I – Introduction:
A- Brief definition of diverticulitis:
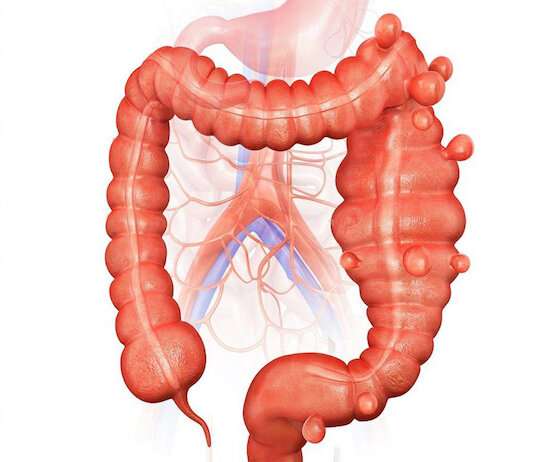
Diverticulitis is inflammation of the diverticula, which are small pockets that form in the wall of the colon. These diverticula are often caused by increased pressure on the wall of the colon, usually due to a low fiber diet. Over time, these pockets can fill with feces and bacteria, causing painful inflammation. Symptoms of diverticulitis include severe abdominal pain, often concentrated on the left side of the abdomen, as well as fever, nausea, and vomiting. If left untreated, diverticulitis can cause serious complications, including bowel perforation, peritonitis, and sepsis. People with diverticulosis, a common condition characterized by the presence of diverticula in the colon, are more likely to develop diverticulitis. Early diagnosis and proper treatment can help prevent life-threatening complications from this condition.
B- Importance of the article to raise public awareness about diverticulitis:
 It is important to educate the public about diverticulitis because it is an increasingly common condition, especially among the elderly. Symptoms can be very painful and can have a significant impact on the quality of life of sufferers. Additionally, diverticulitis can cause serious complications, including bowel perforation and peritonitis, which can be life-threatening. Treating diverticulitis can also be expensive and require surgery, which always carries risks. Therefore, it is essential that people are informed about the prevention of diverticulitis and about the signs and symptoms of this disease, so that they can detect it early and prevent complications. This includes changes in diet, regular exercise and maintaining a healthy weight. Ultimately, this article is important because it provides valuable information about diverticulitis that can help people take the necessary steps to prevent this condition and maintain their gut health.
It is important to educate the public about diverticulitis because it is an increasingly common condition, especially among the elderly. Symptoms can be very painful and can have a significant impact on the quality of life of sufferers. Additionally, diverticulitis can cause serious complications, including bowel perforation and peritonitis, which can be life-threatening. Treating diverticulitis can also be expensive and require surgery, which always carries risks. Therefore, it is essential that people are informed about the prevention of diverticulitis and about the signs and symptoms of this disease, so that they can detect it early and prevent complications. This includes changes in diet, regular exercise and maintaining a healthy weight. Ultimately, this article is important because it provides valuable information about diverticulitis that can help people take the necessary steps to prevent this condition and maintain their gut health.
II- Causes of diverticulitis:
A- Explanation of what a diverticulum is and how it forms:
A diverticulum is a small pocket that forms in the wall of the colon. It is usually caused by increased pressure on the wall of the colon, often due to a low fiber diet. Fiber helps increase stool bulk and consistency, making it easier to pass through the colon. When one lacks fiber in one’s diet, it can cause the intestinal muscles to contract too much, which can increase the pressure on the colon wall. This pressure can cause weakness in the wall, which can lead to the formation of small sacs or diverticula. Diverticula can form at any time in life, but are more common in people over 40. They are often asymptomatic and do not require treatment. However, in some people, diverticula can become inflamed, causing severe pain and other symptoms. In this case, medical treatment is necessary to relieve inflammation and prevent potential complications.
