I – Introduction:
A- Definition of pulmonary embolism:
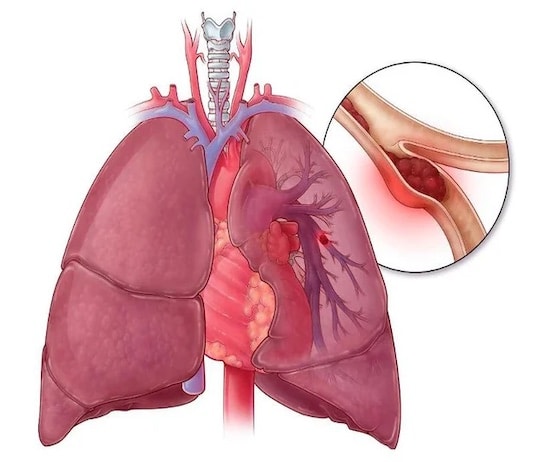
Pulmonary embolism is a potentially serious condition that occurs when a blood clot forms in a vein deep in the body and travels to the lung, thereby blocking part of the blood supply to the lung. This blockage can cause heart failure and respiratory failure and can be fatal if not treated quickly. The blood clots that cause a pulmonary embolism can come from anywhere in the body, but they often form in the legs. Most cases of pulmonary embolism are caused by deep vein thrombosis (DVT), which occurs when a clot forms in a deep vein. Risk factors for blood clots include advanced age, obesity, recent surgery, pregnancy, and taking certain medications.
B- Importance of understanding pulmonary embolism:
 Understanding pulmonary embolism is crucial because of its potential severity and the need for prompt treatment. A pulmonary embolism can be a life or death situation, as it can cause severe heart failure and respiratory failure. If a pulmonary embolism is not diagnosed and treated quickly, it can lead to serious complications, such as acute respiratory failure, cardiac arrest or even death. That’s why it’s important to know the symptoms of pulmonary embolism, understand the risk factors, and know how to prevent it. People at risk of developing a pulmonary embolism, such as those with heart disease or blood clotting disorders, should be particularly aware of the need for adequate prevention. Understanding pulmonary embolism can help avoid these potentially serious situations and save lives.
Understanding pulmonary embolism is crucial because of its potential severity and the need for prompt treatment. A pulmonary embolism can be a life or death situation, as it can cause severe heart failure and respiratory failure. If a pulmonary embolism is not diagnosed and treated quickly, it can lead to serious complications, such as acute respiratory failure, cardiac arrest or even death. That’s why it’s important to know the symptoms of pulmonary embolism, understand the risk factors, and know how to prevent it. People at risk of developing a pulmonary embolism, such as those with heart disease or blood clotting disorders, should be particularly aware of the need for adequate prevention. Understanding pulmonary embolism can help avoid these potentially serious situations and save lives.
C- Objectives of the article:
The goals of this article on pulmonary embolism are to provide complete and up-to-date information about this potentially serious condition, to educate readers about the risks of developing a pulmonary embolism, and to encourage prompt treatment if symptoms develop. This text also aims to help people at risk understand the risk factors and adopt healthy lifestyle habits to prevent the formation of blood clots. The article also aims to inform readers of the treatment options available for pulmonary embolism, including drug and surgical therapies. Finally, the article aims to encourage people with pulmonary embolism to pursue rigorous medical follow-up to prevent recurrences and ensure a full recovery. In sum,
II- Causes of pulmonary embolism:
A- Deep vein thrombosis:
Deep Vein Thrombosis (DVT) is a medical condition that occurs when a blood clot forms in a deep vein in the body, usually in the legs. This condition can cause severe pain and swelling and may increase the risk of developing a pulmonary embolism if the clot travels to the lungs. DVT is often associated with risk factors, such as advanced age, obesity, recent surgery, pregnancy, and taking certain medications. People with blood clotting disorders are also at higher risk of developing DVT. Treatment for DVT usually includes blood thinners to dissolve the clot and prevent new clots from forming. In some cases, surgery may be needed to remove the clot.
