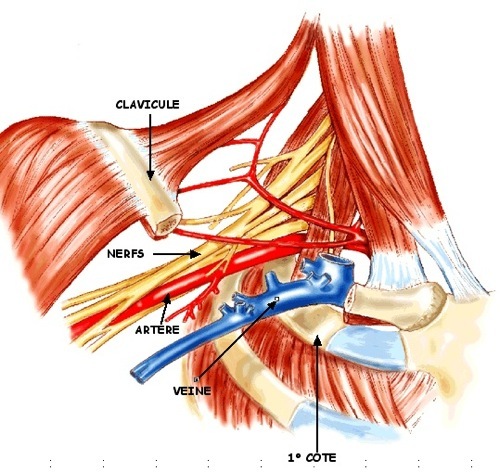
Thoracic outlet syndrome is the more or less complete association of irritation and / or compression of the vasculo-nervous pedicle of the upper limb as it passes through the scalene parade. the costo-clavicular defile and finally, behind the pectoral small muscle before the axillary space.
Thoracic outlet syndrome is the more or less complete association of irritation and / or compression of the vasculo-nervous pedicle of the upper limb as it passes through the scalene parade. the costo-clavicular defile and finally, behind the pectoral small muscle before the axillary space.
Depending on the level of compression, the clinical expression will be pure neurological or pure vascular (arterial and / or venous) or mixed.
The etiology:
The etiology of compression / irritation is often constitutional (supernumerary side, C7 apophysomegaly, fibrous tract …), but its association with an acquired favoring factor (muscle wasting, muscular hypertrophy, bone callus on fracture …), allows clinical expression more or less noisy.
In some cases, the subjects have a weak musculature with collapse of the shoulder belt and fall of the scapula or, on the other hand, hyperabuse work as in electricians or plasterers.
But the most frequent is the hypertrophy of the scalene in force workers (handling, carrying heavy loads …), workers with suspended shoulders (hairdressers, musicians, dentists …) or some sportsmen (swimming, handball, volleyball, ball, baseball, tennis …).
The prevalence of the syndrome is unknown in France and the variability of its clinical expression makes its diagnosis difficult. However, the increase of certain leisure activities (DIY, sport …) must make the clinician vigilant.
The clinic:
It is the most compressed element of the vasculo-nervous pedicle which will give the “tone” of the attack.
The disorders can be chronic and are most often dominated by neurological involvement involving C8-D1 (pain, paraesthesia) or frustrial radiculalgia, with episodes of edema or positional numbness.
More rarely, they can be noisy during “stress phlebitis” (subclavian venous thrombosis), which are extremely severe in cases of arterial ischaemia due to obliteration of the subclavian artery.
The clinical examination at rest, and especially during facilitation maneuvers, is the crucial time, emphasizing the systematic study of the two limbs.
The signs will depend on the age of the attack:
* predominant neurological involvement: pain caused by the supraclavicular trough, abolition of ROT, hypotrophy of the hypothenar eminence;
* predominant venous involvement: positional edema, presence of collateral venous circulation;
* predominant arterial involvement: auscultation of a susclavicular breath, abolition of one or more pulse, claudication, Raynaud’s phenomenon, or trophic nail disorders.
Positional maneuvers exacerbate the symptomatology by increasing the compression and sometimes allow to locate the level of the obstacle:
* Roos test: the appearance of paresthesias when the arms are held in abduction at 90 °, wrists in external rotation (“hands in the air”), before 3 minutes is highly evocative of a predominant neurological attack; the association of the disappearance of a pulse or of the appearance of a breath evokes an arterial component;
* Adson test: forced inspiration with head rotation of the suspect side contracts the scalenas or can mobilize a cervical rib;
* Wright’s maneuver: the complete elevation of the arm tends the pectoral;
* Sander maneuver: the position at attention closes the costo-clavicular forceps.
However, it should be borne in mind that the disappearance of a pulse has no specificity (50 to 70% of positive tests in the general population).
Complementary examinations:
After an interrogation and a good clinical examination, the complementary examinations are carried out at rest, but also during maneuvers of facilitations. They confirm the obstacle or its repercussion.
Cervical radiography:
The cervical radiography centered on C7 (+++): C7 apophysomegaly, supernumerary coast, bone callus.
The electromyogram:
The reduction of the nerve conduction velocities makes it possible to eliminate other differential diagnoses (carpal tunnel …). Some authors advocate the study of somaesthetic evoked potentials.
Doppler and / or echo-Doppler examination:
It must be systematically bilateral and symmetrical.
The use of a small convex probe with an emission frequency between 5 and 8 MHz is adapted to the study of the supraclavicular recess and the subclavicular space. The ideal is to place the probe under the clavicle and to orient it up and down. The vein and the artery passing between the clavicle at the top and the bottom at the bottom must be seen longitudinally (the two vessels are rarely seen at the same incidence).
The facilitation movements, carried out slowly, objectify the compression of the artery and / or the vein if necessary.
Venous compression is manifested by an almost complete reduction of its caliber (better visualized by the use of color Doppler), until the vein disappears.
Arterial compression is visible and audible. However, if the spectral analysis (peak of speeds greater than three times normal, filling of the clear window, envelope
irregular, turbulence until the permanent diastolic flow, or even complete abolition of the signal) confirms the stenosis or the dynamic obliteration, there are not strictly speaking velocimetric criteria determining a threshold of positivity since:
* the compression that can be visualized is frequent in the general population;
* there is no proportionality between the intensity of clinical symptoms and compression;
* the attack can be neurological without vascular participation!
At the stage of lesions formed, one can observe:
* at the arterial level: parietal thickening or localized plaque, or even a fusiform aneurysm with parietal thrombosis up to complete and old obliteration;
* at the venous level: constituted thrombosis or sequels with retraction, collateral circulation until the complete disappearance of the vein.
The scanner or MRI:
Without injection, they make it possible to demonstrate a compression of the vasculo-nervous pedicle, by the muscles or by a fibrous tract.
Angiography:
It uses mostly non-invasive means, in particular MRI, and allows visualizing the vascular effects of obstacles (arterial compression, venous compression, stenosis, obliteration, aneurism …).
In conclusion:
At the end of this assessment, the therapeutic indication is the result of a multidisciplinary confrontation (vascular physician, neurologist, rehabilitation worker, vascular surgeon …). In addition to complications requiring specific treatment (venous thrombosis, arterial ischemia, etc.), treatment involves either physiotherapy with postural rehabilitation (PEET) or surgery (resection of the rib or fibrous tract …).