B- Risk factors for diverticulitis:
Several factors can increase the risk of developing diverticulitis. The main risk factor is age, as diverticula are more common in people over the age of 40. A diet low in fiber may also increase the risk of diverticulitis, as fiber helps prevent constipation by increasing stool bulk and consistency. Other risk factors include being overweight or obese, lack of exercise, smoking, and taking medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids. A family history of diverticulitis can also increase the risk of developing this condition. People with certain diseases, such as Crohn’s disease, are also more likely to develop diverticula and diverticulitis. Finally, women are more likely to develop diverticulitis than men. It is important to understand the risk factors for diverticulitis in order to take the necessary steps to prevent this condition and maintain optimal intestinal health. This may include diet changes, regular exercise and weight management.
1- Age:
Age is one of the main risk factors for diverticulitis. Diverticula are more common in people over the age of 40, and their frequency increases with age. This may be due to several factors, including reduced physical activity, decreased dietary fiber intake, decreased gut muscle tone, and decreased immune system efficiency. As we age, the muscles in the bowel can also become weaker, which can make it harder to pass stool, which can increase pressure on the wall of the bowel and promote the formation of diverticula. It is important to emphasize that age is not a modifiable risk factor,
2- Diet:
Diet is an important factor in the development of diverticulitis. A diet low in dietary fiber is one of the main risk factors for this condition. Dietary fiber is important for maintaining colon health because it increases the bulk and consistency of stool, making it easier to pass. In contrast, a diet low in fiber can lead to constipation, increase pressure on the wall of the intestine, promote the formation of diverticula, and contribute to the development of diverticulitis. Fiber-rich foods include fruits, vegetables, legumes, whole grains, and nuts. Processed foods high in fats and sugars can also contribute to inflammation of the colon lining, thus increasing the risk of developing diverticulitis. It is therefore recommended to follow a healthy and balanced diet, high in fiber and low in processed foods, to prevent diverticula and reduce the risk of developing diverticulitis. In case of diagnosed diverticulitis, it is recommended to follow a specific diet to relieve inflammation and prevent complications.
C- Other potential causes of diverticulitis:
Although age and diet are the main risk factors for diverticulitis, other potential causes can contribute to its development. For example, an obstruction or blockage in the intestine can lead to inflammation of the lining of the colon, leading to diverticulitis. Ingested foreign bodies, such as fruit pits or seeds, can also block the colon and promote the formation of diverticula. Intestinal motility disorders, such as irritable bowel syndrome, can also contribute to the formation of diverticula. Also, inflammatory bowel diseases, such as Crohn’s disease, can increase the risk of diverticulitis. Bacterial infections of the gut can also contribute to the development of diverticulitis. Finally, certain medications, such as steroids, can weaken the lining of the intestine and increase the risk of diverticulitis. Understanding these other potential causes of diverticulitis is important to taking steps to prevent this condition and maintain optimal gut health.
1- Infections:
Bacterial infections are a common cause of diverticulitis. Diverticula are pockets in the wall of the colon, which can become inflamed when infected with bacteria. Infections can occur when feces get trapped in the diverticula, which can lead to bacterial overgrowth. Symptoms of infectious diverticulitis can include fever, abdominal pain, nausea, vomiting, and changes in bowel habits. Diverticulitis infections can be treated with antibiotics, which help kill the bacteria causing the infection. It is important to quickly diagnose and treat diverticulitis infections, because complications such as perforation of the colon or abscess formation can occur if the infection is not treated. To reduce the risk of diverticulitis infections, it is important to eat a diet high in fiber, stay well hydrated, and maintain good bowel hygiene.
2- Inflammatory bowel diseases:
Inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis, can increase the risk of diverticulitis. People with these diseases have chronic inflammation of the intestine, which can cause damage to the lining of the colon. These lesions can promote the formation of diverticula, increasing the risk of diverticulitis. Symptoms of diverticulitis in people with inflammatory bowel disease can be more severe and harder to treat. Managing inflammatory bowel disease through proper diet, regular exercise, and medication can help prevent the development of diverticulitis. People with these conditions should consult their doctor for advice on preventing diverticulitis and treating the symptoms of diverticulitis if it occurs. Also, people with inflammatory bowel disease should have regular checkups to screen for diverticula, as early detection and treatment of diverticulitis can help prevent complications.