B- Paradoxical embolism:
Paradoxical embolism is a rare condition in which a blood clot from a deep vein travels through the atrial septum, a structure that separates the two parts of the heart, and enters the pulmonary bloodstream. This can cause pulmonary embolism, a potentially serious condition that can lead to heart failure and shock. People with blood clotting disorders or heart valve disease, such as mitral stenosis, are at higher risk of developing a paradoxical embolism. Symptoms include chest pain, shortness of breath, coughing up blood, and general weakness. Treatment for paradoxical embolism may include blood thinners to dissolve the clot, as well as treatments to address the underlying cause. In some cases, surgery may be needed to treat the underlying cause. It is important to consult a doctor as soon as symptoms of paradoxical embolism appear to ensure prompt and effective treatment.
C- Other less common causes:
In addition to deep vein thrombosis, there are other less common causes of pulmonary embolism. These include debris from endocarditis, which is an infection of the inner lining of the heart, fatty deposits that break off from the walls of arteries, and air or gas particles that can enter the bloodstream. Embolisms related to the use of drugs such as methamphetamine and crack are also a less common cause of pulmonary embolism. People with certain medical conditions such as rheumatoid arthritis and scleroderma are also at increased risk of pulmonary embolism. It is important to see a doctor if you have symptoms of pulmonary embolism, regardless of the underlying cause, in order to receive appropriate treatment.
III- Symptoms of pulmonary embolism:
A- Acute chest pain:
Acute chest pain is a common symptom of pulmonary embolism. It can look like angina pectoris or myocardial infarction and can feel like severe chest pain or chest tightness. Chest pain may be accompanied by other symptoms such as shortness of breath, coughing, excessive sweating, and heart palpitations. It is important to seek medical attention immediately if you experience sharp chest pain as this can be a sign of pulmonary embolism and can be life threatening if not treated promptly. Early diagnosis of pulmonary embolism can be made using a series of tests, including a chest x-ray, oxygen saturation detection test, and chest scan.
B- Sudden shortness of breath:
Sudden shortness of breath is another common symptom of pulmonary embolism. It can happen suddenly and can be described as difficulty breathing or rapid, shallow breathing. Shortness of breath may be accompanied by other symptoms such as chest pain, coughing, excessive sweating, and heart palpitations. It’s important not to ignore sudden shortness of breath and seek immediate medical attention if you experience it, as it can be a sign of pulmonary embolism and can be life-threatening if not treated quickly. Early diagnosis of pulmonary embolism can be made using a series of tests, including a chest x-ray, oxygen saturation detection test, and chest scan.
C- Cough with bloody sputum:
A cough with bloody sputum is a potential symptom of pulmonary embolism. However, it can also be caused by other conditions such as bronchitis, pneumonia, chronic obstructive pulmonary disease (COPD), or lung cancer. Cough with bloody sputum may be a sign of a bleeding lung injury and may indicate a serious pulmonary embolism. It is important not to ignore a cough with bloody sputum and seek immediate medical attention for prompt diagnosis and proper treatment. Diagnosis of pulmonary embolism can be made using a series of tests, including a chest x-ray, oxygen saturation detection test, and chest scan.
D- Other less common symptoms:
There are other less common symptoms that may be associated with pulmonary embolism. These may include dizziness, fatigue, fever, excessive sweating, nausea, vomiting, mental confusion, loss of consciousness, chest pain, and fear of dying . Although these symptoms are less common than symptoms such as sharp chest pain and sudden shortness of breath, they can still be signs of pulmonary embolism and should be taken seriously. If you experience any of these symptoms, it is important to seek medical attention immediately for prompt diagnosis and appropriate treatment. Diagnosis of pulmonary embolism can be made using a series of tests including a chest X-ray, an oxygen saturation detection test and a chest scan. Treatment for pulmonary embolism may include blood thinners to dissolve the clot, drugs to reduce blood pressure and pain, and hospitalization for observation.
