* The diagnosis should be considered in any acute or sub-acute pain of the spine with segmental stiffness and a fortiori associated fever or an inflammatory syndrome.
* Plain x-rays may be normal at the beginning justifying the action, in emergencies, MRI.
* Germ Research is essential -> disc biopsy (if bacteriological investigation after removal of the front door and blood culture is negative).
* Two peaks in frequency: adolescence and goshawks 60 years. In the majority of cases, the distribution is done through blood. Staphylococcus aureus is responsible for over 50% of non-tuberculous SD;
* The spine is the most common bone localization of brucellosis (mainly lumbar). Lumbar location is the most frequent and including L4-L5 disc. the spondylitis is multifocal in 10% of cases.
* For SD tuberculous, the dorsal and lumbar locations are the most frequent. multifocal disease (more than two spinal segments) in 23% of cases.
* Any febrile acute back pain should suggest the diagnosis; the pain is gradually; it is intense, permanent inflammatory schedule with nighttime awakenings; it can be associated with radicular pain (sciatica, femoral neuropathy). Fever is inconstant; AEG sometimes with major weight loss in over half the cases. The pain may be trivial, mechanical schedule …
* The gradual and insidious onset is common in tuberculous SD
* A moderate or absent inflammatory syndrome (biology) does not rule out the diagnosis. The leukocytosis is inconstant. Neutropenia can suggest the diagnosis of Brucella SD; moderate lymphopenia can be observed.
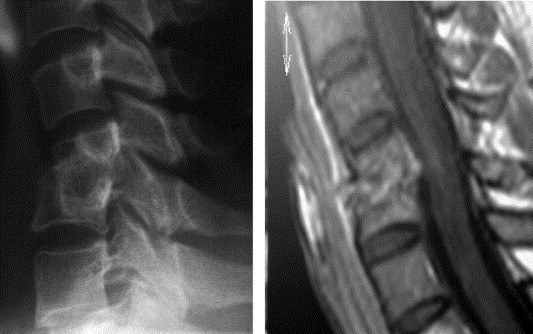
* Plain radiographs (first in prescribe) are often normal at first; because there is a delay in relation to clinical signs (2-3 weeks for commonplace germs and 4 to 6 weeks for tuberculosis).
RADIOLOGY:
– The first signs of erosion of the anterior area of the two adjacent vertebrae reached disk and the reduction of the height of the intervertebral disc (most constant sign).
– More belatedly appear uneven and erosions of the vertebral endplates aspect, geodes intrasomatiques and sometimes vertebral osteolysis -> cuneiform or global collapse of the vertebra with mostly the posterior wall compliance.
– Some time in dorsal paravertebral images and blurry and convexity in the lumbar psoas edge can testify to the presence of abscesses périrachidiens
– Some signs of reconstruction are often early, especially in brucellosis (multiple lap of osteolysis and osteophytes turn the disc)
– The open geodes in the disc, arranged mostly in mirror are the most typical (but not more frequently) of tuberculosis. Auseins bone receivers of these geodes are also very evocative of BK. Other signs (in favor of BK): spondylitis with respect discs; achievement of the posterior arch.
* Paraspinal abscesses are common (50-70% of cases) in infectious spondylitis tuberculous and are readily bilateral and bulky.
* CT is less effective than MRI
* Scintigraphy (technetium) is positive early before X-rays with intense uptake at the site of infection. But it is not very specific.
* Note: the disc involvement is common in the spondyloarthropathies, rarer in rheumatoid arthritis. MRI images are characterized by the absence of signal on T2.
* Treatment is essentially medical; it combines effective antibiotic treatment and immobilization. The indications for surgery are rare.
* Antibiotics: Treatment of attack for 2 to 4 weeks (bi-parenteral antibiotic) -> oral monotherapy for 2 to 3 months (banal germs).
* Bed rest is required until disappearance of pain; then lift with progressive port lombostat (corset) for 3 to 4 weeks.

Leave a Reply