III- Symptoms of diverticulitis:
A- Typical symptoms of diverticulitis:
Typical symptoms of diverticulitis include severe abdominal pain, often concentrated in the left lower quadrant of the abdomen, fever, nausea, vomiting, loss of appetite, and changes in bowel habits, such as diarrhea or constipation. Abdominal pain may be constant or intermittent and may be exacerbated by palpation or pressure on the affected area. Symptoms can be similar to those of other bowel diseases, such as bowel infections or colic, but the pain from diverticulitis can be more intense and more localized. In severe cases, diverticulitis can lead to complications such as perforation of the colon, formation of abscesses or fistulas, which can cause bleeding or generalized infections, endangering the patient’s life. It is therefore important to consult a doctor quickly if symptoms of diverticulitis appear. Early diagnosis and proper treatment can help prevent serious complications and relieve symptoms of diverticulitis.
1- Abdominal pain:
Abdominal pain is one of the most common symptoms of many diseases, including diverticulitis. Abdominal pain can manifest in different ways, ranging from mild, dull pain to intense, sharp pain. The location of the pain can also vary depending on the underlying cause. In the case of diverticulitis, abdominal pain is often localized in the lower left quadrant of the abdomen, but it can also be felt in other parts of the abdomen. The pain may be constant or intermittent and may be exacerbated by certain movements or actions, such as palpation or pressure on the affected area. If abdominal pain is accompanied by other symptoms such as fever, nausea, vomiting, loss of appetite or changes in bowel habits, it is important to seek medical attention promptly. Early diagnosis and proper treatment can help relieve abdominal pain and prevent potentially serious complications associated with diverticulitis.
2- Fever and nausea:
Fever and nausea are two common symptoms associated with diverticulitis. Fever is a normal body response to infection and can indicate severe inflammation. In the case of diverticulitis, fever can occur in response to inflammation and infection in the affected area. The fever can be mild or severe and is often accompanied by a general feeling of being unwell. Nausea is an uneasy feeling in the stomach that may be accompanied by vomiting. Nausea can be caused by inflammation and infection occurring in the affected area, as well as medications that are used to treat diverticulitis. The combination of fever and nausea can make the patient very uncomfortable and disrupt quality of life.
B- Less common symptoms of diverticulitis:
Besides common symptoms such as abdominal pain, fever, and nausea, there are also less common symptoms associated with diverticulitis. These symptoms can vary in intensity and frequency from patient to patient, but they can all indicate inflammation and infection in the affected area. Less common symptoms of diverticulitis may include bloating, gas, constipation or diarrhea, burning sensation or pain when urinating, chills, tiredness or weakness, loss of appetite, loss of unintentional weight loss, joint and muscle pain, and rectal bleeding. If you experience any of these symptoms in addition to the common symptoms of diverticulitis, it is important to seek prompt medical attention for proper diagnosis and treatment. Early identification and treatment of diverticulitis can help prevent potentially serious complications associated with the disease.
1- Diarrhea:
Diarrhea is a less common symptom of diverticulitis, but it can occur in some patients. Diarrhea is characterized by an increase in the frequency and quantity of stools, which may be loose or watery. Diarrhea can be caused by inflammation and infection in the affected area, which can disrupt the normal digestion of food. Antibiotics used to treat diverticulitis can also upset the balance of beneficial bacteria in the gut, which can lead to diarrhea. Diarrhea may be accompanied by other symptoms, such as abdominal pain, bloating, gas, and nausea. It’s important to stay hydrated if you have diarrhea, as excessive fluid loss can lead to dehydration.
2- Constipation:
Constipation is another less common symptom of diverticulitis that can occur in some patients. Constipation is characterized by hard, dry, difficult-to-pass stools, and can be caused by a buildup of feces in the colon. Diverticula can make constipation worse by reducing the colon’s ability to contract and push feces through the digestive system. Constipation can be accompanied by other symptoms, such as abdominal pain, bloating, gas, and nausea. It is important to drink plenty of fluids and eat fiber-rich foods to prevent constipation. Laxatives can also help relieve constipation, but it’s important to talk to a doctor before using them. as they may not be suitable for all patients with diverticulitis. If constipation persists or is accompanied by severe abdominal pain, blood in the stool, or vomiting, it is important to see a doctor for proper diagnosis and treatment.