IV- Diagnosis of pulmonary embolism:
A- Clinical examination:
Clinical examination is a key element in diagnosing pulmonary embolism. The doctor will perform a series of tests to assess symptoms, including breathing and heart rate. The doctor may also check the medical history to determine if the patient has any risk factors for pulmonary embolism, such as a history of deep vein thrombosis or other medical conditions. Additionally, the doctor may perform a complete physical exam, including an assessment of the skin and mucous membranes for signs of lack of oxygen, as well as an assessment of cough and sputum. Finally, the doctor may perform tests such as X-rays, scans, and blood tests to check lung function and the presence of blood clots.
B- Laboratory tests:
Laboratory tests can play an important role in the diagnosis of pulmonary embolism. Blood tests can be used to measure levels of certain substances that may be associated with pulmonary embolism, such as indicators of inflammation or abnormalities in blood clotting. The d-dimer test can also be done to detect the presence of substances in the blood that are generated when clots break down. Other blood tests may be used to assess liver and kidney function, as pulmonary embolism can lead to damage to these organs. Finally, blood tests can also help assess the effects of anticoagulant therapy and monitor reactions to these medications.
C- Imaging tests:
Imaging tests can play an important role in the diagnosis of pulmonary embolism. X-rays can help determine if the pulmonary embolism has caused swelling or cloudiness in the lungs. Computed tomography (CT) can be used to get more detailed images of the lungs and blood flow to detect the presence of blood clots. A lung scan can also be done to visualize blood flow in the lungs and determine if a clot is present. Finally, pulmonary angiography can be used to obtain images of blood vessels in the lungs to better understand blood flow and determine if a clot is present.
V- Treatment of pulmonary embolism:
A- Anticoagulant therapy:
Anticoagulant therapy is a common treatment for pulmonary embolism. It aims to reduce the formation of blood clots and prevent the growth of existing clots. Commonly used blood thinners include warfarin, dabigatran, apixaban, and rivaroxaban. These can be administered orally or by subcutaneous injection. Blood thinners can help prevent new blood clots from forming and reduce the size of existing ones. However, they can also increase the risk of bleeding, so it is important to carefully monitor the effects of these drugs. Finally, the duration of anticoagulant therapy may vary depending on the severity of the pulmonary embolism and the presence of other risk factors for thrombosis.
B- Thrombolytic therapy:
Thrombolytic therapy is a form of treatment for pulmonary embolism that aims to dissolve blood clots. It is often used in cases of severe pulmonary embolism or if the patient has severe symptoms. Commonly used thrombolytics include streptokinase, alteplase, and reteplase. These are given intravenously in a health care setting. Thrombolytics can help dissolve blood clots quickly and reduce symptoms associated with pulmonary embolism. However, this treatment also carries an increased risk of bleeding, especially in the brain. Accordingly, thrombolytic therapy should be administered with caution and under the supervision of a qualified physician. At the end of the day, the decision to treat with a thrombolytic will depend on the severity of the pulmonary embolism and the presence of other bleeding risk factors. Clot-busting therapy can help dissolve blood clots quickly and improve the chances of full recovery.
C- Surgical treatment:
Surgical treatment is an option for patients with severe pulmonary embolism who do not respond to other forms of treatment, such as anticoagulant therapy and thrombolysis. The most common surgical procedure to treat pulmonary embolism is clot filtration. During this procedure, a doctor removes the blocking clot by inserting a needle or catheter through the skin and into the affected vein. This treatment can be done in a minimally invasive way, reducing the risk of complications and scarring.
Other surgical procedures, such as pulmonary revascularization surgery and endarterectomy surgery, may also be used in severe cases of pulmonary embolism. However, these procedures are more invasive and carry an increased risk of complications. The choice of surgical treatment will depend on the severity of the pulmonary embolism and the presence of other risk factors. Ultimately, the decision for surgical treatment will be made in consultation with a qualified physician and will depend on each patient’s individual needs.
VI- Prevention of pulmonary embolism:
A- Modification of lifestyle habits:
Changing lifestyle habits is an important part of treating pulmonary embolism. People with pulmonary embolism are encouraged to adopt a healthier lifestyle to reduce the risk of a recurrence. This can include changes such as quitting smoking, eating a balanced diet, reducing stress, and exercising regularly. People with a blood clotting disorder are especially encouraged to watch their sugar and salt intake and to drink enough water.
