Warning:
• The fungus Candida is a commensal gut but its presence in the mouth, vagina and on the skin is pathological.
• Contributing factors are: diabetes, obesity, estrogen plus progestin contraception, a systemic antibiotic treatment and immunosuppression (including HIV).
• A chronic pharyngeal and oral candidiasis in a young person has to suspect HIV seropositivity.
• If in doubt, mycological examination can be requested;growing very fast Candidaest (3 days).
Clinic:
Oral candidiasis: thrush.
Vaginal candidiasis: thick white discharge.
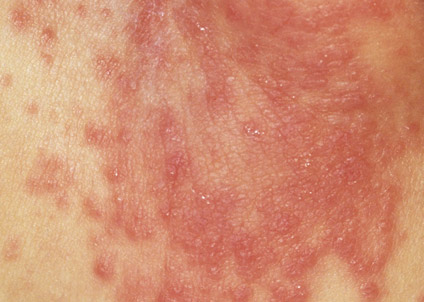
Candidiasis folds: intertrigo inguinal, axillary folds and submammary, thoroughly oozing and crumbled borders.
Treatment:
Order No. 1: vulvovaginal candida albicans vaginitis
– Toilet with vaginal HYDRALIN powder for local solution [sodium borate, sodium perborate, monosodium carbonate, anhydrous disodium carbonate] liquid soap, 1 sachet in 1 liter of water.
– GYNO Pevaryl LP-150 [éconazole], one egg at night, single dose.
Order No. 2 in case of recurrence
Cure 1 monthly for 2 months:
– GYNO-Pevaryl [econazole nitrate] egg (6 days).
Accompanied during the first cure:
– FUNGIZONE [amphotericin B] oral suspension, 1 teaspoon 3 times a day for 10 days.
No.3: oral candidiasis
– FUNGIZONE [amphotericin B] oral suspension,
– Infant and child, 1 teaspoon per 10 kg body weight per day in 2 to 3 doses
– For adults: 4 teaspoons per day in 2-3 doses for 2 to 3 weeks.
– If dentures: brushing with the oral suspension.
Ordinance No. 4: candidiasis sub-mammary fold
– Dry thoroughly after washing as needed with a hand dryer.
– Apply Pevaryl [econazole nitrate] powder or solution or DAKTARIN [miconazole] powder or Fazol[isoconazole] powder, 2 times a day on the lesions for 2 weeks.

You must be logged in to post a comment.