C- Differences between the symptoms of diverticulitis and those of other intestinal disorders:
It can be difficult to differentiate the symptoms of diverticulitis from those of other bowel conditions because many diseases have similar symptoms. For example, Crohn’s disease, ulcerative colitis, and acute appendicitis can all cause abdominal pain, fever, and nausea, which are also common symptoms of diverticulitis. However, there are a few key differences to consider. For example, diverticulitis is often associated with localized pain in the lower left abdomen, while acute appendicitis is often associated with localized pain in the lower right abdomen. Additionally, Crohn’s disease and ulcerative colitis can cause rectal bleeding and bloody diarrhea, which are less common symptoms of diverticulitis. If you have symptoms of diverticulitis, it is important to see a doctor for an accurate diagnosis. Your doctor may perform a physical exam, blood test, and imaging tests to determine the cause of your symptoms and recommend the appropriate treatment.
IV- Diagnosis of diverticulitis:
A- Examinations and tests used to diagnose diverticulitis:
To diagnose diverticulitis, the doctor may perform several examinations and tests. First, the doctor will start with a physical exam to check for signs of abdominal pain, fever, nausea, and other symptoms of diverticulitis. Then blood tests may be done to check for signs of infection, such as an increased white blood cell count. Imaging tests may also be used to aid in the diagnosis of diverticulitis. Magnetic resonance imaging (MRI) and computed tomography (CT) are two of the most commonly used tests. These tests can help detect inflammation, diverticula, and other abnormalities in the colon and intestines. In some cases, a colonoscopy may be recommended to help confirm the diagnosis and rule out other bowel conditions. If you have symptoms of diverticulitis, it is important to see a doctor for an accurate diagnosis. Early diagnosis and proper treatment can help avoid serious complications and relieve symptoms.
1- Computed tomography (CT):
Computed tomography (CT) is a medical imaging technique that uses X-rays to produce detailed images of the inside of the body. It is one of the most common tests used to diagnose diverticulitis. During a CT scan, the patient lies on a table that slides into a donut-shaped scanner. The scanner sends X-rays through the body, which are picked up by detectors on the other side. A computer analyzes the data and produces detailed three-dimensional images of the inside of the body, including the intestines and colon. CT can help detect inflammation, diverticula, and other abnormalities in the colon and intestines. It is also useful for assessing the extent of infection and possible complications. Although CT is generally safe, it involves exposure to x-rays, so it’s important to discuss the risks and benefits of this test with your doctor before having it. Overall, CT is a valuable tool for diagnosing diverticulitis and helping to plan the appropriate treatment.
2- Endoscopy:
Endoscopy is a medical imaging technique that allows doctors to view the inside of the digestive tract, including the colon and intestines, using a thin, flexible instrument called an endoscope. It is a useful test for diagnosing diverticulitis and for assessing the extent of inflammation and infection. During an endoscopy, the patient lies on their side and an endoscope is inserted into the anus. The doctor can then visualize the walls of the colon and intestines and take tissue samples for laboratory analysis. Endoscopy can also be used to detect and remove polyps, which are abnormal growths in the intestinal walls. Endoscopy can be uncomfortable, but is generally well tolerated with mild sedation. As with any medical test, there are risks associated with endoscopy, including bleeding and intestinal perforation, but these risks are rare. Overall, endoscopy is a valuable tool for diagnosing diverticulitis and helping plan the appropriate treatment.