It is also important to monitor medications that may increase the risk of pulmonary embolism. People taking hormone replacement medications, oral contraceptives, or growth medications are especially encouraged to talk to their doctor about changing or stopping these medications. People who are immobile for long periods, such as hospitalized patients, should be encouraged to exercise regularly and change positions frequently to reduce the risk of deep vein thrombosis.
In short, changing lifestyle habits can help prevent pulmonary embolism and improve the quality of life of those affected. It is important to speak with a doctor to develop a treatment plan that is suitable for each person.
B- Treatment of underlying conditions:
Treating the underlying conditions is a key part of treating pulmonary embolism. Conditions such as blood clotting disorders, heart disease, obesity and diabetes can increase the risk of pulmonary embolism. It is therefore important to treat these conditions to reduce the risk of recurrence.
Treatment for heart disease may include managing blood pressure, lowering cholesterol, taking medication to control palpitations, and treating atrial fibrillation. Treatment for obesity can include losing weight, adopting a healthy diet, and exercising regularly. Diabetes treatment may include controlling blood sugar, taking medication to control blood sugar, and adopting a healthy lifestyle.
It is also important to treat blood clotting disorders, such as thrombophilia, to reduce the risk of pulmonary embolism. This treatment may include taking blood-thinning medicines, such as warfarin or dabigatran, or changing the dose of these medicines to control blood clotting.
In sum, treatment of the underlying conditions is important for the prevention and treatment of pulmonary embolism. It is important to speak with a doctor to develop a personalized treatment plan for each person with pulmonary embolism.
C- Prevention of deep vein thrombosis:
The prevention of deep vein thrombosis is crucial to avoid the development of a pulmonary embolism. There are several simple steps people can take to reduce their risk of deep vein thrombosis, including adopting a healthy lifestyle, avoiding standing still for long periods of time, and wearing compression stockings when flying or flying. long car trips. It is also important to treat underlying medical conditions such as obesity, protein C and antithrombin III deficiency and to control blood clotting factor levels. Finally, blood-thinning medications can be used to prevent blood clots from forming in the deep veins.
VII- Conclusion:
A- Summary of key information:
Pulmonary embolism is a potentially serious condition in which a blood clot forms in a deep vein in the body and travels to the lungs, where it can block blood vessels and impede blood flow. Symptoms include sharp chest pain, sudden shortness of breath, and coughing up bloody sputum. Diagnosis is often made using clinical examination, laboratory tests, and imaging tests. Treatment for pulmonary embolism may include blood-thinning medications, thrombolytic therapy, or surgery. Changing lifestyle habits, treating underlying conditions, and preventing deep vein thrombosis can also help reduce the risk of developing a pulmonary embolism. At the end of the day,
B- Importance of prevention and rapid treatment of pulmonary embolism:
Pulmonary embolism is a potentially fatal condition that can cause irreparable damage to the lungs and other parts of the body if not treated quickly. This is why the prevention and prompt treatment of pulmonary embolism is extremely important. Risk factors may include a history of deep vein thrombosis, prolonged sedentary activity, underlying medical conditions such as obesity, and blood clotting disorders. It is therefore crucial to monitor the symptoms and seek prompt medical attention if a pulmonary embolism is suspected. Treatment may include blood-thinning medications, thrombolytic therapy, or surgery. Changing lifestyles, treating underlying conditions and preventing deep vein thrombosis can also help prevent the development of pulmonary embolism. Ultimately, an understanding of the importance of prevention and prompt treatment of pulmonary embolism can save lives.
C- Invitation to learn more about the prevention and treatment of pulmonary embolism:
Pulmonary embolism can be a serious and potentially fatal disease. This is why it is important to be informed about ways to prevent and treat this condition. In addition to following prevention tips such as regular exercise, healthy eating, and stress management, it is also important to seek medical attention immediately if symptoms such as sharp chest pain, sudden shortness of breath, or cough with bloody sputum occur. Prompt treatment can help reduce the risk of serious complications and improve the chances of full recovery. If you want to learn more about the prevention and treatment of pulmonary embolism, please talk to your doctor or consult reliable resources online or at local libraries.
Leave a Reply