, in particular by work on an unstable plateau and muscular reinforcement of the stabilizing muscles, especially the fibular muscles. Recall also that acute pain can be interpreted by the patient as an instability.
On the contrary, there are genuine laxities without instability in patients with excellent muscular potential and very good proprioceptive control.
Finally, we must not ignore instabilities in the syndromes of joint hyperlaxity of which there are minor forms, especially in the young adolescent, which tend to improve at the end of growth, but also severe forms translating a real elastopathy .
This syndrome of hyperlaxity is easily observed because it also results in hyperextension of the metacarpophalangeal joints, hyperextension of the elbows, a genu recurvatum, in particular. In all these cases, surgical treatment should be considered only with extreme caution and, on the contrary, everything should be done to favor conservative treatment by re-education and the use of strapping for sporting activities, port of orthesis.
Only chronic ligament laxities will be considered.
Clinical signs of orientation:
• The interrogation accurately refers to the array of genuine sprains repeatedly. He must also reconstruct the history of the disturbances, their age, the treatments already carried out, not to mention the usual sports investigation. . .
• the clinical examination must begin with the inspection to record the axes of the lower limb and the hindfoot, knowing that a constitutional or acquired varus results in abnormal and high stresses on the ligamentous apparatus lateral of the ankle.
The lateral collateral ligament must be tested by the search for abnormal movements in varus and drawer, very easy to demonstrate at this stage of chronicity and outside any current or too recent trauma. This research must be comparative with the healthy side to eliminate any constitutional physiological laxity.
However, the examination must in any case be complete, with, for example, very careful palpation, study of joint amplitudes, examination of the subtalar joint and all the joints of the foot, and all the muscular and tendinous structures that may be interested (calcaneal tendons, anterior and posterior tibial, fibular, etc.), in search of associated pathologies.
Complementary examinations:
• Standard radiographs with the usual four clichés are always indispensable in first intention;
• ultrasound has become an essential examination to show the state of the lateral collateral ligament bundles and the level of their lesion, while at the same time allowing the study of the tendons around the ankle;
• X-rays in the forced position (frontal varus and anterior drag) have their full value, at a distance from a recent trauma, in contrast to acute lesions. They must be comparative in order to eliminate constitutional hyperlaxity.
They measure laxity. They are made manually, in autovarus or under mechanical stress (Telos ® );
• other examinations are often useful for finding a concomitant lesion (foreign body, lesion of the talian dome or lesions of the fibular tendons).
The treatment:
• It can only be surgical, since restraining by orthesis is difficult to envisage permanently, especially in young athletes.
Two types of plasties can be used:
• substitution ligamentoplasties, made from the peroneus brevis (short peroneal lateral) according to the techniques of Chrisman-Snook or, better, of Colville, more anatomical in respect of the paths of the anterior and middle beams.These two plasties use only half the tendon, so as not to deprive the foot of its action);
• ligamentous retension) with transosseous reinsertion through tunnels or bone anchors that fully respect the anatomy.If the ligamentous ligamentous tissue is of insufficient quality, the plasty may be reinforced by a periosteal flap or by a part of the ligamentary ligament (retinaculum of the extensors).
After the operation, the patient is immobilized in a resin boot for eight to 15 days, replaced by an orthesis until the sixth week, allowing partial support and the beginning of rehabilitation.
In the athlete, the plasties should be preferred by retensioning and reinsertion of the external ligamentous apparatus, possibly reinforced because they do not in any way alter the peroneus brevis, the sole stabilizing muscle of the ankle and therefore essential in the control of the ligament ‘inversion.
Before considering ligamentous plasty, it is necessary to have considered the examination of the axis of the hindfoot. It is clear that any significant varus is a contraindication to plasty as long as this varus has not been corrected. If the clinical examination shows this, the varus should be measured by a podometry knowing that the normal is at a valgus of 6 </s>.
In the case of a significant varus, correction is required by calcaneal osteotomy of valgisation associated or not, at the same time, with ligamentous plasty.
It should also be emphasized that any ligamentous plasty is excluded if there is a synostosis of the hindfoot.
Tibiotarsal osteoarthritis:
It is the ultimate complication of the lateral chronic laxities of the ankle, consequence of lateral sprains in inversion.
It is by no means a virtuality, but rather a real and far from exceptional complication justifying, if it is still needed, to treat carefully any recent sprain or to identify and treat in time all laxity chronic.
The osteoarthritic lesions sit on the supra-medial dome, resulting in a localized pinching of the articular line and hence a varus of the hindfoot under load. This only increases the risk of reversal instability, hence a true “ vicious circle “which can only go to aggravation).
We will only summarize signs and treatment because the framework of sports traumatology is now outdated.
Clinical signs of orientation:
• Diffuse, mechanical pain;
• joint effusion;
• joint laxity inversely proportional to progressive stiffness.
Complementary examinations:
• Standard X-rays under load are sufficient for diagnosis;
• other examinations are only available on a case-by-case basis, depending on specific factors or the need for additional information. As such, podometry allows to measure the importance of the deaxation and the CT to study the subtalian articulation. They are sometimes essential before considering treatment.
The treatment:
It can be “ medical “ at first and especially in minor forms. It rests on all the usual therapeutic arsenal to which we can validly add plantar orthoses of correction and now the viscosupplementation, but whose effectiveness can not yet prove.
Surgical treatment offers the choice between:
• talocurural arthrodesis;
• total ankle prosthesis.
Each technique has its advantages and disadvantages and only the case-by-case discussion and the precise information of the patient make it possible to choose the indication. But this question goes beyond the scope of this paper.