B- Potential complications of diverticulitis:
Diverticulitis can lead to potentially serious complications if not treated quickly and correctly. Common complications of diverticulitis include abscess formation and peritonitis, which is inflammation of the lining of the abdomen that can spread to other organs. Patients with diverticulitis may also develop intestinal obstruction, intestinal fistula, intestinal bleeding, or generalized infection. Complications can be avoided or minimized by seeking treatment as soon as symptoms of diverticulitis appear. Complications of diverticulitis can be treated with a combination of drugs, antibiotics, and surgery. In severe cases, surgery may be needed to remove the damaged or infected part of the intestine. It is important to follow your doctor’s advice to reduce the risk of complications and recover faster.
1- Intestinal perforation:
Diverticulitis can lead to perforation of the intestine, which is a potentially dangerous complication. Perforation occurs when the inflammation associated with diverticulitis damages the intestinal wall, causing feces to leak into the abdominal cavity. This can lead to a serious infection in the abdomen called peritonitis. Symptoms of bowel perforation include severe abdominal pain, fever, nausea, and vomiting. If bowel perforation is suspected, emergency surgery is often needed to repair the damage and prevent the infection from spreading. Treatment may involve removing the damaged part of the bowel or creating a temporary colostomy to allow the bowel to heal.
2- Peritonitis:
Peritonitis is a serious infection of the abdominal cavity that can occur as a complication of untreated or poorly treated diverticulitis. This condition can occur when bacteria present in feces leaking from a perforated diverticulum spreads into the abdominal cavity, causing inflammation. Symptoms of peritonitis include severe abdominal pain, fever, nausea and vomiting, and a tender, tender abdomen. Peritonitis is a medical emergency that requires emergency surgery to remove accumulated fecal matter and pus from the abdominal cavity, as well as to repair damage to the bowel. Patients with peritonitis must be hospitalized and given intravenous antibiotics to fight the infection. Although peritonitis can be a serious and life-threatening complication of diverticulitis, early diagnosis and prompt treatment can reduce the risk of long-term complications and improve patient outcomes.
V- Treatment of diverticulitis :
A- Treatment options for diverticulitis:
The treatment for diverticulitis depends on the severity of the disease. For mild cases, home treatment may be sufficient, with antibiotics to fight infection, a gentle diet, rest, and painkillers to relieve pain. For more serious cases, hospitalization may be necessary to administer intravenous antibiotics, for better medical monitoring and for the establishment of intravenous feeding. In some cases, surgery may be needed to remove the affected part of the colon. This procedure, called a colectomy, is usually used for severe cases of diverticulitis that do not respond to other forms of treatment or for patients who develop complications. Patients may also be encouraged to make lifestyle changes, such as eating a high fiber diet and exercising regularly, to prevent future attacks of diverticulitis. The choice of treatment depends on each individual case and should be discussed with a healthcare professional.
1- Antibiotics:
Antibiotics are a common treatment for uncomplicated diverticulitis. They are usually prescribed for seven to ten days and are effective in reducing inflammation and infection. The types of antibiotics used depend on the severity of the infection, the patient’s medical history, and other factors such as drug allergies. Common side effects of antibiotics include upset stomach, diarrhea, and rash. Patients must take the antibiotics exactly as prescribed and complete the full course to prevent the infection from coming back. In more severe cases, intravenous antibiotics may be given in the hospital for a longer period. Antibiotics aren’t always needed in cases of mild diverticulitis or when symptoms go away quickly without treatment. In some cases, doctors may recommend surgery to prevent recurrences of diverticulitis.
2- Dietary changes:
Diet is an important aspect of treating diverticulitis. Dietary changes can help relieve symptoms and prevent future attacks. Doctors often recommend increasing fiber intake to improve gut health. Fiber helps soften stools and prevent constipation, which can reduce pressure on diverticula. Fiber-rich foods include fruits, vegetables, whole grains, and legumes. It is also recommended that you drink enough water to help soften the stool and make it easier to pass. However, it is important not to increase fiber intake suddenly, as this can cause bloating and gas. Dietary changes can also include avoiding foods that can trigger or worsen symptoms, such as fried foods, dairy products, spicy foods, and alcoholic beverages. A dietitian can help develop an appropriate eating plan for patients with diverticulitis.
B- Surgery for diverticulitis:
Surgery may be recommended for people with complicated or recurring diverticulitis. The surgery involves the removal of the affected part of the colon, called a colectomy, and can be performed openly or laparoscopically. The laparoscopic procedure is generally preferred as it is less invasive and allows for faster recovery. In some cases, a temporary colostomy may be needed to allow the colon to heal properly. Risks associated with diverticulitis surgery include anesthesia-related complications, bleeding, infections, anastomotic leaks, and fistulas. It’s important to discuss the potential benefits and risks of surgery with your doctor to decide if it’s the best treatment option for each individual case. After surgery, it may be recommended to follow a specific diet to help prevent the recurrence of diverticula.
1- Indications for surgery:
In some cases of diverticulitis, surgery may be necessary. Indications for surgery include complications such as peritonitis, intestinal perforation, stenosis, abscesses and fistulas. Other factors to consider may include a history of recurrent diverticulitis, persistent symptoms despite medical treatment, poor quality of life due to symptoms, or an increased risk of complications due to an underlying disease such as Crohn’s disease. The type of surgery will depend on the severity of the disease and the location of the diverticula. In some cases, a partial or total colectomy may be necessary. Patients undergoing surgery for diverticulitis can expect a variable recovery period depending on the specific procedure and their overall health. It is important for patients to discuss the risks and benefits of surgery with their doctor to decide on the best treatment option for them.
2- Different surgical procedures available:
There are several surgical options to treat diverticulitis, depending on the severity of the disease and the general health of the patient. The most common surgery is sigmoid resection, which involves removing the part of the colon affected by diverticulitis. This procedure can be performed using laparoscopy, a minimally invasive surgical technique that uses small incisions in the abdomen and a camera to view inside the abdominal cavity. In the most severe cases of diverticulitis, a colostomy may be necessary. This procedure involves creating an opening in the abdomen to allow stool to pass into an external sac, rather than through the anus. This may be temporary or permanent, depending on the extent of the disease and the colon’s ability to heal. In general, surgery is considered a treatment option for patients with recurrent diverticulitis, severe complications, or advanced disease that does not respond to other treatments. The pros and cons of each option should be discussed with a healthcare professional to determine the best course of treatment for each patient.
VI- Prevention of diverticulitis:
A- Tips to prevent diverticulitis:
Although some causes of diverticulitis, such as age and genetics, cannot be changed, there are steps people can take to reduce their risk of developing this condition. One of the most effective ways to prevent diverticulitis is to eat a healthy, fiber-rich diet. Fiber-rich foods include vegetables, fruits, whole grains, and legumes. It’s also important to drink enough water and stay active to help maintain regular bowel movements. Avoiding tobacco and limiting alcohol consumption can also help reduce the risk of developing diverticulitis. Finally, it is important to discuss any gastrointestinal symptoms with your doctor, because early diagnosis and treatment can help prevent the progression of diverticulitis. By taking care of your body and being alert to the signs of diverticulitis, it is possible to prevent or limit the symptoms of this condition.
1- Eat a fiber-rich diet:
Eating a high fiber diet is one of the most common tips for preventing diverticulitis. Fiber is a type of carbohydrate that the body cannot digest, but is essential for digestive health. Fiber helps regulate bowel movements and prevent constipation, which can reduce pressure on the intestinal walls and thus reduce the risk of diverticula. Fiber-rich foods include fruits, vegetables, whole grains, legumes, and nuts. It is recommended to consume at least 25 grams of fiber per day for women and 38 grams for men. However, it is important to gradually increase the amount of fiber in the diet to avoid bloating and abdominal pain. Moreover, it is important to drink enough water to allow fiber to work well in the gut. Eating a high-fiber diet can not only help prevent diverticulitis, but also help maintain good digestive health in general.
2- Exercising regularly:
Exercising regularly has many physical and mental health benefits. Physical benefits include improved cardiovascular health, weight loss, increased muscle strength and endurance, improved bone health, and reduced risk of certain chronic diseases, such as type 1 diabetes. 2, high blood pressure and certain types of cancer. The mental benefits of exercise include reduced stress, anxiety, and depression, as well as improved mood and sleep quality. For optimal health benefits, it is recommended that you engage in moderate to vigorous intensity exercise for at least 150 minutes per week. This can be achieved through a combination of aerobic activities and muscle strengthening. It’s important to choose activities you enjoy and start slowly to avoid injury. With regular practice, exercise can help improve quality of life and prevent chronic disease.
B- How people with diverticulosis can prevent diverticulitis:
Diverticulosis is a condition where pockets (diverticula) form in the wall of the colon. Although diverticulosis is usually not serious, it can lead to complications such as diverticulitis, an inflammation of a diverticulum. To prevent diverticulitis, people with diverticulosis should eat a diet high in fiber. Fiber is essential for maintaining regular bowel movements and preventing constipation, which can increase pressure in the colon and make diverticulosis worse. Fiber-rich foods include fruits, vegetables, legumes, and whole grains. People with diverticulosis should also drink enough water to help maintain soft, easy-to-pass stools. Moreover, regular exercise is recommended to maintain a healthy digestive system. Finally, it is important to see a doctor regularly to monitor the progress of diverticulosis and discuss any concerns or symptoms.
C- Summary of the most effective preventive measures for diverticulitis:
There are several effective preventive measures to prevent diverticulitis and its complications. First of all, it is recommended to adopt a diet rich in fiber, consisting of fruits, vegetables, legumes and whole grains. Fiber helps maintain regular bowel movements, thus preventing constipation which can increase pressure in the colon and worsen diverticulitis. Drinking enough water to maintain soft, easy-to-pass stools is also important. Regular exercise can help maintain a healthy digestive system and prevent diverticulitis. Also, it is important to see a doctor regularly to monitor the progress of diverticulosis and discuss any concerns or symptoms. Avoid processed and fatty foods reducing alcohol consumption and not smoking are also important preventive measures. Finally, people with diverticulosis should avoid medications that can irritate the colon and cause inflammation, such as nonsteroidal anti-inflammatory drugs (NSAIDs).
VII- Conclusion:
A- Summary of the main points of the article:
Diverticulitis is a condition that occurs when pockets called diverticula form in the lining of the colon and become inflamed or infected. Symptoms of diverticulitis include severe abdominal pain, fever, nausea, and vomiting. Risk factors for diverticulitis include aging, lack of fiber in the diet, obesity, smoking, and taking certain medications. Common diagnostic tests include urinalysis, X-rays, CT scans, and colonoscopy. Drug treatments for diverticulitis include antibiotics, antispasmodics, and painkillers. In cases of severe or recurring diverticulitis, surgery may be necessary.
B- Importance of preventing diverticulitis:
Preventing diverticulitis is important because it can help reduce the risk of serious complications and improve the quality of life for people with this condition. By making healthy lifestyle changes such as a high-fiber diet, adequate hydration, and regular physical activity, people with diverticulosis can prevent the formation of diverticula and reduce the risk of developing diverticulitis. Additionally, by avoiding risk factors such as smoking, obesity, and taking medications that increase the risk of diverticulitis, people can improve their digestive health and reduce their risk of other colon-related health problems. Finally, by regularly consulting a doctor and carrying out appropriate screening examinations,
C- Call to action to seek medical attention if symptoms of diverticulitis are present:
It is important to see a doctor as soon as symptoms of diverticulitis are present. Symptoms such as abdominal pain, nausea and vomiting, changes in bowel habits, and fever may indicate inflammation or infection of the diverticula. Without proper treatment, this can lead to serious complications such as peritonitis, fistula, stenosis or bowel obstruction. People with a family history of diverticulitis, the elderly, and people with medical conditions such as Crohn’s disease or irritable bowel syndrome are particularly at risk. It is therefore essential to consult a doctor as soon as symptoms are present for early diagnosis and treatment, which can help prevent serious complications and improve quality of life. Ultimately, it’s important to take care of your digestive health by adopting a healthy lifestyle and monitoring signs and symptoms to catch any abnormalities early and act quickly to treat them.
Leave a Reply